Abstract
Purpose
To investigate differences in the risk of benign prostatic hyperplasia (BPH)-related hospitalization, for surgical and non-surgical reasons, and of new prostate cancer (PCa) diagnosis between patients using finasteride or dutasteride.
Methods
A retrospective cohort study was conducted using data from record linkage of administrative databases (pharmaceutical prescription data, hospital discharge records, Italian population registry). Men aged ≥40 years old who had received a prescription for at least 10 packs/year between January 1, 2004 and December 31, 2004 were included and followed for 5 years.
The association of the outcomes was assessed using a multiple Cox proportional hazard model. Propensity score-matched analysis and a 5–1, greedy 1:1 matching algorithm were performed.
Results
8,132 patients were identified. Overall incidence rates of BPH hospitalization and BPH-related surgery were 21.05 (95 % CI 19.52–22.71) and 20.97 (95 % CI 19.45–22.61) per 1,000 person-years, respectively. In the dutasteride group compared with finasteride group, the incidence rate of both events was statistically significant lower: 16.07 versus 21.76 for BPH hospitalization and 15.91 versus 21.69 for BPH-related surgery. The incidence rate of new PCa was also lower for the dutasteride group [8.34 (95 % CI 5.96–11.68) vs. 10.25 (95 % CI 9.15–11.49)]. Dutasteride was associated with a reduction in BPH-related hospitalizations (HR 0.75, 95 % CI 0.58–0.98 and 0.58–0.98 for surgical and non-surgical reasons). The matched analysis confirmed the risk reduction with dutasteride for BPH-related surgery.
Conclusions
These findings suggest that the clinical effects of dutasteride and finasteride might be different. Patients treated with dutasteride seem to be less likely to experience BPH-related hospitalization. Comparative studies are needed to confirm these results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower urinary tract symptoms (LUTS) are common in aging men. There is an increasing understanding that male LUTS result from several pathophysiological conditions. Benign prostatic hyperplasia (BPH) has been recognized as a major contributing factor to the development of LUTS. Because of its high prevalence, the BPH management represents a challenging healthcare issue with economic implications [1]. The first-line pharmacological therapy for men with moderate-to-severe LUTS includes alpha-adrenoreceptor antagonists (ABs) and 5α-reductase inhibitors (5ARIs) alone or in combination [2]. In clinical practice, ABs are used for rapid symptom relief, while the 5ARIs modify the BPH natural history by delaying the disease progression [3–6]. Finasteride and dutasteride are the two 5ARIs clinically useful. In the prostate tissue, finasteride inhibits the type 2 5-α-reductase isoenzyme, whereas dutasteride inhibits both types (isoenzymes 1 and 2). This dual inhibition results in a greater serum dihydrotestosterone suppression [7]. However, the clinical value of the dual inhibition remains unclear [2]. Several studies have documented the efficacy of treatment with 5ARIs alone or in combination with ABs in the management of BPH [4, 5], but the question of what is, if any, “the best 5ARI” has rarely been addressed in part because comparative data are unavailable or scarce [8–11]. In addition, treatment with 5ARIs has been extensively investigated in order to reduce the incidence of newly detected prostate cancer, but the data, though encouraging, are inconclusive and inconsistent [12, 13]. The issue continues to be the subject of extensive debate within the medical and scientific societies and yet to be determined [14, 15], also considering a potentially different effect between the two drugs [10, 11, 16]. In this context, an observational study on unselected population and in the actual conditions of care can be considered a rich source of clinical information.
Methods and patients
We carried out a retrospective study based on information from three databases: pharmaceutical prescription data, hospital discharge records and Italian population registry. The examined databases include information on approximately 1,500.000 subjects aged ≥40 years. The analysis was performed in 22 Local Health Units between January 1, 2004 and December 31, 2008.
Data sources
The pharmaceutical prescription database documents all prescriptions reimbursed by the National Health System with drugs coded according to the international Anatomical Therapeutic Chemical system (ATC) [17]. The Hospital records include detailed information on primary diagnosis and up to five coexisting diagnoses, procedures performed, and dates of hospital admission and discharge. The diagnoses are classified, according to the International Classification of Diseases-Ninth Revision, Clinical Modification (ICD9-CM) [18]. The Italian population registry provides demographic information (date of birth, sex and date of death if this occurred) on each subject.
A record linkage of these three databases was carried out and pharmacological and clinical history for each patients was obtained. The reliability of this strategy to produce an epidemiological survey has been previously validated and reported [19–21]. All security and protection measures for patient’s data were performed according to National laws on privacy protection.
Patients and drugs
The cohort consisted of men aged ≥40 years, who received prescription for at least 10 boxes/year of finasteride or dutasteride in the index year (2004). We have arbitrarily considered the cut off value of 10 boxes/year as reasonable chronic BPH treatment. The first prescription of one of these drugs during the index year was considered as index date (Day 0) for including patient. The exclusion criteria were either exclusive ABs therapy and/or short-term 5-ARI therapy (<10 boxes/year). Dutasteride was commercialized in June 2004, so all patients identified in this year were the new users of this drug. To ensure the same condition for patients treated with finasteride, men who received prescription of this drug in the year preceding the index date were excluded from the cohort. Furthermore, for all patients, the databases were searched during the 12-month period preceding the index date to verify the absence of BPH complications and cancer prostate (PCa). Specifically, patients with an urethral stricture (ICD9-CM: 598, 589.0, 598.00, 598.01, 598.1, 598.2, 598.8, 598.9) and/or with PCa diagnoses (ICD9-CM: 185, 198.82, 233.4, 236.5, 239.5, V10.46) and/or at least a prescription of LHRH analogues and/or antiandrogens were not considered eligible. Patients using ABs (alfuzosin, tamsulosin, terazosin) were included in the study. Moreover, to assess the comorbidities, the Charlson Comorbidity Index (CCI) with the Dartmouth-Manitoba modification was used [22, 23].
Clinical outcomes
Follow-up for each identified patient is extended from the index date to 5 years or until the occurrence of the following major events:
-
hospitalization for BPH (non-surgical reasons);
-
hospitalization for BPH-related surgery;
-
new diagnosis of PCa.
The occurrence of hematuria (ICD9-CM:599.7), bladder stones and diverticula (ICD9-CM:592.0, 592.1, 592.9, 594.1, 563.3), bladder neck obstruction (ICD9-CM:599.7), urinary retention and obstruction (ICD9-CM:788.20, 599.6), acute and chronic renal failure (ICD9-CM:584, 585, 586), hydronephrosis (ICD9-CM:591), urinary infection (ICD9-CM:595.0, 595.4) were also assessed to capture and characterize the “severity factors” in the population.
The new diagnosis of PCa was identified through hospitalization (ICD9-CM:185, 198.82, 233.4, 236.5, 239.5, V10.46) and/or PCa medical therapy (GnRH agonists L02AE01, L02AE02, L02AE03, L02AE04; and/or antiandrogens: L02BB01, L02BB02, L02BB03).
Statistical analysis
For the whole sample, patients’ characteristics were reported as frequency (percentage) and mean ± standard deviation. Differences between patients’ treatment subgroups were assessed using standardized difference. For major outcomes, crude incidence rates (IRs) per 1000 men-year were calculated as the number of events divided by the number of person-years of follow-up. Incidence rate ratios (IRRs) with 95 % confidence intervals (CIs) were calculated using Poisson regression model.
The association of hospitalization for BPH, BPH-related surgeryand PCa was assessed using a multiple Cox proportional hazard model. All multivariate analyses were adjusted for the following variables: age, Charlson comorbidity score, previous hospitalization for BPH, previous BPH-related surgery, pre-existing severity factors, previous pharmacological treatment with ABs. Results are expressed as hazard ratios (HRs) and 95 % confidence intervals (CIs).
Furthermore, to check consistency of our results, a propensity score (PS)–matched analysis was performed [24, 25]. A logistic model including the same covariates used in the multivariate Cox model—plus quadratic terms and a set of two-term interactions between the same covariates—was performed to predict the probability to be assigned to study drugs. PS logistic model was selected in a stepwise fashion, and pair-wise comparisons were performed. A 5–1, greedy 1:1 matching algorithm [26] was used to identify a unique matched control for treated patient according to their PS. Adequacy of covariate balance in the matched sample was assessed via standardized difference between the two groups, considering differences less than 10 % as good balance [27].
Finally, since PS methodology addresses only imbalances due to measured confounders, we also performed a sensitivity analysis to account for potential residual confounding deriving from the effect of an unmeasured binary covariate [28].
p values <0.05 were considered significant. All analyses were performed using SAS Statistical Package Release 9.2 (SAS Institute, Cary, NC, USA).
Results
Patients characteristics
From 1,417.969 men aged ≥40 years, 72,943 (5 %) chronically treated with drugs for BPH were identified, without significant variation in prescriptions across the 22 Local Health Units. Among these, 8,132 were chronically exposed to 5ARIs; 7,111 received finasteride and 1,021 dutasteride. No significant differences were observed between these two groups with exception of previous ABs therapy (Table 1).
Clinical outcomes during follow-up
During 5 years, 673 patients were hospitalized for BPH non-surgical reasons, 675 for BPH-related surgery and 330 were newly diagnosed with PCa. The overall hospitalization IR for BPH non-surgical reasons and for BPH-related surgery were 21.05 (95 % CI, 19.52–22.71) and 20.97 (95 % CI, 19.45–22.61) per 1000 person-years, respectively. Among patients under dutasteride compared with those under finasteride, the IR of both events was lower (IRR = 0.74; 95 % CI, 0.57–0.96; for both hospitalizations) (Table 2). For new-onset PCa, the overall IR was 10.02 (95 % CI, 8.99–11.16) per 1000 person-years with no difference between the two drug groups (IRR = 0.81; 95 % CI, 0.57–1.16) (Table 2).
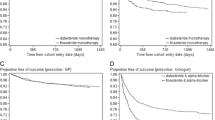
The multivariate analysis showed that dutasteride was associated with an independent reduced likelihood of hospitalization for BPH and for BPH-related surgery (HR 0.75; 95 %CI, 0.58–0.98 and HR 0.75; 95 % CI, 0.58–0.98; p = 0.03) and a positive trend, not statistically significant, toward less risk of newly detected PCa (HR 0.81, 95 % CI, 0.57–1.16; p = 0.24). The adjusted survival curves of patients under dutasteride and those under finasteride are presented in Fig. 1.
The matched analysis identified 2,042 patients: 1,021 under dutasteride were matched with 1,021 under finasteride. No significant differences were observed among groups (Table 1). The adjusted propensity score–matched Cox model confirmed the positive effect of dutasteride only on hospitalization for BPH-related surgery (HR 0.68, 95 % CI, 0.48–0.96; p < 0.02); no significant differences were observed for non-surgical BPH hospitalization (HR 0.76, 95 % CI, 0.54–1.07; p = 0.11) and for newly detected PCa (HR 0.78,95 % CI, 0.48–1.27; p = 0.31). Moreover, the sensitivity analysis showed that in order to modify the results, an unmeasured confounder should have a hypothetical hazard ratio of at least 1.25 (HR > 1.25) and an asymmetrical distribution between finasteride and dutasteride groups of at least 20 % for both the outcomes analyzed (surgical and non-surgical hospitalization).
Discussion
Dutasteride and finasteride are the two currently available 5ARIs and are widely recommended in patients with moderate-to-severe BPH-related LUTS [6]. Their short- and long-term (i.e., >4 years) efficacy and safety profiles have been demonstrated in numerous clinical studies [4, 5].
By blocking both the type-1 and type-2 5α-reductase-isoenzymes, dutasteride achieves 50 % more serum dihydrotestosterone suppression than finasteride. Because it is still not clear whether and to what extent this increased suppression affects the clinical outcomes, a long-term comparative study between the two drugs would be advisable in order to clarify the benefit of the dual 5αR-isoenzymes inhibition.
Placebo-controlled studies have shown reduced rates of acute urinary retention (AUR) and surgical therapy with both 5ARIs. In the PLESS study, after 4 years, finasteride treatment reduced the relative risk of AUR by 57 % and of surgery by 55 % [29]. In the MTOPS study, a significant reduction in the risk of overall clinical progression by 34 % was reported [4]. The COMBAT study also reported lower incidence of AUR in the dutasteride group (2.7 %) compared to the tamsulosin group (6.8 %) [5]. However, a comparative analysis of these results cannot be made, because differences in patient populations and in trial design may have affected the outcomes.
The EPICS study, the only randomized clinical trial comparing dutasteride vs finasteride, did not show significant differences between the drugs in terms of clinical efficacy. However, as pointed out by the authors, the study had two main limitations: the use of prostate volume as surrogate endpoint for AUR and BPH-related surgery and the too short (1-year) duration [11].
In lack of valuable, prospective comparator studies, the purpose of the present study was to assess the likelihood of BPH-related hospitalization, surgery and new detection of PCa in patients under dutasteride or finasteride therapy in a real-world, managed care setting. Even with the well-known limitations of this kind of approach, this study has been conducted because it reflects the real life of prescriptions, clinical uses, and finally physician’s attitudes.
In our study cohort, the crude incidence rate of hospitalization for BPH medical reasons and for BPH surgery were 21.7 and 21.6 in the finasteride group and 16.0 and 15.9 in the dutasteride group, respectively. These findings confirm that patients treated with dutasteride are less likely to experience BPH hospitalization and BPH-related surgery than patients treated with finasteride (Fig. 1). Our results are similar to those reported by Issa [10]. The authors, albeit in a smaller population, showed that patients under dutasteride were protected against the AUR risk with a trend toward less prostate-related surgery. In another study, Fenter showed a statistically significant difference in the likelihood of AUR and prostate surgery between dutasteride and finasteride [30], in favor of dutasteride.
Taken together, this evidence supports the clinical benefit of the dual 5α-reductase-isoenzymes inhibition. The two molecules are effective in BPH; nevertheless, due to its peculiar pharmacokynetic and pharmacodynamic characteristics (longer half-life and dual inhibition of 5α-reductase-isoenzymes), dutasteride seems to be more active.
As far as the new diagnosis of PCa is concerned, in our peculiar setting, we found a PCa incidence lower (IR10.03 finasteride group vs IR8.22 dutasteride group) than that reported in the PCPT and REDUCE trials (18.4 and 19.9 %, respectively) [12, 13]. This discrepancy reflects the fact that both trials were conducted in men at risk for PCa (particularly REDUCE), but without a PCa diagnosis at study entry. On the other hand, we analyzed a very large, unselected population typical of observational studies, which better reflects the real-world practice and policy.
Despite the lack of significant differences in PCa detection, we have found a positive trend in favor of dutasteride (HR, 0.81; 95 % CI, 0.57–1.17; p = 0.25). This outcome could also reflect the more intense hormonal suppression made by dutasteride and could be verified in a larger sample size with a longer follow-up.
Although our results suggest that there are differences between the two 5ARIs in terms of clinical outcomes, interpretation of the results is limited by the retrospective, non-randomized nature of the study. In fact, we have no information about symptoms scores, uroflowmetry parameters, baseline PSA values, number and kind of biopsies and Gleason score. This is main limitation of the study that hinders any inference about detailed outcomes (such as the subjective burden of the disease and the tumor aggressiveness). However, the administrative database is widely used with all the inherent limitations and is considered a valuable source of clinical information [19–21].
To minimize the influence of selection bias, our analysis was adjusted for several covariates and was also refined by using the propensity score–matched analysis, the matching algorithm and the sensitivity analysis to account for potential residual confounders deriving from the effect of an unmeasured binary covariate.
In conclusion, the comparison of dutasteride and finasteride monotherapies shows that treatment with dutasteride significantly reduces the overall risk of BPH-related surgery hospitalizations. About the risk of PCa development, the effect of dutasteride treatment, as compared to finasteride, shows a positive trend although this did not reach statistical significance. Further clinical trials are warranted in order to evaluate the long-term effectiveness of these drugs.
References
Emberton M, Fitzpatrick JM, Garcia-Losa M, Qizilbash N, Djavan B (2008) Progression of benign prostatic hyperplasia: systematic review of the placebo arms of clinical trials. BJU Int 102:981–986
Oelke M, Bachmann A, Descazeaud A,et al. Guidelines on Management of Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO) Uroweb 2012. Accessed 21 June 2012 at http://www.uroweb.org/gls/pdf/12_Male_LUTS_LR%20May%209th%202012.pdf
Boyle P, Roehrborn C, Harkaway R, Logie J, de la Rosette J, Emberton M (2004) 5-alpha reductase inhibition provides superior benefits to alpha blockade by preventing AUR and BPH-related surgery. Eur Urol 45:620–626
McConnell JD, Roehrborn CG, Bautista O et al (2003) Medical therapy of prostatic symptoms (MTOPS) research group. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 349:2387–2398
Roehrborn CG, Siami P, Barkin J et al (2010) The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol 57:123–131
Robert G, Descazeaud A, de la Taille A (2011) Lower urinary tract symptoms suggestive of benign prostatic hyperplasia: who are the high-risk patients and what are the best treatment options? Curr Opin Urol 21:42–48
Clark RV, Hermann DJ, Cunningham GR, Wilson TH, Morrill BB, Hobbs S (2004) Marked suppression of dihydrotestosterone in men with benign prostatic hyperplasia by dutasteride, a dual 5alpha-reductase inhibitor. J Clin Endocrinol Metab 89:2179–2184
Naslund M, Black L, Eaddy M, Batiste LR (2007) Differences in alpha blocker usage among enlarged prostate patients receiving combination therapy with 5 ARIs. Am J Manag Care 13:S17–S22
Naslund M, Regan TS, Ong C, Hogue SL (2008) 5-Alpha reductase inhibitors in men with an enlarged prostate: an evaluation of outcomes and therapeutic alternatives. Am J Manag Care 14:S148–S153
Issa MM, Runken MC, Grogg AL, Shah MB (2007) A large retrospective analysis of acute urinary retention and prostate-related surgery in BPH patients treated with 5-alpha reductase inhibitors: dutasteride versus finasteride. Am J Manag Care 13:S10–S16
Nickel JC, Gilling P, Tammela TL, Morrill B, Wilson TH, Rittmaster RS (2011) Comparison of dutasteride and finasteride for treating benign prostatic hyperplasia: enlarged Prostate International Comparator Study (EPICS). BJU Int 108:388–394
Thompson IM, Goodman PJ, Tangen CM et al (2003) The influence of finasteride on the development of prostate cancer. N Engl J Med 349:215–224
Andriole GL, Bostwick DG, Brawley OW et al (2010) Effect of dutasteride on the risk of prostate cancer. N Engl J Med 362:1192–1202
Theoret MR, Ning YM, Zhang JJ, Justice R, Keegan P, Pazdur R (2011) The risks and benefits of 5α-reductase inhibitors for prostate-cancer prevention. N Engl J Med 365:97–99
Margel D, Fleshner N (2012) The role of 5-alpha-reductase inhibitors in active surveillance. Curr Opin Urol 22:243–246
Cohen SA, Parsons JK (2012) Combination pharmacological therapies for the management of benign prostatic hyperplasia. Drugs Aging 29:275–284
WHO Collaborating Centre for Drug Statistics Methodology (2003) ATC Index with DDDs. WHO, Oslo, Norway
US Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessibility verified 14 May 2012
Monte S, Macchia A, Pellegrini F et al (2006) Antithrombotic treatment is strongly underused despite reducing overall mortality among high-risk elderly patients hospitalized with atrial fibrillation. Eur Heart J 27:2217–2223
Macchia A, Monte S, Romero M, D’Ettorre A, Tognoni G (2007) The prognostic influence of chronic obstructive pulmonary disease in patients hospitalized for chronic heart failure. Eur J Heart Fail 9:942–948
Macchia A, Monte S, Pellegrini F et al (2008) Depression worsens outcomes in elderly patients with heart failure: an analysis of 48,117 patients in a community setting. Eur J Heart Fail 10:714–721
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40:373–383
Romano PS, Roos LL, Jollis JG (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46:1075–1079
D’Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281
Yanovitzky I, Zanutto E, Hornik R (2005) Estimating causal effects of public health education campaigns using propensity score methodology. Eval Program Plann 28:209–220
Parsons LS (2004) Reducing bias in a propensity score matched pair sample using greedy matching techniques. Proceedings of the Twenty-Sixth Annual SAS Users Group International Conference. SAS Institute, Cary, NC, In
Austin PC, Grootendorst P, Anderson GM (2007) A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 26:734–753
Lin DY, Psaty BM, Krommal RA (1998) Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics 54:948–963
McConnell JD, Bruskewitz R, Walsh P et al (1998) The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. finasteride long-term efficacy and safety study group. N Engl J Med 338:557–563
Fenter TC, Runken MC, Black L, Eaddy M (2007) Finasteride versus dutasteride: a real-world economic evaluation. Am J Manag Care 13:S23–S28
Acknowledgments
This study was financially supported by an unconditional grant from GlaxoSmithKline.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cindolo, L., Fanizza, C., Romero, M. et al. The effects of dutasteride and finasteride on BPH-related hospitalization, surgery and prostate cancer diagnosis: a record-linkage analysis. World J Urol 31, 665–671 (2013). https://doi.org/10.1007/s00345-012-1000-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-012-1000-4