Abstract
Purpose
Inguinoscrotal sarcomas are exceedingly rare tumors. The aim of this study was to enable clinicians an easy and rapid access to the available information on this tumor entity.
Methods
An updated series of 21 men treated for sarcoma of the inguinoscrotal region at our institution between 1992 and 2012 was analyzed, and a systematic review of the literature with meta-analysis of outcome data was performed. The review was focused on demographic data, survival rates, prognostic factors, sites of relapse and complete remissions or successful treatments for metastatic disease.
Results
With only 38 %, the proportion of high-grade tumors in our sample was lower than reported in the literature and the 10-year relapse-free, disease-specific and overall survival rates were favorable with 77, 93 and 81 %. Beside our series, twelve studies including 345 patients were identified in the literature. The weighed mean 10-year relapse-free, disease-specific and overall survival rates were 63, 64 and 50 %. Only in patients with rhabdomyosarcoma, durable control of metastatic disease has been reported in more than one case (n = 4). Successful treatment in these cases consisted of a combination of complete surgical resection of metastatic lesions, subsequent chemotherapy and (optional) radiotherapy.
Conclusions
Overall, about two-thirds of inguinoscrotal sarcomas may be cured. In series with a predominance of low-grade tumors, the long-term survival rates in completely excised inguinoscrotal sarcomas may be as favorable as in testicular germ cell tumors. Life-long surveillance is advisable to detect late recurrences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although representing the most frequent urological soft tissue malignancies in adults [1], inguinoscrotal sarcomas are exceedingly rare. In a multicentric study, eight Italian institutions collected less than ten cases during a 19-year period [2]. Due to the rarity of these tumors, only sparse outcome information is available [1, 3, 4]. Clinicians interested in treatment and outcome details are confronted with scattered and heterogeneous reports of small sample sizes. Finding and reviewing these studies may be difficult and time-consuming. In this study, we analyzed our patients with tumors of the inguinoscrotal region treated during two decades and performed a systematic review of the literature with special attention to disease control and survival rates in order to enable clinicians an easy and rapid access to the available information on this rare tumor entity.
Patients and methods
Patient sample
A total of 21 men older than 16 years (range 32–84) who underwent surgical treatment for primary (n = 19) or locally recurrent (n = 2) sarcomas of the inguinoscrotal region at our institution between 1992 and 2012 were studied. Institutional review board approval was obtained. The patients were identified by a review of collected histopathological reports. The tumor grade (high vs. low) was assigned according to the Hajdu grading system based on histopathological type, cellularity, stromal content, necrosis, maturation and mitotic activity [5]. The majority of patients studied have already been subject to two earlier analyses [6, 7]. No patient was lost to follow-up. Death was attributed to sarcoma if there was uncontrolled recurrent disease at the time of death.
Primary treatment consisted of radical excision of the primary or locally recurrent tumor. After resection of the primary tumor, four patients received adjuvant radiotherapy, one retroperitoneal lymph node dissection. Treatment for recurrent disease was (if necessary repeated) surgical removal, combined with local radiotherapy. Metastatic disease was repeatedly removed in one patient partially by multivisceral resection and adjuvant radiotherapy (high-grade leiomyosarcoma [7]), treated by radiotherapy resulting in durable disease control (low-grade myxoid malignant fibrous histiocytoma [7]) and radiotherapy and chemotherapy (high-grade rhabdomyosarcoma; the latter patient died of disease 18 years after removal of the primary tumor).
Systematic review of the literature
The systematic review of the literature was performed oriented on criteria suggested by Galfano and Novara [8] for systematic reviews of randomized trials. Two internet-based data sources were used: the PubMed database of the National Institute of Health (website: http://www.ncbi.nlm.nih.gov/sites/entrez/) and the Web of Knowledge databases of Thompson Reuters (website: http://apps.webofknowledge.com). Journal articles were considered when they fulfilled the following criteria: unselected series (i.e. not restricted to one entity like rhabdomyosarcoma or liposarcoma); reporting more than five sarcomas arising in the inguinoscrotal region in adult males; written in English language; published in the years 1970–2012 (including electronic publications ahead of print). Meeting abstracts and book chapters were not considered. Studies including patients younger than 16 years or female patients were excluded, with the exception of studies with tabular patient data enabling a separate analysis of adult male patients. The excluded studies were cited in the results section to ease future search activities by others. When more than one report analyzing the same patient sample was published, the most recent one reporting outcome data was included.
The key word combinations and the number of retrieved articles are shown in Table 1. If headline and abstract were suggestive of potential fulfilling the search criteria, the full text version was studied. Finally, the reference sections of all full text articles cited in this article were reviewed for possible further suitable studies. Questions relevant for treatment planning and outcome prediction have been formulated prior to the literature search. Except from the separately recorded distribution of histopathological subtypes, these questions constituted the headlines of the columns in Tables 2 and 3.
Statistical analysis
Kaplan–Meier method was used to determine overall survival, whereas competing risk analysis was used to determine recurrence-free and disease-specific survival both in our patient sample and in three patient samples reported in the literature [9, 11, 12] in which analyzable tabular outcome data were given. Recurrence-free and disease-specific survival rates after 5 and 10 years were calculated by subtracting the incidence rates obtained by competing risk analysis from 100 %. Comparisons of variables were made with the log rank and the Pepe-Mori tests, respectively. A meta-analysis of the recurrence-free, disease-specific and overall survival rates of the single studies was performed by weighing the corresponding rates by the number of patients in the beginning of follow-up. The statistical analyses were performed with the Statistical Analysis Systems (SAS Institute, Cary, NC) statistical package.
Results
The mean tumor diameter was 6.2 cm (range 1.7–15). Further demographic data are shown in Table 2. Recurrence-free survival, disease-specific survival and overall survival rates are shown in Fig. 1. None of the investigated variables (age: below median vs. older, tumor size: below 5 cm vs. greater, subtype: liposarcoma vs. other, grade: low vs. high, margin status: negative vs. positive, adjuvant radiotherapy: yes vs. no) were significant predictors of overall and disease-specific survival in our series.
The results of the systematic review of the literature are shown in Tables 2 and 3. Five studies were excluded from the review because they included pediatric cases [2, 3, 23–25] and three because they included female patients [26–28]. Two studies containing pediatric cases but reporting separately analyzable tabular patient data enabling a separate analysis of adult sarcomas were included in the review [9, 11]. In one of these studies [11], beside two pediatric cases, one case of mesothelioma was excluded from our re-analysis.
The mean (or median) age in the included studies ranged between 44 and 62 years, the sample sizes between 6 and 156. Three samples from the United States were larger than the present series: a Surveillance, Epidemiology, and End Results database query for patients diagnosed with primary scrotal cancer between 1973 and 2006 (n = 156) [19], one of the Memorial Sloan Kettering Cancer Center (n = 47) [1] and one of the M. D. Anderson Cancer Center (n = 32) [18]. The recruitment periods varied between 7 and 38 years.
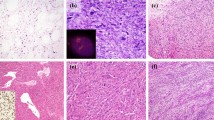
All but one study [19] provided histopathological details. Overall, with 31 % of cases, liposarcoma was the most common subtype, followed by leiomyosarcoma (27 %), malignant fibrous histiocytoma (17 %), rhabdomyosarcoma (13 %) and other types (12 %). The proportion of high-grade tumors ranged until 100 % and was lowest in our series (38 %).
Metastatic disease was durably controlled in 10 patients, at least four of them had rhabdomyosarcoma (three embryonal subtype and one pleomorphic) [1, 12], one malignant fibrous histiocytoma, one leiomyosarcoma (our series; Table 3); in four further cases, no histopathology details were reported [1, 14].
The sites of recurrence have to be considered with the qualification that it was not always unequivocally stated whether patients with local recurrence later developed distant relapse as well. Local and distant recurrences have been reported with similar frequency. Of patients with distant recurrence, less than half had pelvic, abdominal or retroperitoneal involvement, isolated retroperitoneal recurrence was an exception (Table 3). The latest relapse was observed after 132 months, the latest sarcoma-related death after 216 months. Only one of the studies identified a prognostic factor (complete resection [1]). The role of prophylactic retroperitoneal lymph node dissection was controversially discussed. There were six statements merely pro-retroperitoneal lymph node dissection [1, 10–12, 15], two merely contra [14, 18], in four studies a neutral or no statement was given [9, 13, 17, 19].
Discussion
Although reporting was heterogeneous, satisfactory information could be derived from the articles identified by the systematic review of the literature, particularly from studies providing tabular details on patient histories [9–12]. Such data presentation enabling later combined analyses should be encouraged for small reports of rare diseases.
Identifying prognostic factors in inguinoscrotal sarcomas is difficult because of the small sample sizes. The only reported parameter complete excision [1] is certainly a presupposition for successful treatment. Although disease grade has not been identified as prognostic factor, most likely because of limited statistical power due to small sample sizes and—as in our sample—too few observed events, the great clinical importance of this factor is underlined by the distinctly favorable outcome of our series with predominantly low-grade sarcomas (relative 5-year survival 106 %) resembling that of testicular germ cell tumors (relative 5-year survival 96 % [29]). Nevertheless, metastatic disease may occur and was associated with dismal outcome with few exceptions. Apparently, multimodal treatment was most likely successful when metastatic disease had rhabdomyosarcoma histopathology (Table 3). Successful treatment regimens for metastatic adult inguinoscrotal rhabdomyosarcoma consisted of a combination of complete surgical resection of metastatic foci with subsequent chemotherapy (in three out of four cases doxorubicin-based [1, 12]), optionally combined with radiotherapy [1]. Durable control of metastatic spread of other inguinoscrotal sarcoma subtypes has been documented only in single cases not allowing general conclusions. Only a minority of distant disease recurrences were restricted to areas which may be cleared by retroperitoneal lymph node dissection (Table 3). It is impossible to estimate whether routine retroperitoneal lymph node dissection would have been able to prevent these recurrences, in the majority of cases probably not. In individual cases of the above-mentioned rhabdomyosarcomas (Table 3), durable disease control was achieved by retroperitoneal lymph node dissection with removal of single positive nodes followed by chemotherapy [12]. These observations and the general susceptibility of rhabdomyosarcoma to chemotherapy support routine retroperitoneal lymph node dissection in this subtype. Altogether, there are still uncertainties on the role of retroperitoneal lymph node dissection in inguinoscrotal sarcomas reflected by the conflicting statements in the studies identified during systematic literature review.
Considering the histopathological subtypes (most common subtype liposarcoma followed by leiomyosarcoma and malignant fibrous histiocytoma) and the age at diagnosis (Table 2), inguinoscrotal sarcomas had demographic similarity with sarcomas of retroperitoneal origin (in a series of 500 cases, the same sequence of the most common subtypes and a median age of 58 year were observed [30]).
In all studies providing long-term outcome data, disease recurrences after more than 5 years of follow-up were observed, once even after more than 10 years [18]. Disease-related deaths may occur later than 10 years after diagnosis (Table 2). These data suggest a need for life-long follow-up in this rare tumor entity.
This study has several limitations. The systematic review of the literature was restricted to unselected series of inguinoscrotal sarcomas. Case series of distinct histopathological entities or single case reports were not included. Such types of publications could contain information on clinical course and treatment that may not be found in unselected studies, and could, however, introduce a selection bias by over-reporting of single cases with favorable outcome. Without access to the original data or the standard errors of the majority of studies identified by the systematic literature search, only a weighing of survival rates by the sample sizes was possible as meta-analysis. The resulting figures should be interpreted with this qualification. Including relatively old patient series may be associated with uncertainties in tumor classification, and the disease management might have differed from contemporary standards.
Conclusions
Overall, about two-thirds of inguinoscrotal sarcomas may be cured. In series with predominance of low-grade tumors, the long-term survival rates in completely excised inguinoscrotal sarcomas may be as favorable as in testicular germ cell tumors. In individual cases, mainly in rhabdomyosarcomas, metastatic disease may be controlled by multimodal treatment. In the latter subtype, prophylactic retroperitoneal lymph node dissection could be beneficial. Life-long surveillance is advisable to detect late recurrences.
References
Coleman J, Brennan MF, Alektiar K, Russo P (2003) Adult spermatic cord sarcomas: management and results. Ann Surg Oncol 10:669–675
Mondaini N, Palli D, Saieva C, Mondaini N, Palli D, Saieva C, Nesi G, Franchi A, Ponchietti R, Tripodi S, Miracco C, Meliani E, Carini M, Livi L, Zanna I, Trovarelli S, Marino V, Vignolini G, Pomara G, Orlando V, Giubilei G, Selli C, Rizzo M (2005) Clinical characteristics and overall survival in genitourinary sarcomas treated with curative intent: a multicenter study. Eur Urol 47:468–473
Hazariwala R, Morris CG, Gilbert S, Algood C, Zlotecki RA (2012) Radiotherapy for spermatic cord sarcoma. Am J Clin Oncol [Epub ahead of print]
Rodríguez D, Olumi AF (2012) Management of spermatic cord tumors: a rare urologic malignancy. Ther Adv Urol 4:325–334
Hajdu SI (1979) Pathology of soft tissue tumors. Lea & Febiger, Philadelphia, pp. 44–45
Froehner M, Lossnitzer A, Manseck A, Koch R, Noack B, Wirth MP (2000) Favorable long-term outcome in adult genitourinary low-grade sarcoma. Urology 56:373–377
Froehner M, Schober RR, Koch R, Lossnitzer A, Laniado M, Wirth MP (2011) Adult urologic sarcoma: Experience during 2 decades. Urol Oncol [Epub ahead of print]
Galfano A, Novara G (2008) Methodological bases for systematic reviews. J Androl Sci 15:185–193
Bhargava MK (1976) Paratesticular tumours of mesenchymal origin. Indian J Cancer 13:108–122
Sogani PC, Grabstald H, Whitmore WF Jr (1978) Spermatic cord sarcoma in adults. J Urol 120:301–305
Blitzer PH, Dosoretz DE, Proppe KH, Shipley WU (1981) Treatment of malignant tumors of the spermatic cord: a study of 10 cases and a review of the literature. J Urol 126:611–614
Catton CN, Cummings BJ, Fornasier V, O’Sullivan B, Quirt I, Warr D (1991) Adult paratesticular sarcomas: a review of 21 cases. J Urol 146:342–345
Rao CR, Srinivasulu M, Naresh KN, Doval DC, Hazarika D (1994) Adult paratesticular sarcomas: a report of eight cases. J Surg Oncol 56:89–93
Fagundes MA, Zietman AL, Althausen AF, Coen JJ, Shipley WU (1996) The management of spermatic cord sarcoma. Cancer 77:1873–1876
Berkmen F, Celebioğlu AS (1997) Adult genitourinary sarcomas: a report of seventeen cases and review of the literature. J Exp Clin Cancer Res 16:45–48
Merimsky O, Terrier P, Bonvalot S, Le Pechoux C, Delord JP, Le Cesne A (1999) Spermatic cord sarcoma in adults. Acta Oncol 38:635–638
Catton C, Jewett M, O’Sullivan B, Kandel R (1999) Paratesticular sarcoma: failure patterns after definitive local therapy. J Urol 161:1844–1847
Ballo MT, Zagars GK, Pisters PW, Feig BW, Patel SR, von Eschenbach AC (2001) Spermatic cord sarcoma: outcome, patterns of failure and management. J Urol 166:1306–1310
Johnson TV, Hsiao W, Delman KA, Canter DJ, Master VA (2013) Scrotal cancer survival is influenced by histology: a SEER study. World J Urol 31:585–590
Russo P, Brady MS, Conlon K, Hajdu SI, Fair WR, Herr HW, Brennan MF (1992) Adult urological sarcoma. J Urol 147:1032–1037
Dotan ZA, Tal R, Golijanin D, Snyder ME, Antonescu C, Brennan MF, Russo P (2006) Adult genitourinary sarcoma: the 25-year Memorial Sloan-Kettering experience. J Urol 176:2033–2038
Wright JL, Morgan TM, Lin DW (2008) Primary scrotal cancer: disease characteristics and increasing incidence. Urology 72:1139–1143
Malek RS, Utz DC, Farrow GM (1972) Malignant tumors of the spermatic cord. Cancer 39:1108–1113
Soosay GN, Parkinson MC, Paradinas J, Fisher C (1996) Paratesticular sarcomas revisited: a review of cases in the British Testicular Tumour Panel and Registry. Br J Urol 77:143–146
Korkes F, Castro MG, Romero FR, Godoy G, Amary MF, Fernandes RC, Perez MD (2009) Paratesticular sarcomas in Brazil. Urol Int 82:448–452
Mack LA, Temple WJ, DeHaas WG, Schachar N, Morris DG, Kurien E (2004) Groin soft tissue tumors–a challenge for local control and reconstruction: a prospective cohort analysis. J Surg Oncol 86:147–151
Brooks AD, Bowne WB, Delgado R, Leung DH, Woodruff J, Lewis JJ, Brennan MF (2001) Soft tissue sarcomas of the groin: diagnosis, management, and prognosis. J Am Coll Surg 193:130–136
Collin T, Blackburn AV, Milner RH, Gerrand C, Ragbir M (2010) Sarcomas in the groin and inguinal canal—often missed and difficult to manage. Ann R Coll Surg Engl 92:326–329
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
Lewis JJ, Leung D, Woodruff JM, Brennan MF (1998) Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 228:355–365
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Froehner, M., Koch, R., Lossnitzer, A. et al. Adult inguinoscrotal sarcomas: outcome analysis of 21 cases, systematic review of the literature and meta-analysis. World J Urol 32, 445–451 (2014). https://doi.org/10.1007/s00345-013-1124-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1124-1