Abstract
Purpose
To explore the risk factors, prevention, and management of the septic shock following the mini-percutaneous nephrolithotripsy (mini-PCNL).
Methods
A total of 834 consecutive patients who underwent mini-PCNL from June 2004 to April 2012 were retrospectively analyzed. The causes, prevention, and treatment of septic shock following mini-PCNL were assessed.
Results
Twenty out of 834 patients developed septic shock, and 17 patients recovered without complications. Three patients progressed to multiple organ dysfunction syndromes and expired. Multivariable analysis showed that the following variables were independently related to septic shock following mini-PCNL: female, with an odds ratio (OR = 1.055E8, P < 0.001) and diabetes mellitus (OR = 4.192, P = 0.001).
Conclusion
Female and diabetes mellitus are the risk factors for septic shock following mini-PCNL. Perioperative preventive measures can reduce the incidence of septic shock. Early recognition and timely bundle treatment may decrease the mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Using a smaller size percutaneous tract than standard percutaneous nephrolithotomy (PCNL), minimally invasive PCNL (mini-PCNL) has the potential advantage of decreasing bleeding and trauma to renal parenchyma but the disadvantage of needing longer operative time to dislodge stones. Septic shock after PCNL has a low reported incidence that ranges from 0.3 to 1 % but a high mortality (66–80 %) [1]. To limit morbidity and mortality, it is crucial to identify the risk factors of septic shock, prompt diagnosis, and provide multidisciplinary treatment. However, evidence-based guidelines in the prevention and treatment of septic shock following mini-PCNL are lacking. Our study sought to identify the factors associated with septic shock following mini-PCNL and assess the optimal prevention and management.
Patients and methods
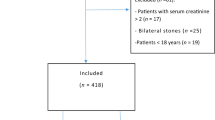
We have retrospectively analyzed the clinical characteristics of 834 consecutive patients who underwent mini-PCNL from June 2004 to April 2012 at our department of urology. The inclusion criteria were single tract procedure performed on a unilateral kidney. Patients who had double tract procedure, solitary kidney, and separate procedures on bilateral stones were excluded from this study. All patients received a single dose of antibiotic prophylaxis (second- or third-generation cephalosporin) before mini-PCNL. For the patients whose urine culture tests were positive, broad-spectrum antibiotics were administrated for at least 2 weeks or until their urine culture tests became negative.
Operations were all performed by three experienced urologists. Dilatation of the nephrostomy tract was performed with fascial dilators until an 18-Fr Amplatz sheath was inserted. An 8/9.8F ureteroscope was used in combination with holmium laser lithotripsy for stone disintegration in all cases. A 5-Fr double-J catheter and a 16-Fr nephrostomy tube were placed at the end of each procedure. Postoperatively intravenous antibiotics were routinely administered for 24 h or until patients remained afebrile.
Diagnostic criteria of septic shock were [2, 3]: (1) proven bacteraemia or clinical suspicion of sepsis; (2) systemic inflammatory response syndrome (SIRS) diagnosed by meeting two or more of the following four criteria including body temperature ≥38 or ≤36 °C, tachycardia ≥90 beats min−1, tachypnoea ≥20 breaths min−1 or respiratory alkalosis with a PaCO2 ≤32 mmHg, leukocytes ≥12,000 μL−1 or ≤4,000 μL−1 or bandforms >10 %; and (3) refractory hypotension with a systolic blood pressure ≤90 mmHg.
If septic shock is recognized, therapy was started parenterally according to a careful evidence-based methodology in the recently published ‘Surviving Sepsis Guidelines’ [2, 3]. The protocolized resuscitation of a patient should be initiated as soon as hypoperfusion is recognized and should not be delayed pending ICU admission. During the first 6 h of resuscitation, the goals of initial resuscitation should include all of the following as one part of a treatment protocol: central venous pressure, 8–12 mmHg; mean arterial pressure (MAP) ≥65 mmHg; urine output ≥0.5 mL kg−1 h−1; central venous (superior vena cava) or mixed venous oxygen saturation ≥70 or ≥65 %, respectively. If it is not achieved with fluid resuscitation to the central venous pressure target, then transfusion of packed red blood cells to achieve a hematocrit of ≥30 % and/or administration of a dobutamine infusion can be used to achieve this goal.
Intravenous antibiotic therapy should be started as early as possible and within the first hour of recognition of septic shock and severe sepsis without septic shock. Appropriate cultures should be obtained before initiating antibiotic therapy but should not prevent prompt administration of antimicrobial therapy. Carbapenems (imipenem or meropenem) were used for initial empirical anti-infective therapy based upon the expected bacterial spectrum, the local susceptibility patterns. We recommend that the duration of therapy typically be 7–10 days or determined by the patient’s clinical response.
Statistics analysis
Clinical characters were reviewed, Chi-square test and logistic regression analysis were used for statistical analysis in the SPSS software, and P < 0.05 was considered statistically significant (Tables 1, 2).
Results
Twenty out of 834 patients developed septic shock, and 17 patients recovered without complications. Three patients progressed to multiple organ dysfunction syndromes (MODS) and expired. Multivariable analysis showed that the following variables were independently related to post-mini-PCNL septic shock: female, with an odds ratio (OR of 1.055E8, P < 0.001), and diabetes mellitus (OR = 4.192, P = 0.001). Surgical site, history of hypertension, history of urinary tract infection, preoperative serum creatinine, history of stone surgery, size of stone, positive urine culture, length of the procedure, and age were not significantly correlated with septic shock following mini-PCNL (Tables 1, 2).
Discussion
Although the definitions used vary, septic shock rates following PCNL have been reported to be 0.3–1 % [1]. It is triggered when, during percutaneous nephrolithotomy, stone manipulation produces an intense liberation of bacteria and endotoxins, and their products enter the blood stream via pyelovenous-lymphatic and pyelotubular backflow and forniceal rupture [4]. We performed PCNL using an 18-French percutaneous working tracts. Technically, recent studies [5–7] revealed that mini-PCNL has the potential advantage of decreasing the risk of bleeding and tearing of the renal cortex but the disadvantage of needing longer time to dislodge stones than the standard PCNL. We demonstrated the risk factors for septic shock following mini-PCNL and the optimal prevention and management of the complication.
Preoperative predictors and preparation
The high-risk factors for septic shock includes positive urine culture, female gender, renal insufficiency, high pressure of irrigation fluid during PCNL, staghorn calculus, preoperative nephrostomy, diabetes, infected stones, indwelling catheters, obstruction, and duration of the operation [8–11]. In our study, two major risk factors identified are diabetes mellitus and female, which were consistent with the literatures. All the patients had septic shock in our study were female. Several studies have shown that most patients with sepsis following percutaneous or endoscopic procedures for urinary tract stones were female [12, 13]. Diabetes mellitus was identified as another independent risk factor for septic shock in our study. Cellular and humoral immune in diabetics are well known to be impaired. Therefore, strict control of blood glucose should be achieved to prevent septic shock in patients who have diabetes or hyperglycemia with a target blood glucose level of 8.3 mmol/L [2].
In addition to female and diabetes, the rate of septic shock was numerically higher in the larger stone (size ≥2 cm) group and in the preexisting urinary tract infections group. But the association between preexisting urinary tract infections and stone size with the development of septic shock was on the edge of being statistically significant, maybe due to the relatively limited sample size. In agreement with prior studies [8, 14], septic shock is correlated with preexisting urinary tract infections and stone size.
Although it is generally agreed that patients who are scheduled for PCNL must have a negative urine culture before surgery [1], severe sepsis still occurs in patients with sterile urine. Mariappan et al. [15] showed that a standard urine culture has a rather low predictive value for an infectious complication and that a direct culture of the renal pelvis and stone culture are better predictors of infection. The present findings [9] indicate that the antibiotic prophylaxis of patients undergoing PCNL with a negative baseline urine culture is associated with a significant reduction in the rate of postoperative fever. Reduction in the risk of urinary tract infection [14] by preoperative urine culture and appropriate antibiotic therapy and prophylaxis in patients with sterile urine are key preventive measures for sepsis. But antibiotic prophylaxis [8] fails to completely eliminate the risk of septic shock following mini-PCNL as one of the methods in preventing the complication. This probably reflects the liberation of bacteria and endotoxins in the interstices of the stone, which triggers a systemic inflammatory response.
Therefore, septic shock following PCNL is impossible to be predicted preoperatively with certainty. High-risk patients even with negative urine culture may need preoperative antibiotics at least 1 week before the planned procedure.
Intraoperative predictors and management
On occasion, during renal puncture, purulent urine may be unexpectedly encountered. Smith et al. [1, 16, 17] suggested to leave a nephrostomy tube in place and defer the procedure until the infection is treated and the upper tract is confirmed sterile.
Zhong et al. [18] demonstrated that mean intrapelvic pressure >20 mmHg may cause enough backflow, resulting in bacterial and endotoxin translocation into the systemic circulation, and the small tract in mini-PCNL might result in high pressure in the collecting system, which would cause pyelovenous or pyelosinus backflow, resulting in postoperative fever. In the case of torquing a rigid endoscope against the pelvicalyceal system to get to an inaccessible calyx, a temporarily elevated renal pelvic pressure may occur on the conditions that restrict irrigation outflow from the interspace between endoscope and peel-away sheath, such as the peel-away sheath is compressed and stone fragments enter into the interspace between the scope and peel-away sheath. The small tract in mini-PCNL might result in longer operation time and higher pressure in the collecting system. However, recent studies have demonstrated that the renal pelvic pressure remained lower during mini-PCNL [19, 20]. Low intrapelvic pressure is achieved using an open low-pressure access system (operating instrument 4F sizes smaller than the access sheath), inflow of irrigant should be at gravity, and is never pressurized [21]. Though the drawback of mini-PCNL is the longer operative time, it has no significant correlation with septic shock following mini-PCNL in our study. The key point to control intrapelvic pressure is to minimize the infusion pump pressure, keep the peel-away sheath smooth, and wash fragmentation in sheath promptly.
Postoperative care
Septic shock frequently occurs within the first 6 h of the stone-related surgery [13, 16]. To diagnose septic shock as early as possible, patients suspected should be prioritized and receive timely care in the postoperative period. The clinical picture of a septic patient frequently, but not always, involves warm skin, bounding pulses, and hyperdynamic circulation. If the patient is hypovolemic, has preexisting myocardial dysfunction, or is at late stage of the septic process, hypotension, vasoconstriction, and peripheral cyanosis may be present [14]. The doctor should rapidly check the criteria for the diagnosis of sepsis, in order to initiate further investigations.
If septic shock is the putative diagnosis, the best strategy has been summarized and graded according to a careful evidence-based methodology in the recently published ‘Surviving Sepsis Guidelines’ [2]. Appropriate therapy is a continuum of management of infection ranging from drainage (opening the nephrostomy tube) and empirical broad-spectrum antibiotics to aggressive fluid resuscitation and invasive monitoring with medical management in the intensive care setting until the causative agent is found and eradicated [21].
We recommend that intravenous antibiotic therapy should be started as early as possible and within the first hour. Initial empirical anti-infective therapy includes one or more drugs that have activity against all likely pathogens. Usual causes derived from urinary sources are aerobic gram-negative bacilli and enterococci. Empirical antibiotic therapy, therefore, needs to follow certain rules, which are based upon the expected bacterial spectrum, the local susceptibility patterns [14].
If septic shock is recognized, besides empiric antibiotic therapy, prompt treatment in the intensive care unit should include initial resuscitation with large amounts of crystalloid intravenous fluids. Adjunctive sepsis therapy such as cardiovascular support, mechanical ventilation, organ substitution, or management of endocrine insufficiency should be instigated if warranted [2]. Bicarbonate and low-dose steroids may be used and maintain good blood glucose control. Applying these standards to our septic patients will substantially reduce the mortality.
In our study, there are 3 patients progressed to MODS and expired, all with various degree of intraoperative blood loss, with hemoglobin dropped to 51–76 g L−1 and leukocytes <1,000 μL−1. Septic shock along with hemorrhagic shock may insinuate higher mortality.
While our study falls short of the level of evidence afforded by a randomized controlled trial comparing mini-PCNL with standard PCNL, all retrospective analyses have inherent limitations, and our database only allows us to account for some of these factors. In general, mini-PCNL is safe and effective for managing renal calculi. Little tract may bring less trauma to renal parenchyma than standard PCNL tract, especially in these renal collecting system with narrow infundibulum neck [5–7]. Compared to PCNL, mini-PCNL was associated with higher clearance rate, especially in decreasing the rate of bleeding necessitating transfusion and improving stone-free rate for multiple caliceal stones [20, 22]. The concept of a smaller nephrostomy sheath causing less invasiveness may be intuitive in thought but has not been fully examined. Li et al. [22] demonstrated no significant difference in associated invasiveness between the mini-PCNL and standard PCNL groups, by comparing the levels of inflammatory acute-phase mediators. The most important drawback of mini-PCNL that clearly emerged from our study was the longer operative time to dislodge stones than the standard PCNL [5, 20]. Compared to the septic shock rate of standard PCNL (0.5 %) [14], mini-PCNL group has a higher septic shock rate (2.40 %) in our study, in addition to the relatively longer duration of mini-PCNL, some patients referred from other clinics already had complicated medical conditions such as longer duration of diseases, multiple surgery history, poor health, which might contribute to the relative higher incidence of septic shock in our hospital.
Conclusion
Although septic shock following mini-PCNL is uncommon, it carries high morbidity and mortality. Female and diabetes mellitus were the high-risk factors. We recommend routine use of antibiotics in patients with higher risk factors, even if their preoperative urine cultures are negative. Early recognition and timely bundle treatment of septic shock may decrease the mortality.
References
Michel MS, Trojan L, Rassweiler JJ (2007) Complications in percutaneous nephrolithotomy. Eur Urol 51:899–906
Dellinger RP, Levy MM, Carlet JM et al (2008) Surviving sepsis campaign:international guidelines for management of severe sepsis and septic shock. Crit Care Med 36(1):296–327
Dellinger RP, Carlet JM, Masur H et al (2004) Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Intensive Care Med 30(4):536–555
Scherz HC, Parsons CL (1987) Prophylactic antibiotics in urology. Urol Clin North Am 14:265–271
Zhong W, Zeng G, Wu W et al (2011) Minimally invasive percutaneous nephrolithotomy with multiple mini tracts in a single session in treating staghorn calculi. Urol Res 39(2):117–122
Kruck S, Anastasiadis AG, Herrmann TR et al (2012) Minimally invasive percutaneous nephrolithotomy: an alternative to retrograde intrarenal surgery and shockwave lithotripsy. World J Urol [Epub ahead of print]
Schilling D, Gakis G, Walcher U et al (2011) The learning curve in minimally invasive percutaneous nephrolitholapaxy: a 1-year retrospective evaluation of a novice and an expert. World J Urol 29(6):749–753
Gutierrez J, Smith A, Geavlete P et al (2012) Urinary tract infections and post-operative fever in percutaneous nephrolithotomy. World J Urol [Epub ahead of print]
Gravas S, Montanari E, Geavlete P et al (2012) Postoperative infection rates in low risk patients undergoing percutaneous nephrolithotomy with and without antibiotic prophylaxis: a matched case control study. J Urol 188(3):843–847
Bootsma AM, Laguna Pes MP, Geerlings SE, Goossens A (2008) Antibiotic prophylaxis in urologic procedures: a systematic review. Eur Urol 54(6):1270–1286
Mariappan P, Smith G, Moussa SA, Tolley DA (2006) One week of ciprofloxacin before percutaneous nephrolithotomy significantly reduces upper tract infection and urosepsis: a prospective controlled study. BJU Int 98:1075–1079
Aghdas FS, Akhavizadegan H, Aryanpoor A et al (2006) Fever after percutaneous nephrolithotomy: contributing factors. Surg Infect 7(4):367–371
Foxman B (2002) Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 113:5S–13S
Seitz C, Desai M, Häcker A et al (2012) Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol 61(1):146–158
Mariappan P, Smith G, Bariol SV, Moussa SA, Tolley DA (2005) Stone and pelvic urine culture and sensitivity are better than bladder urine as predictors of urosepsis following percutaneous nephrolithotomy: a prospective clinical study. J Urol 173:1610–1614
Smith TP, Mark Ryan J, Niklason LE (2004) Sepsis in the interventional radiology patient. J Vasc Interv Radiol 15:317–325
Matlaga BR, Shah OD, Assimos DG (2006) Complications of percutaneous approaches, including incisions. In: Nakada SY, Pearle MS (eds) Advanced endourology: the complete clinical guide. Humana Press, Totowa, pp 283–297
Zhong W, Zeng G, Wu K et al (2008) Does a smaller tract in percutaneous nephrolithotomy contribute to high renal pelvic pressure and postoperative fever? J Endourol 22:2147–2151
Aghdas FS, Akhavizadegan H, Aryanpoor A et al (2006) Frequency of postpercutaneous nephrolithotomy fever and its contributing factors. Surg Infect 7:367–371
Cheng F, Yu W, Zhang X et al (2010) Minimally invasive tract in percutaneous nephrolithotomy for renal stones. J Endourol 24(10):1579–1582
Negrete-Pulido O, Gutierrez-Aceves J (2009) Management of infectious complications in percutaneous nephrolithotomy. J Endourol 23(10):1757–1762
Li LY, Gao X, Yang M et al (2010) Does a smaller tract in percutaneous nephrolithotomy contribute to less invasiveness? A prospective comparative study. Urology 75(1):56–61
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, C., Zhang, X., Liu, Y. et al. Prevention and treatment of septic shock following mini-percutaneous nephrolithotomy: a single-center retrospective study of 834 cases. World J Urol 31, 1593–1597 (2013). https://doi.org/10.1007/s00345-012-1002-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-012-1002-2