Abstract
Purpose
Androgen deprivation therapy (ADT) for prostate cancer (PCa) may increase peripheral insulin resistance, induce type 2 diabetes, change body composition, and alter lipoprotein profile. Some studies have reported an association between ADT and increased risk of cardiovascular events. It is known that serum level of fibrinogen (SF) is associated with coronary artery disease and increased cardiovascular risk (CVR). The aim of this study is to determine the increase in SF and C-reactive protein (CRP) of PCa patients on ADT.
Methods
Ninety-seven patients with locally advanced PCa (study group) were analyzed [mean age 73.4 years ± 6.3 SD, mean prostate specific antigen (PSA) 15.4 ng/ml ± 7.5 SD]. They were examined with blood chemistry including serum cholesterol (CHL), high density lipoproteins (HDL), low density lipoproteins (LDL), very low density lipoproteins, triacylglycerol (TAG), serum fibrinogen (FB), CRP and serum fasting glucose (SFG), serum testosterone, free testosterone at baseline, and after 12 months of ADT.
Results
Patients after 12 months of ADT (study group) had significantly higher overall serum CHL (p < 0.001), higher LDL (p = 0.01), higher FB (p < 0.001), higher serum SFG (p = 0.03) in comparison with the control group. Increase in HDL (p = 0.245) and CRP (p = 0.1) was not significant. Two patients from the study group were diagnosed with new-onset diabetes.
Conclusions
This is the first study that demonstrates the significant increase in FB in PCa patients on ADT, while CRP as inflammatory marker did not increase. Elevation of SF may contribute to increased CVR in PCa patients. Further prospective studies are warranted to confirm this association.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most commonly diagnosed cancer and the second leading cause of cancer death in men in the United States [1]. Nevertheless, the 5-year relative survival rate for men diagnosed with PCa is 99.7 % for white men, 96.2 % for black men, respectively [2]. Almost 10 % of patients live 10 years beyond the diagnosis of metastatic disease [3]; therefore, the treatment related morbidity is an important issue, especially when long-term treatment is administered.
In 1941, Huggins et al. [4] described the androgen dependence of PCa by showing that castration decreases its growth. Later on, androgen deprivation therapy (ADT) has been the cornerstone in the treatment of advanced and metastatic PCa. In metastatic disease, ADT has been shown to significantly improve morbidity, quality of life, and bone pain [5]. Furthermore, GnRH agonists improve disease-free and overall survival when administered in combination with external beam radiation therapy for locally advanced or high-risk nonmetastatic disease [6]. However, there has been an increasing trend of employing ADT even in patients with localized PCa and in those who experience biochemical PSA recurrence, even though no survival advantage has been shown in such patients [7]. The report of Shahinian et al. [8] revealed that the use of ADT has significantly increased from 3.7 % in 1991 to 31 % in 1999.
Androgen deprivation therapy is intended to cause severe hypogonadism. The drastic reduction in serum testosterone causes several undesirable changes. Side effects associated with ADT include skeletal complications, metabolic and cardiovascular complications, sexual dysfunction, hot flashes, and mood disorders [9–11]. Especially, skeletal, metabolic, and cardiovascular complications are particularly concerning because of their impact on morbidity as well as mortality. It was shown that administration of ADT reduces bone mineral density (BMD), which leads to the increased risk of skeletal fractures [12, 13], and these skeletal events negatively correlate with overall survival in men with PCa [14]. It also has been demonstrated that ADT decreases insulin sensitivity [15, 16] alters cholesterol levels and lipoprotein profile [17] and causes unfavorable changes in body composition [18], all of which are risk factors for metabolic syndrome, diabetes, cardiovascular-related morbidity and mortality.
Fibrinogen (FB) is an inflammatory biomarker that has been independently associated with cardiovascular disease outcomes (both coronary heart disease and stroke) [19]. It plays a key role in thrombus formation, platelet aggregation and is a major contributor to plasma viscosity. It is also an acute-phase reactant, increased in inflammatory states. FB is associated with traditional cardiovascular risk (CVR) factors such as age, cigarette smoking, lipids, body mass index, diabetes, and blood pressure [20, 21] and has recently been associated with impaired myocardial systolic function [22].
We performed prospective study to determine the changes of fibrinogenemia, CRP and other CVR factors in patients with PCa treated by ADT. When using systematic search on www.pubmed.com with keywords “prostate cancer, ADT, fibrinogen” there are no studies related to this topic.
Patients and methods
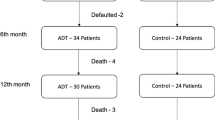
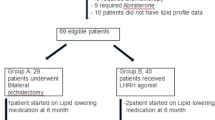
Ninety-seven patients with locally advanced PCa (study group) were analyzed [mean age 73.4 years ± 6.3 SD, mean prostate specific antigen (PSA) 15.4 ng/ml ± 7.5 SD]. Patients had verified PCa via prostate biopsy. They were examined with blood chemistry including serum cholesterol (CHL), high density lipoproteins (HDL), low density lipoproteins (LDL), very low density lipoproteins (VLDL), triacylglycerol (TAG), serum fibrinogen (FB), C-reactive protein (CRP) and serum fasting glucose (SFG), serum testosterone (TST), free testosterone (fTST) at baseline and after 12 months of ADT. All patients were mobile with Karnofsky performance status >50, without any major metabolic disorder (chronic renal failure, hypo- or hyperparathyreodism…) Patients were given LHRH agonists every 3 or 6 months. Patients with PSA >20 ng/ml were examined via bone scintigraphy and patients with bone metastasis were excluded from the study.
All measurements were performed by the same experienced physician, under standard conditions (blood samples collected between 8 and 10 a.m.), analyzed by the same certified laboratory. These measurements were also made to the control group of 89 patients (mean age 71.9 years, SD ± 6.7 mean PSA 2.4 ng/ml, SD ± 1.8). Patients of the control group were matched with the study group in terms of age and BMI. These patients had no history of any malignant or chronic metabolic disease. Patients of the control group were the patients who visited our department because of other urological problem (LUTS, stones, etc.…) Patients with the history of diabetes or patients taking cholesterol lowering drugs were excluded from the study.
All subjects gave their informed consent prior to study.
Statistical analysis
Quantitative variables are presented as mean and standard deviation. Nonparametric Mann–Witney U-test was used to compare independent quantitative variables between two groups. Chi-square test was used to compare qualitative variables between two or more groups. Two-tailed test was used for all comparisons. The value of p < 0.05 was considered as statistically significant. Statistical analysis was performed using the software Statistical Package for Social Sciences SPSS version 17.
Results
Results at the baseline are summarized in Table 1. Patients of the control group had significantly higher baseline overall cholesterol (p = 0.05). All other differences in results were statistically insignificant at the baseline.
Patients after 12 months of ADT (study group) had significantly higher overall serum CHL (p < 0.001), higher LDL (p = 0.01), higher FB (p < 0.001), higher SFG (p = 0.03) and BMI (p < 0.001) in comparison with the control group (Table 2). Increase in HDL (p = 0.245) and CRP (p = 0.1) was not significant (Table 2). Two patients from the study group were diagnosed with new-onset diabetes.
Discussion
As mentioned previously, FB that has been independently associated with cardiovascular disease (CVD) outcomes (both coronary heart disease and stroke) [19]. Increasing FB concentrations might promote risk via effects on atherogenesis (like lipoproteins, FB infiltrates the arterial wall and can be converted to fibrin and its atherogenic degradation products), thrombogenesis (promoting both platelet aggregation and fibrin formation, and making thrombi more resistant to lysis), and ischemia (increasing plasma and whole-blood viscosity) [20].
The association of FB with risks of CVD and mortality in healthy individuals has been reliably established through international collaborative individual-person meta-analyses. The Fibrinogen Studies Collaboration (FCS) involved combined analyses of individual data from 31 prospective studies of plasma FB levels in 154,211 adults without known CVD at an initial baseline examination [23], and its successor, the Emerging Risk Factors Collaboration [24], are the largest studies of its kind. FSC investigators have previously reported that a long-term increase in 1 g/l in plasma FB level is associated with an approximate doubling in risk of major CVD outcomes (such as coronary heart disease and stroke). The strength of FB’s associations with coronary heart disease and stroke is similar to those of classic risk factors, such as blood pressure and CHL, and to the circulating concentration of CRP [24].
Serum fibrinogen is also an inflammatory biomarker [19]. Few interventional studies have evaluated the relationship between male hypogonadism and serum levels of pro- and/or anti-inflammatory cytokines. In one study, acute induction of hypogonadism with GnRH agonists in healthy elderly men was followed by elevated serum levels of inflammatory cytokines TNF alpha and IL-1 beta, suggesting an anti-inflammatory role for testosterone [26]. The limitation of this study was the duration of ADT- only 4 months. In contrast, long-term ADT (at least 12 months) did not demonstrate elevated levels of inflammatory cytokines compared with age- and disease-matched controls [27].
The association between FB and CRP during acute inflammatory response is well known [20], as well as elevation of CRP and progression of PCa [28]. In our study, we found significant increase of FB, but not CRP. This indicates that the sole elevation of FB is related to induced hypogonadism, not to inflammation or cancer. Patients in this study had locally advanced disease, no metastasis was diagnosed at the baseline. This may also be the cause why CRP was not elevated.
Long-term ADT is associated with the rapid loss of BMD leading to bone fractures and increased morbidity and mortality [13]. Adverse effects of long-term ADT linked to CV morbidity include changes in body composition, alterations in lipoprotein profile, elevation of SFG, thus leading into the development of metabolic syndrome [15–17]. In this study, we proved the profound metabolic changes resulting from hypogonadism (elevation of overall cholesterol, LDL, SFG, BMI, two patients from the study group were diagnosed with new-onset diabetes). These significant changes may contribute to CV risk and development of metabolic syndrome.
Since FB levels can be reduced considerably by lifestyle interventions that also affect levels of established risk factors (such as regular exercise, smoking cessation, and moderate alcohol consumption) [29], physicians prescribing ADT should be aware of pluripotent role of testosterone, and possible consequences resulting from induced hypogonadism. Lifestyle modifications and interventions should be taken to minimize this risk and the possible effect of statins should be investigated, too.
Conclusions
To our knowledge, this is the first study which has shown the significant increase of FB in PCa patients on long-term ADT. The association of FB and its contribution to CV risk is unknown in PCa patients, since it has never been studied. However, the association of FB to CVD and stroke is well documented [24, 25]. ADT can increase CV morbidity per se [15–18]. What is the role of FB and how does FB contribute to this risk remains currently unknown. To answer these questions, larger prospective studies are warranted.
References
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics 2010. CA Cancer J Clin 60:277–300
Surveillance Epidemiology and End Results. SEER Stat Fact Sheets: Prostate Cancer. 2008 Available at: http://seer.cancer.gov/statfacts/html/prost.html Accessed 25 July 2011
Tangen CM, Faulkner JR, Crawford ED et al (2003) Ten-year survival in patients with metastatic prostate cancer. Clin Prostate Cancer 2:41–45
Huggins C, Stevens RE Jr, Hodges CV (1941) Studies on prostatic cancer. II. The effects of castration on advanced carcinoma of the prostate gland. Arch Surg 43:209–223
Chodak GW, Keane T, Klotz L (2002) Critical evaluation of hormonal therapy for carcinoma of the prostate. Urology 60:201–208
Bolla M, Collette L, Blank L et al (2002) Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet 360:103–106
Chodak GW (1998) Comparing treatments for localized prostate cancer: persisting uncertainty. JAMA 280:1008–1010
Shahinian VB, Kuo YF, Freeman JL, Orihuela E, Goodwin JS (2005) Increasing use of gonadotropin-releasing hormone agonists for the treatment of localized prostate carcinoma. Cancer 103:1615–1624
Green HJ, Pakenham KI, Headley BC et al (2004) Quality of life compared during pharmacological treatments and clinical monitoring for non-localized prostate cancer: a randomized controlled trial. BJU Int 93:975–979
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS (2006) Risk of the ‘‘androgen deprivation syndrome’’ in men receiving androgen deprivation for prostate cancer. Arch Intern Med 166:465–471
Alibhai SM, Gogov S, Allibhai Z (2006) Long-term side effects of androgen deprivation therapy in men with non-metastatic prostate cancer: a systematic literature review. Crit Rev Oncol Hematol 60:201–215
Ziaran S, Goncalves FM, Breza J (2011) Bone mineral density, pathological fractures and bisphosphonate therapy in prostate cancer patients on androgen deprivation therapy. Endocr Regul 45:199–204
Daniell HW, Dunn SR, Fergusson DW, Lomas G, Niazi Z, Srtatte PT (2000) Progressive osteoporosis during andorgen deprivation therapy for prostate cancer. J Urol 163:181–186
Oefelein MG, Ricchiuti V, Conrad W, Resnick MI (2002) Skeletal fractures negatively correlate with overall survival in men with prostate cancer. J Urol 168(3):1005–1007
Smith MR, Lee H, Nathan DM (2006) Insulin sensitivity during combined androgen blockade for prostate cancer. J Clin Endocrinol Metab 91:1305–1308
Basaria S, Muller DC, Carducci MA, Egan J, Dobs AS (2006) Hyperglycemia and insulin resistance in men with prostate carcinoma who receive androgen-deprivation therapy. Cancer 106(3):581–588
Smith JC, Bennett S, Evans LM, Kynaston HG, Parmar M, Mason MD, Cockcroft JR, Scanlon MF, Davies JS (2001) The effects of induced hypogonadism on arterial stiffness, body composition, and metabolic parameters in males with prostate cancer. J Clin Endocrinol Metab 86:4261–4267
Haseen F, Murray LJ, Cardwell CR, O’Sullivan JM, Cantwell MM (2010) The effect of androgen deprivation therapy on body composition in men with prostate cancer: systematic review and meta-analysis. J Cancer Surviv 4(2):128–139
Danesh J, Lewington S, Thompson SG, Lowe GD, Collins R, Kostis JB, Wilson AC, Folsom AR, Wu K, Benderly M et al (2005) Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA 294(14):1799–1809
Kaptoge S, White IR, Thompson SG, Wood AM, Lewington S, Lowe GD, Danesh J (2007) Associations of plasma fibrinogen levels with established cardiovascular disease risk factors, inflammatory markers, and other characteristics: individual participant meta-analysis of 154,211 adults in 31 prospective studies: the fibrinogen studies collaboration. Am J Epidemiol 166(8):867–879
Palmieri V, Celentano A, Roman MJ, de Simone G, Best L, Lewis MR, Robbins DC, Fabsitz RR, Howard BV, Devereux RB (2003) Relation of fibrinogen to cardiovascular events is independent of preclinical cardiovascular disease: the strong heart study. Am Heart J 145(3):467–474
Yan RT, Fernandes V, Yan AT, Cushman M, Redheuil A, Tracy R, Vogel-Claussen J, Bahrami H, Nasir K, Bluemke DA et al (2010) Fibrinogen and left ventricular myocardial systolic function: the multi-ethnic study of atherosclerosis (MESA). Am Heart J 160(3):479–486
Fibrinogen Studies Collaboration (2005) Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA 294:1799–1809
The Emerging Risk Factors Collaboration (2010) C-reactive protein concentration and the risk of coronary heart disease, stroke, and mortality. Lancet 375:132–140
Lowe GDO (1995) Fibrinogen and cardiovascular disease: historical introduction. Eur Heart J 16(Suppl A):2–5
Khosla S, Atkinson EJ, Dunstan CR, O’Fallon WM (2002) Effect of estrogen versus testosterone on circulating osteoprotegerin and other cytokine levels in normal elderly men. J Clin Endocrinol Metab 87:1550–1554
Maggio M, Blackford A, Taub D, Carducci M, Ble A, Metter EJ, Braga-Basaria M, Dobs A, Basaria S (2006) Circulating inflammatory cytokine expression in men with prostate cancer undergoing androgen deprivation therapy. J Androl 27:725–728
Elsberger B, Lankston L, McMillan DC, Underwood MA, Edwards J (2011) Presence of tumoural C-reactive protein correlates with progressive prostate cancer. Prostate Cancer Prostatic Dis 14(2):122–128
Danesh J, Collins R, Peto R, Lowe GDO (2000) Haematocrit, viscosity, erythrocyte sedimentation rate: meta-analyses of prospective studies of coronary heart disease. Eur Heart J 21:515–520
Conflict of interest
I certify that there is no actual or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ziaran, S., Goncalves, F.M. & Breza, J. Patients with prostate cancer treated by ADT have significantly higher fibrinogenemia than healthy control. World J Urol 31, 289–292 (2013). https://doi.org/10.1007/s00345-012-0926-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-012-0926-x