Abstract
Objectives
Report 20 years experience of bladder injuries after external trauma.
Methods
Gender, age, mechanism/location of damage, associated injuries, systolic blood pressure (SBP), Revised Trauma Score (RTS), Injury Severity Score (ISS), Trauma Injury Severity Score (TRISS), complications, and length of stay (LOS) were analyzed in a prospective collected bladder injuries AAST-OIS grade ≥II database (American Association for the Surgery of Trauma Organ Injury Scaling) from 1990 to 2009 in a trauma reference center.
Results
Among 2,575 patients experiencing laparotomy for trauma, 111 (4.3 %) presented bladder ruptures grade ≥II, being 83.8 % (n = 93) males, mean age 31.5 years old (±11.2). Blunt mechanism accounted for 50.5 % (n = 56)–motor vehicle crashes 47.3 % (n = 26), pedestrians hit by a car (29.1 %). Gunshot wounds represented 87.3 % of penetrating mechanism. The most frequent injury was grade IV (51 patients, 46 %). The mean ISS was 23.8 (±11.2), TRISS 0.90 (±0.24), and RTS 7.26 (±1.48). Severity (AAST-OIS), mechanism (blunt/penetrating), localization of the bladder injury (intra/extraperitoneal, associated), and neither concomitant rectum lesion were related to complications, LOS, or death. Mortality rate was 10.8 %. ISS > 25 (p = 0.0001), SBP <90 mmHg (p = 0.0001), RTS <7.84 (p = 0.0001), and pelvic fracture (p = 0.0011) were highly associated with grim prognosis and death with hazard ratios of 5.46, 2.70, 2.22, and 2.06, respectively.
Conclusions
Trauma scores and pelvic fractures impact survival in bladder trauma. The mortality rate has remained stable for the last two decades.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
About 10 % of all injuries seen in the emergency room involve the genitourinary system to some extent. These injuries are highly associated with severe multiple trauma, and failure of diagnosis can lead to significant morbidity and mortality [1].
Bladder injury after external trauma is uncommon and occurs as a result of blunt or penetrating trauma. In the USA and Europe, blunt trauma accounts for 67–86 % of bladder ruptures, while 14–33 % [2–4] for penetrating trauma.
Surgical intervention is needed on intraperitoneal injuries and on extraperitoneal ones that have associated injuries requiring exploration. Bladder injuries are highly associated with multisystem trauma, and bladder rupture has a reported mortality rate of 10–22 %, due to the fact that, from 35 to 90 % of the times it occurs with a pelvic fracture, stating high energy trauma involved [5–7].
In order to establish the patient’s overall situation and prognosis, trauma scores have been widely used over decades and can accurately state the patient’s condition and estimate their survival probability [8–11]; however, their relation to bladder injury has to be defined.
This study revisits the status and implication of bladder trauma in the last two decades and brings to light the meaning of using trauma scores as a tool in this scenario as well as exposes the underexplored impact of other associated lesions, mainly rectum injury on morbidity and survival.
Materials and methods
A medical chart review from a prospectively maintained database was performed from January 1990 to December 2009 in the Trauma Surgery Division of University of Campinas; responsible for all major traumatic and non-traumatic surgical emergencies in a metropolitan region consisting of 2.7 million people in São Paulo state, Brazil. The institutional review board and ethics committee have approved the study and in the hospital admittance patients or their family consent to have their data analyzed.
The inclusion criteria were patients experiencing laparotomy for trauma and bladder injury AAST-OIS [8] grade ≥II (American Association for the Surgery of Trauma Organ Injury Scaling).
Variables such as gender, age, AAST-OIS [8], mechanism (blunt or penetrating), location of injury (intra/extraperitoneal, associated), associated injuries (i.e., pelvic fractures, concomitant rectum lesion), complications (urinary and non-urinary), systolic blood pressure (SBP), Revised Trauma Score (RTS) [9], Injury Severity Score (ISS) [10], Trauma Injury Severity Score (TRISS) [11], and the length of stay (LOS) were analyzed.
Calculation of the RTS includes the Glasgow Coma Scale (GCS), systolic blood pressure (SBP), and the respiratory rate (RR) with values ranging from 0 to 7.84; lower values refer to the greater severity of physiologic disability [9]. ISS is an anatomical scoring system that provides an overall score for patients with multiple injuries. Varying from 0 to 75, scores from 16 to 25 represent severe and ≥25 represent very severe anatomical injury [10]. TRISS or Ps is the probability of survival for trauma patients and ranges from 0 to 0.99 [11].
The sequences of diagnostic and therapeutic procedures adopted were in agreement with normalization standards established by Advanced Trauma Life Support (ATLS®).
Bladder injuries were diagnosed by retrograde plain film cystography and computed tomography (CT) cystography in cases of patients with acute abdominal pain with no defined diagnosis [3, 6, 12]. Eventually, missed lesions were found intraoperative.
The treatment was determined by the location and extent of injury identified in the pre- or intraoperative time. Briefly, intraperitoneal bladder ruptures were surgically repaired. Minor isolated extraperitoneal bladder injuries were managed non-operatively with catheter drainage alone, prophylactic antibiotics, and a cystogram on the 10th to 14th day. In major extraperitoneal injuries on patients undergoing laparotomy for reasons other than urological injuries, the rupture was repaired transvesically by opening the dome, avoiding violation of the pelvic hematoma [12].
Urinary complications included urinary fistula, persistent hematuria, and urinary infection, while non-urinary (systemic) complications included pneumonia, renal insufficiency, coagulopathy, sepses, and thromboembolic events.
Statistical analyses were performed through the Statistical Analysis System software for Windows, version 9.2 (SAS Institute Inc, 2002–2008, Cary, NC, USA) in the following ways. To verify association between determined variables, a chi-squared test or Fisher’s test was used. To compare continued measures between two groups, the Mann–Whitney test was applied. To identify complications-associated risk factors, simple and multiple logistic regression of Cox were applied, and the hazard ratio (HR) calculated. A confidence interval (CI) of 95 % was chosen, and a two-sided p value of less than 0.05 was arbitrarily defined as significant.
Results
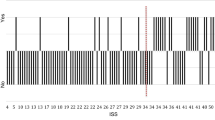
Among 2,575 patients experiencing laparotomy for trauma, 111 (4.3 %) AAST-OIS [8] grade ≥II bladder ruptures were identified, with 66 cases from 1990 to 1999 and 45 cases from 2000 to 2009.
Of all compiled patients, 83.8 % (n = 93) were males, and the average age was 31.5 years old (±11.2), reflecting young males in predominantly violent trauma.
Blunt mechanism has had a slightly higher occurrence in comparison with penetrating mechanism, accounting for 50.5 % (n = 56) of all cases admitted in our facility. Of these incidences, motor vehicle crashes (MVC) represented 47.3 % (n = 26), followed by pedestrians hit by a car (29.1 %) and falling from a great height (14.5 %). Assault and other blunt mechanisms represented the minority of 9.1 %.
Gunshot wounds have had an overwhelming rate (87.3 %), when compared to other kinds of penetrating mechanisms like stab wounds.
Up to 45.9 % (n = 51) of trauma patients were represented in the emergence room (ER) with intraperitoneal bladder rupture, 34.2 % (n = 38) with extraperitoneal, and 19.8 % (n = 22) with associated intra and extraperitoneal bladder injuries. The most frequent grade of injury in operative findings was AAST-OIS [8] grade IV (51 patients, 46 %), followed by grades III (45 patients, 40.5 %), II (14 patients, 12.6 %), and V (1 patient, 0.9 %).
In blunt trauma, twenty patients (35.7 %) had associated abdominal injuries, and in penetrating trauma the incidence of associated injuries was higher (41 patients, 74.5 %). Types of associated intra-abdominal injuries suffered by patients in the study group are listed in Table 1.
Pelvic fracture was surprisingly present in only 30.3 % (n = 34) of the patients, the large majority related to blunt mechanism (n = 32). Only two were open injuries (compound pelvic fractures), both by gunshot wound, classified as such where there was a soft-tissue defect communicating with the pelvic fracture. Seventy-two percent of all admitted patients were considered with no other concomitant fractures.
The following were the averages of trauma scores on patient’s arrival: RTS, 7.26 (±1.48); ISS, 23.8 (±11.2); and TRISS, 0.90 (±0.24).
The mean arterial SBP was found to be 118.2 mmHg. Eighty-five percent of the patients were found with SBP higher than 90 mmHg; 36.9 % recorded the ISS of ≤16 and 32.4 % >25, indicating a heterogeneous trauma population.
Only 10 patients (9 %) underwent bladder non-operative treatment through catheter drainage due to extraperitoneal lesions, despite laparotomy and one missed (intra and extraperitoneal) lesion was intraoperative found despite the preoperative diagnostic workup with CT due to insufficient bladder distension.
Surgical repair with absorbable suture was the treatment in 101 cases (90.9 %) with intraperitoneal, associated lacerations or extraperitoneal on patients undergoing laparotomy for reasons other than urological injuries.
A supra-pubic cystostomy catheter was inserted to protect the repair in eight patients (7.2 %) with complex injuries (three had associated urethral tears).
Complications were present in 37.8 % of all operated patients, and 10.8 % (n = 12) resulted in death from either associated injuries or its complications. Patients presenting systemic, non-urinary complications were more prone to fatality 26.2 % (11 cases among 42); compared to non-complicated patients 1.4 % (one case among 69), p < 0.0001. There was no mortality due to urinary complications, and urinary infections were diagnosed in seven patients (6.3 %) and urinary fistula in two (1.8 %).
Neither the severity (AAST-OIS grade) of the bladder injury or the trauma mechanism (blunt or penetrating) or the kind of rupture (intraperitoneal, extraperitoneal, or associated) was related to the presence of complications, to the length of hospital stay or to death.
After analyzing the impact of concomitant rectum lesion, it was not considered a determining prognosis factor. Considering the death rate, it was 11.4 % (10 among 88) for negative versus 8.7 % (2 among 23) for positive rectum lesion, p = 1.0000.
After utilizing simple and multiple logistic regression to determine complications risk factors for bladder trauma, we could be able to define that ISS >25 (p = 0.0005), SBP <90 mmHg (p = 0.0031), RTS <7.84 (p = 0.0110), and pelvic fracture (p = 0.0194) are the most important predictors for complications. Table 2 shows the hazard ratio and confidence interval for the variables.
Although blunt trauma and specifically MVC were associated with a larger number of deaths, only ISS >25 (p = 0.0001), SBP <90 mmHg (p = 0.0001), RTS <7.84 (p = 0.0001), and pelvic fracture (p = 0.0011) were statistically highly associated with grim prognosis (Table 2) and death.
Comparing the first and the second decades studied, 1990–1999 and 2000–2009, there was a significant decrease in pelvic fractures in the last decade, 37.9 % (25 among 66 cases) versus 20 % (9 among 45 cases), respectively, p = 0.0448. Furthermore, a higher mean arterial systolic blood pressure (SBP) was verified in the last decade than in the first decade, 125.12 ± 24.72 versus 113.79 ± 26.36 (p = 0.0117).
While SBP has significantly increased and pelvic fracture significantly decreased in the last decade, complications and death rates were comparable between decades. Complications occurred in 39.4 % (26 cases among 66) in the first decade versus 35.6 % (16 cases among 45) in the second decade, p = 0.6823. Death occurred in 9.1 % (six cases among 66) in the first decade versus 13.3 % (6 cases among 45), p = 0.5417.
Discussion
The bladder’s special position, deep within the bony pelvis, protects it against trauma, especially when empty. Bladder trauma is seldom an isolated injury; however, it is usually one part of multiple injuries. Many studies have stated that bladder injury is frequently missed in multiple trauma cases, because of attention being focused on more life-threatening injuries, that is, head injury, tension pneumothorax, hemothorax, and/or hemoperitoneum [13]. In our series, we could be able to prove otherwise, presumably because of the severe heterogeneity of our admitted trauma patients.
Injuries that result in bladder trauma also commonly share direct force on the pelvis. However, it is important to recognize the bladder as a separate organ with potential for isolated injury.
Furthermore, there was an increasing trend to suture bladder ruptures during concomitant surgery directed to associated injuries (101 cases, 90.9 %) in agreement with recently published series [14].
Different from ureteral injuries, the two most common signs and symptoms of bladder injury, for instance, are macroscopic hematuria (80 %) and abdominal tenderness (60 %). Other findings include the inability to void urine, bruising of the supra-pubic region, and extravasations of urine. Pelvic fractures associated with multiple organ damage, including bladder, have a significant mortality rate (20–40 %), as we also could be able to see in this study; however, the low incidence rate of pelvic fracture in our studied group challenged the authors to find a specific reason for that [15, 16]. One of the possible reasons is that penetrating trauma (i.e., gunshot wounds) accounts for almost 50 % of the bladder injuries, being much higher than other reports, and could account for why the incidence of pelvic fracture is much lower.
The present results are not in perfect agreement with previously published data, which states that extraperitoneal ruptures are more commonly seen, leading us to wonder whether or not the incidence of intra/extraperitoneal bladder injuries could geographically switch worldwide, or if what we found here is a regional isolated fact [17]. It is also likely that the high incidence of intraperitoneal rupture came from penetrating injury and not blunt trauma, considering the percentage of pelvic fracture with bladder rupture after blunt trauma.
Another thing, according to our knowledge, that is novel in this series is the correlation made with trauma scores to this extent. We have seen some correlation to age, Glasgow Coma Scale and SBP, but none of the manuscripts researched by these authors guided the readers’ attention to how important is the use of trauma scores related to bladder injuries [18]. By the routine use of RTS and ISS, one will not only be able to estimate their survival probability, but also predict complications in this specific population of bladder-injured patients.
Comparing the determining complications risk factors for bladder trauma, Table 2 shows the hazard ratio and confidence interval to each one of the variables, defining those more likely to impact patients prognosis (ISS >25 and SBP <90 mmHg, respectively). In this regard, it is clear the interaction between SBP and RTS once the last variable is a derivate from GCS, SBP, and RR as described in the methods section.
Additionally, we attempted to classify bladder injuries according to AAST-OIS [8], and as observed by others, no statistically significant correlation was found between the grade of bladder injury and morbidity. The proposed current bladder trauma classification did not add significant information regarding prognosis and treatment. Important factors impacting survival in patients presenting bladder trauma were the presence of pelvic fracture (mostly for closed bladder trauma) and trauma scores (physiologic and anatomic), which the urologist who deals with trauma should be familiar. In clinical practice, the trauma scores are more important than the mechanism, grade, or kind of bladder injury.
Albeit a significant decline was shown in pelvic fracture incidences in the last decade in association with bladder trauma, as well as higher-pressure levels for patients arriving in the ER, these factors did not significantly impact survival, which has remained stable for bladder trauma over the last 20 years.
Neither the severity of the bladder injury (AAST-OIS) or the trauma mechanism (blunt or penetrating), or the kind of rupture (intraperitoneal, extraperitoneal, or associated) was the prognostic factor and did impact the survival of bladder trauma.
Although 55.9 % of our studied group was admitted with multiple injuries, indicating that bladder injuries often occur as part of a myriad of problems associated with significant trauma, the mean length of stay was relatively short (10.83 ± 11.06 days).
As for pelvic fractures with closed bladder trauma (confirmed important prognostic factor in the presented series), we revolutionarily hypothesized that rectum lesions could be considered an important additional morbidity for patients presenting open bladder trauma. To the best of our knowledge, there are no data regarding the impact of rectal injury on open bladder trauma patients’ survival. In fact, despite clear additional morbidity for obvious reasons, such as contamination, rectum lesion did not impact survival in the presented series. Whereas future studies are warranted to confirm our results, this is one feature deserving spotlight once underexplored.
It should be emphasized that the bladder injuries were determined by findings at exploratory laparotomy for trauma, being these data an exceptional cross-sectional view of bladder trauma, which takes advantage of its unique features (developing world setting; operative diagnosis; high percentage of penetrating injuries).
This study is limited in that it is a regional research with a relatively small population in the urban setting not reflecting diverse scenery, that is, rural. However, it is the reflection of our reality, and the largest series ever reported in our home country and Latin America. Through this study, we expect to bring to light the importance of using trauma scores as complication predictors estimating patient’s prognosis as reliable and useful tools to our daily practice in managing bladder trauma.
Conclusions
Trauma scores and pelvic fractures impact survival in bladder trauma. ISS >25, SBP <90 mmHg, RTS <7.84, and pelvic fracture are associated with higher mortality rates in bladder-injured patients, respectively. The mortality rate has remained stable for the last two decades, and concomitant rectum lesion was not considered a determining prognostic factor.
References
Shenfeld OZ, Gnessin E (2011) Management of urogenital trauma: state of the art. Curr Opin Urol 21(6):449–454
Srinivasa RN, Akbar SA, Jafri SZ et al (2009) Genitourinary trauma: a pictorial essay. Emerg Radiol 16(1):21–33
Lynch TH, Martinez-Pineiro L, Plas E et al (2005) EAU guidelines on urological trauma. Eur Urol 47(1):1–15
Reis LO, Barreiro GC, D’Ancona CA et al (2007) Arteriovesical fistula as a complication of a gunshot wound to the pelvis: treatment dilemma. Int J Urol 14(6):569–570
Tezval H, Tezval M, von Klot C et al (2007) Urinary tract injuries in patients with multiple trauma. World J Urol 25(2):177–184
Morey AF, Iverson AJ, Swan A et al (2001) Bladder rupture after blunt trauma: guidelines for diagnostic imaging. J Trauma 51(4):683–686
Corriere JN Jr, Sandler CM (2006) Diagnosis and management of bladder injuries. Urol Clin North Am 33(1):67–71
Moore EE, Cogbill TH, Jurkovich GJ et al (1992) Organ injury scaling III: chest wall, abdominal vascular, ureter, bladder, and urethra. J Trauma 33(3):337–339
Champion HR (1989) A revision of the trauma score. J Trauma 29(5):623–629
Baker SP, O’Neill B, Haddon W Jr et al (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14(3):187–196
Boyd CR, Tolson MA, Copes WS (1987) Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma 27(4):370–378
Gomez RG, Ceballos L, Coburn M et al (2004) Consensus statement on bladder injuries. BJU Int 94(1):27–32
Ziran BH, Chamberlin E, Shuler FD et al (2005) Delays and difficulties in the diagnosis of lower urologic injuries in the context of pelvic fractures. J Trauma 58(3):533–537
Wirth GJ, Peter R, Poletti PA et al (2010) Advances in the management of blunt traumatic bladder rupture: experience with 36 cases. BJU Int 106:1344–1349
Pereira BM, Ogilvie MP, Gomez-Rodriguez JC et al (2010) A review of ureteral injuries after external trauma. Scand J Trauma Resusc Emerg Med 18:6
Fraga GP, Borges GM, Mantovani M et al (2007) Penetrating ureteral trauma. Int Braz J Urol 33(2):142–150
Brandes S, Borrelli J Jr (2001) Pelvic fracture and associated urologic injuries. World J Surg 25(12):1578–1587
Bjurlin MA, Fantus RJ, Mellett MM et al (2009) Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Trauma 67(5):1033–1039
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pereira, B.M.T., de Campos, C.C.C., Calderan, T.R.A. et al. Bladder injuries after external trauma: 20 years experience report in a population-based cross-sectional view. World J Urol 31, 913–917 (2013). https://doi.org/10.1007/s00345-012-0871-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-012-0871-8