Abstract
Objectives
Current treatments for localized prostate cancer include brachytherapy, external beam radiation, surgery, and active surveillance. Unfortunately, 20–40% of prostate cancer patients will experience recurrence and require hormonal therapies. These therapies involve androgen ablation by chemical or surgical castration and application of antiandrogens. Hormonal therapy is initially effective, but will inevitably fail and the disease will progress to lethal castration-resistant prostate cancer (CRPC) from which patients succumb within 2 years. CRPC is considered to be dependent on transcriptionally active androgen receptors (AR). This article reviews recent advances in the discovery and development of small molecule inhibitors of AR.
Methods
A PubMed database search was performed for articles focused on small molecule inhibitors of AR for potential development for the treatment of prostate cancer. Compounds with broad effects on other pathways were not included.
Results
Currently, there are several novel antiandrogens being tested in the clinic that have improved affinity for the AR and work by different mechanisms to the current battery of approved antiandrogens that are discussed. Small molecule inhibitors that interact with regions other than the AR ligand-binding pocket have been also been discovered. These small molecules include allosteric inhibitors of the LBD, compounds that alter AR conformation, and antagonists to the AR NTD and are highlighted.
Conclusions
CRPC is dependent upon transcriptionally active AR. Survival improvement may be achieved by complete blockade of all AR activity using novel small molecule inhibitors with unique mechanisms of action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prostate is an androgen-dependent tissue. Upon removal of testicular androgens by chemical or surgical castration, the prostate will involute with apoptosis of the luminal epithelial cells. Androgen mediates its effect through the ligand-activated transcription factor, the androgen receptor (AR). The dependency of prostate upon androgen forms the rationale for blocking AR activity for the treatment of advanced prostate cancer by androgen ablation and competitive inhibitors to the AR. While initially effective, all current forms of hormonal therapies to block AR activity ultimately fail and the disease will progress to lethal castration-resistant prostate cancer (CRPC). This article focuses on the recent advances in the development of small molecule inhibitors of the AR.
Structure and function of the AR
AR is a member of the steroid receptor superfamily that includes the closely related receptors, progesterone receptor (PR) and glucocorticoid receptor (GR). Structural similarity between these receptors is highest at the C-terminal ligand-binding domain (LBD), and the DNA-binding domain (DBD) being greater than 50 and approximately 80%, respectively, for each domain. AR LBD and DBD are folded with the crystal structures solved. Inhibitors that bind the AR LBD may also inhibit PR activity such as bicalutamide [1]. Generally, the LBD has 12 α-helices with helices 3, 4, and 12 being integral to ligand-binding and interactions with other proteins. The N-terminal domains (NTD) have little sequence homology with less than 15% between the AR and PR or GR. AR NTD is unique from other steroid receptors because this domain contains most of the transcriptional activity of the receptor. The transcriptional activity of other steroid hormone receptors is predominantly located in the activation function-2 (AF-2) region in the LBD. The NTD of AR, as well as other steroid hormone receptors, has not been crystalized. Thus, drug development to these largely disordered regions requires empirical testing of each drug candidate.
Current therapies targeting AR
Conventional therapy for advanced prostate cancer has focused on androgen-dependent activation of AR through its C-terminal LBD by either (1) androgen ablation or (2) antiandrogens that compete for the LBD to prevent binding of the endogenous ligand.
Androgen ablation
To reduce circulating levels of androgen, chemical (GnRH/LHRH analogs) or surgical castration have historically been the standard forms of therapy. Unfortunately, reduction of testicular androgen by these approaches does not completely eliminate tissue levels of androgen that can be detected in metastatic prostate cancer [2]. Measurement of residual androgen in prostate cancer tissue has led to suggestion that adrenal androgens or de novo synthesis of androgen by prostate cancer cells play contributing roles in failure to current treatments. Development of inhibitors of androgen synthesis has thus been renewed with abiraterone, an irreversible inhibitor of 17, 20 lyase/CYP17, recently approved by the FDA for patients who had received docetaxel. Abiraterone treatment in this patient group resulted in a 3.9 months survival advantage [3]. Other small molecules targeting androgen synthesis include ketoconazole, which has been used for many years but associated with toxicities, as well as investigational drugs TOK-001 (VN-124-1) and TAK-700 that are currently in clinical trials. In addition to inhibiting CYP17 to reduce synthesis of androgen, ketoconazole and TOK-001 are also reported to have antiandrogen activities (Fig. 1a). TOK-001 also inhibits the growth of cells not dependent upon AR or androgens for growth and survival, such as PC3 and DU145 with an IC50 ~7 μM by induction of the endoplasmic reticulum stress response [4]. Other effects of TOK-001 include decreased levels of AR [5]. Interestingly, no similar reports of degradation of AR or antiandrogen effects have been reported for abiraterone which has a similar structure (Fig. 1a). Bicalutamide [6] as well as a plethora of compounds not necessarily specific for AR have been reported to decrease the levels of AR through various mechanisms.
Antiandrogens
Antiandrogens currently used in the clinic include flutamide, bicalutamide, and nilutamide (Fig. 1b). Antiandrogens compete with androgen for the AR LBD to inhibit the transcriptional activity of the AR. Although each of these antiandrogens binds to the LBD, there are subtle differences observed between these molecules, which probably explains why each compound has shown additional therapeutic benefit despite that all bind to the same domain. Flutamide was the first developed pure antiandrogen [7], followed by nilutamide [8] and bicalutamide [9]. Preclinical assessment of these antiandrogens showed that they bound to the AR or prostate tissue and inhibited AR transcriptional activity as measured by reporter gene constructs, gene expression, and/or in vivo caused atrophy of androgen-dependent tissue and antitumor activity on prostate cancer tumors. Unfortunately, all of these antiandrogens eventually fail as indicated by rising levels of serum prostate-specific antigen (PSA) and return of clinical symptoms. PSA is a gene regulated by AR, thus re-expression of PSA indicates a transcriptional active AR in CRPC. Cessation of antiandrogens in these failing patients can paradoxically result in a decline of serum PSA and improvement, a phenomenon termed antiandrogen withdrawal syndrome. Although anywhere for 18–30% of patients are reported to display antiandrogen withdrawal, the mechanism is complex with the detection of gain-of-function mutations in the LBD associated with these antiandrogens being relatively rare such as mutations L874P and W741C/L. Rather these antiandrogens are thought to fail due to increased levels of AR and its coactivator proteins. Two families of AR interacting proteins are CREB-binding protein (CBP) and steroid receptor coactivator (SRC) which are elevated in CRPC tissues. All antiandrogens to date, including the investigational drug MDV3100, cause the normally cytoplasmic AR to translocate to the nucleus in the absence of androgen thereby placing the AR in a dangerous vicinity to promiscuously initiate transcription if cellular conditions exist such as elevated coactivators. In addition to nuclear translocation of the AR, bicalutamide also causes the AR to bind DNA at known androgen response elements (AREs) of target genes. Flutamide, bicalutamide, and nilutamide are partial agonists for AR, which in combination with their relatively low affinity for the AR as compared to the natural ligand, (i.e., dihydrotestosterone (DHT) which has 30-fold higher affinity than bicalutamide [10]) is thought to contribute to their clinical failure. This together with the recent discovery of residual levels of androgens in CRPC tissues supports the need for the development of antiandrogens with better affinity for the AR.
New antiandrogens
The relatively recent acceptance in the field that the AR remains transcriptional active in CRPC is based on the discovery of residual levels of androgen in CRPC tissue together with impressive clinical responses obtained with abiraterone in CRPC patients. These observations have renewed interest in developing more potent antiandrogens.
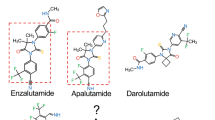
MDV3100 and RD162
MDV3100 is an antiandrogen with a similar structure to bicalutamide and was originally developed by using RU59063 as the chemical scaffold for structure activity relationship (SAR) studies (Fig. 1b). RD162 is structurally related to MDV3100 and shows similar properties to MDV3100 with IC50s for 18F-DHT-binding to AR of 30.9 ± 9.2 and 21.4 ± 4.4 nM, respectively, compared with 160 ± 29 for bicalutamide in cell-based assays [11]. Thus, RD162 and MDV3100 have improved affinities compared with bicalutamide. Inhibition of the expression of androgen-regulated genes and proliferation were also inhibited by RD162, albeit even better than MDV3100 which was unexpected in view of MDV3100 having better affinity for AR. RD162 had specificity for AR as compared to binding with PR and GR, but this was not provided for MDV3100. The inhibitory effect of MDV3100 and RD162 on androgen-dependent proliferation of VCaP prostate cancer cells was reversed by 1 nM synthetic androgen, R1881 [11]. These data may forecast failure of MDV and analogs in patients with residual levels of tissue androgens. In addition, confocal micrographs reveal that MDV3100 causes the majority of AR to become nuclear in the absence of androgens [11] which has been observed with other antiandrogens and thought to be important in the ultimate failure of these compounds. However, the ratio of nuclear to cytoplasmic AR obtained with MDV3100 is apparently less than fivefold that obtained with bicalutamide [11]. RD162 also caused some nuclear translocation of the AR with about equal levels in the cytoplasm and nucleus when examining confocal micrographs [11]. Strongly supporting that MDV3100 and RD162 have some differences to bicalutamide includes their inhibitory effect on the AR W741C mutant [11] that is resistant to inhibition by bicalutamide and originally discovered from a patient with antiandrogen withdrawal syndrome [12]. Both RD162 and MDV3100 cause apoptosis of VCaP cells while bicalutamide does not [11]. Transcriptional activity of the AR is inhibited by MDV3100 and RD162 as indicated by reduced endogenous expression of androgen-regulated genes, reporter gene assays, and androgen-dependent proliferation by a mechanism that involves competition for the LBD with androgen and decreased DNA-binding activity [11]. Pharmacokinetic parameters for RD162 are promising with a long half-life of 11.6 (iv) to 30.2 h (oral) and 47.4% bioavailability. In vivo, RD162 has impressive antitumor activity on LNCaP/AR-luc xenografts with regression of 12 tumors after 28 days. However, RD162 only slowed the growth of LAPC4/AR xenografts, while MDV3100 was not tested in this model [11]. Positive antitumour activity has been reported for MDV3100 in Phase 1–2 studies [13].
ARN-509
The Aragon drug ARN-509 is currently in Phase 1 clinical trials. Although no peer-reviewed data have been published, Aragon’s website states “ARN-509 is unique in its action in that it inhibits both AR nuclear translocation and AR binding to androgen response elements in DNA. Importantly, and in contrast to the first-generation anti-androgen bicalutamide, it exhibits no agonist activity in prostate cancer cells that over-express AR.” It will be interesting to see how this antiandrogen’s mechanism differs from MDV3100 and whether it can achieve any additional clinical benefit.
BMS-641988
Preclinical studies with the antiandrogen BMS-641988 inhibited the growth of prostate cancer cells in vitro and had cytostatic effect on xenografts [14]. The metabolite, BMS-501949 caused seizures in dogs although no seizures were observed with the parent compound [15]. Phase I studies of sixty-one patients with CRPC treated daily with BMS-641988 had outcomes of stable disease and partial agonism as predicted from preclinical studies [15]. Due to the limited antitumor activity and seizures, the study was closed [15].
AR LBD allosteric antagonists
Three nonsteroidal anti-inflammatory drugs, flufenamic acid, 3,3′,5-triiodothyroacetic acid, and triiodothyronine (Fig. 1c), were discovered using a fluorescence polarization (FP) screen to initially find compounds that inhibited interaction between the AF-2 region in the LBD with 15 amino acid residues encoding the LXXLL sequence of SRC2 known to interact with AF-2 followed by X-ray screens [16]. The studies revealed a previously unknown regulatory surface cleft, binding function (BP)-3 that was proposed to be an allosteric regulatory site required for AR activity. Binding of 3,3′,5-triiodothyroacetic acid to BP-3 was shown by X-ray structure analysis to remodel the adjacent interaction site on AF-2 thereby reducing coactivator binding [16]. These compounds were required at high concentrations to block interactions with recombinant proteins (~50 μM), but inhibited reporter assays between 10 and 30 μM in cell-based assays [16]. Specificity was not addressed but since these compounds are ligands of thyroid receptor, off-target effects would be expected. Further chemistry to develop specific BP-3 inhibitors could provide a novel approach to block ligand-activated AR.
Gesolin is a coactivator of the AR that interacts with the AR DBD and LBD [17]. D36 and D80 were identified (Fig. 1c) as novel allosteric antagonists of the AR by using a mammalian two-hybrid screen to measure interaction between VP16-AR and Gal4DBD-gelsolin fusion protein, followed by MMTV-luciferase reporter assays [18]. A Ki of 9.0 ± 0.37 and 17.0 ± 0.86 μM for D36 and D80, respectively, were calculated [18]. Both compounds effectively competed for 3H-R1881 with IC50s of 10 and 34 μM for D36 and D80, respectively [18]. Surface plasmon resonance using both full-length AR and LBD revealed D36 bound LBD with same affinity as full-length AR (Kd = 90 μM), while D80 had reduced binding to solely the LBD as compared to full-length AR (Kd = 40 μM) [18]. Importantly, binding of both compounds was independent of saturating agonist thereby supporting that these compounds do not bind to the ligand-binding pocket. In vitro, both compounds inhibited proliferation of commonly used prostate cancer cells that express AR. Neither compound caused nuclear translocation of the AR or DNA-binding activity in the absence of androgen. No studies were shown to provide evidence for specificity or negligible off-targets.
Antagonists of unknown AR domain
Pyrvinium pamoate and harmolhydrochloride (Fig. 1d) inhibit AR conformation in living cells [19]. The binding site on the AR is unknown, although they do not compete with hydroxyflutamide or DHT thereby suggesting they do not bind to the ligand-binding pocket in the LBD. IC50s using reporter gene constructs were impressive in the nM range. Chromatin immunoprecipitation experiments revealed that pyrvinium pamoate had no effect on blocking androgen-induced AR recruitment to AREs, while harmol hydrochloride did block this interaction [19]. Both compounds reduced RNA polymerase II recruitment and had some effect on blocking androgen-dependent proliferation of LNCaP cells without effects on HEK293 cells in vitro [19]. Harmol hydrochloride was quickly metabolized and not assessed in vivo. Plasma concentrations of pyrvinium pamoate ranged between 150 and 20 nM using a once daily i.p. regime of 1 mg/kg body weight [19]. After 4 weeks of treatment, no effect was observed on the weights of prostate with solely pyrvinium pamoate in spite of repression of some androgen-regulated genes. However, a combination of pyrvinium pamoate with bicalutamide resulted in a 63% decrease in prostate weight compared to 35% with bicalutamide alone [19].
AR NTD allosteric antagonists
The AR NTD contains the AF-1 that contributes most of the activity to the ligand-bound AR and contributes all of the activity to AR activated by alternative pathways in the absence of ligand [20, 21]. Recently, naturally occurring splice variants of the AR that lack the LBD have been reported in prostate cancer cell lines and also in CRPC [22–25]. These mutants are constitutively active and would not be inhibited by current therapies that target the AR LBD such as antiandrogens and androgen ablation therapy. Proof-of-concept that targeting the AR NTD blocks in vivo prostate cancer tumor growth in the presence (androgen sensitive) and absence of androgens (CRPC) was shown by decoy molecules encoding the 558 amino acid residues of the AR NTD [26].
AR AF-1 has characteristics of a collapsed disordered region meaning that it is predicted to have some proportion of secondary structure, but not a stable tertiary structure. To date, very few small molecule inhibitors of intrinsically disordered proteins have been discovered, and contrary to intuition that they should be large and bulky molecules, those discovered tend to be relatively small in size (Fig. 2a; for a review see [27]). The limited structure of the AR NTD is thought to require interactions with other proteins to assume correct folding for further protein–protein interactions including interactions with bridging factors and the basal transcriptional machinery to result in active transcription. However, because of this high degree of intrinsic disorder and lack of a solved crystal structure, it is not possible to be used for structure-based drug design. Instead, screening assays are required that test each drug empirically. Using a cell-based screen, two structurally unrelated small molecules, EPI-001 and SINT1 (sintokamide), that inhibit transactivation of the AR NTD have recently been reported (Fig. 2b).
SINT1 is a novel structure that was isolated from an extract of Dysidea sp. sponge collected in Indonesia. SINT1 (5 ug/ml) blocks AR transcriptional activity induced by androgen and androgen-induced proliferation of LNCaP cells without affecting the proliferation of PC3 cells that do not depend on AR for growth [28]. Transactivation of the AR NTD can be induced by forskolin that stimulates the PKA pathway or by interleukin-6 [20, 21]. SINT1 reduced forskolin-induced transactivation of AR NTD to baseline levels [28]. Further studies are required to verify specificity and in vivo efficacy.
An analog of EPI-001 was first isolated from the marine sponge Geodia lindgreni collected in Papua New Guinea. Approximately 20 analogs were tested in cell-based assays to obtain additional SAR for the pharmacophore. The compound EPI-001 had the most potent activity with an IC50 of 6 μM for blocking transactivation of the NTD [29]. EPI-001 was found to: inhibit AR activity and block transactivation of the AR NTD; have specificity to the AR and did not inhibit related steroid receptors; block androgen-induced proliferation without effects on proliferation of cells not dependent on AR for growth; inhibit expression of endogenous genes regulated by AR; prevent AR interaction with AREs of target genes in response to androgen; and inhibit a constitutively active AR lacking the LBD [29]. The mechanism of action involves EPI-001 binding AF-1 to alter its conformation and prevent essential interaction with CBP and N/C interaction that are required for transcriptional activity [29]. In vivo, EPI-001 (50 mg/kg body weight) delivered intravenously blocked the growth of androgen-dependent and CRPC xenografts, as well as reduced the weight of benign prostate in non-castrated hosts, without any apparent toxicity. Fourteen days after the first injection, EPI-001 caused regression of LNCaP xenografts in 8 of 10 animals between 11 and 66% (mean = 33 ± 18%) [29] which is comparable to the 10–40% regression reported in a very small number of animals (n = 4) after 28 days of treatment with MDV3100 also in LNCaP xenografts [11]. Analogs of EPI-001 are currently in development for clinical trials.
Advantages of AR NTD antagonists
All hormonal therapies in the clinic and in clinical trials target AR LBD directly with antiandrogens or indirectly by reducing ligand (Fig. 3a). Unfortunately, all of these therapies eventually fail by mechanisms thought to involve constitutively active splice variants of the AR, breakthrough of androgen/steroid blockade, increased expression of AR and coactivators, and/or rarely including gain-of-function mutations in the LBD. Although no long-term studies have been reported for EPI-001, there is low potential for gain-of-function point mutations to develop because the AR NTD is intrinsically disordered. Importantly, failure of current hormonal therapies is considered to still involve transcriptionally active AR species. Rationale for blocking the AR NTD is based on AF-1 being located in this business end of the molecule and AF-1 is absolutely essential for transcriptional activity by a mechanism that involves protein–protein interactions. Thus, inhibitors of the NTD should block the activities of all AR species regardless of ligand, something that antiandrogens, castration, and CYP17 inhibitors cannot achieve.
Advantages of NTD inhibitors. a EPI-001 binds to the NTD to block transactivation of AR through AF-1. All current therapies target the AR LBD either by reducing androgen (androgen ablation) or by application of antiandrogens (AA). b EPI-001 inhibits essential protein–protein interactions with CBP, RAP-74 (subunit of TFIIF), and N/C. c EPI-001 does not cause AR to bind AREs on the DNA in the absence of androgen and in the presence of androgen blocks interaction of ligand-bound AR with AREs. d EPI-001 inhibits AR splice variants lacking the LBD
Based upon the results reported with EPI-001, advantages of an NTD inhibitor include: (1) it does not cause nuclear translocation of the AR in the absence of ligand contrary to all antiandrogens; (2) it does not cause the AR to bind AREs unlike bicalutamide (Fig. 3b); (3) it inhibits protein–protein interactions that are necessary for transcription such as CBP, RAP-74, and N/C interactions (Fig. 3c); and (4) it is the only known inhibitor of constitutively active AR splice variants that lacks the LBD (Fig. 3d). AR constitutively active splice variant, v567es, lacks the LBD and is solely expressed in 20% of metastases obtained from CRPC patients [24]. Expression of AR splice variants is increased in CRPC bone metastases and is associated with poor prognosis [25]. Blocking the LBD or decreasing the levels of androgen would have no effect on the activities of these AR variants present in CRPC metastases.
Conclusions
The dependence of CRPC on transcriptionally active AR by the mechanisms involving residual androgens, constitutively active splice variants lacking LBD, increased expression of AR and coactivators, and alternative signaling pathways has resurged the interest in developing small molecule inhibitors to AR or androgen axis. Importantly, discovery of these mechanisms of CRPC has revealed targets for drug development that include blocking androgen synthesis and targeting domains other than the ligand-binding pocket of AR LBD. Development of small molecule inhibitors of AR that work through different mechanisms should each translate into clinical benefit as already shown for the battery of antiandrogens currently used in the clinic.
References
Poujol N, Wurtz JM, Tahiri B, Lumbroso S, Nicolas JC, Moras D, Sultan C (2000) Specific recognition of androgens by their nuclear receptor. A structure-function study. J Biol Chem 275:24022–24031
Montgomery RB, Mostaghel EA, Vessella R, Hess DL, Kalhorn TF, Higano CS, True LD, Nelson PS (2008) Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res 68:4447–4454
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, Chi KN, Jones RJ, Goodman OB Jr, Saad F, Staffurth JN, Mainwaring P, Harland S, Flaig TW, Hutson TE, Cheng T, Patterson H, Hainsworth JD, Ryan CJ, Sternberg CN, Ellard SL, Fléchon A, Saleh M, Scholz M, Efstathiou E, Zivi A, Bianchini D, Loriot Y, Chieffo N, Kheoh T, Haqq CM, Scher HI, COU-AA-301 Investigators (2011) Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 364:1995–2005
Bruno RD, Gover TD, Burger AM, Brodie AM, Njar VC (2008) 17alpha-Hydroxylase/17, 20 lyase inhibitor VN/124–1 inhibits growth of androgen-independent prostate cancer cells via induction of the endoplasmic reticulum stress response. Mol Cancer Ther 7:2828–2836
Vasaitis T, Belosay A, Schayowitz A, Khandelwal A, Chopra P, Gediya LK, Guo Z, Fang HB, Njar VC, Brodie AM (2008) Androgen receptor inactivation contributes to antitumor efficacy of 17{alpha}-hydroxylase/17, 20-lyase inhibitor 3beta-hydroxy-17-(1H-benzimidazole-1-yl) androsta-5,16-diene in prostate cancer. Mol Cancer Ther 7:2348–2357
Waller AS, Sharrard RM, Berthon P, Maitland NJ (2000) Androgen receptor localisation and turnover in human prostate epithelium treated with the antiandrogen, casodex. J Mol Endocrinol 24:339–351
Neri RO, Monahan MD, Meyer JG, Afonso BA, Tabachnick IA (1967) Biological studies on an anti-androgen (SH 714). Eur J Pharmacol 1:438–444
Moguilewsky M, Fiet J, Tournemine C, Raynaud JP (1986) Pharmacology of an antiandrogen, anandron, used as an adjuvant therapy in the treatment of prostate cancer. J Steroid Biochem 24:139–146
Furr BJ, Valcaccia B, Curry B, Woodburn JR, Chesterson G, Tucker H (1987) ICI 176, 334: a novel non-steroidal, peripherally selective antiandrogen. J Endocrinol 113:R7–R9
Kolvenbag GJ, Blackledge GR, Gotting-Smith K (1998) Bicalutamide (Casodex) in the treatment of prostate cancer: history of clinical development. Prostate 34:61–72
Tran C, Ouk S, Clegg NJ, Chen Y, Watson PA, Arora V, Wongvipat J, Smith-Jones PM, Yoo D, Kwon A, Wasielewska T, Welsbie D, Chen CD, Higano CS, Beer TM, Hung DT, Scher HI, Jung ME, Sawyers CL (2009) Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science 324:787–790
Yoshida T, Kinoshita H, Segawa T, Nakamura E, Inoue T, Shimizu Y, Kamoto T, Ogawa O (2005) Antiandrogen bicalutamide promotes tumor growth in a novel androgen-dependent prostate cancer xenograft model derived from a bicalutamide-treated patient. Cancer Res 65:9611–9616
Scher HI, Beer TM, Higano CS, Anand A, Taplin ME, Efstathiou E, Rathkopf D, Shelkey J, Yu EY, Alumkal J, Hung D, Hirmand M, Seely L, Morris MJ, Danila DC, Humm J, Larson S, Fleisher M, Sawyers CL, Prostate Cancer Foundation/Department of Defense Prostate Cancer Clinical Trials Consortium (2010) Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1–2 study. Lancet 375:1437–1446
Attar RM, Jure-Kunkel M, Balog A, Cvijic ME, Dell-John J, Rizzo CA, Schweizer L, Spires TE, Platero JS, Obermeier M, Shan W, Salvati ME, Foster WR, Dinchuk J, Chen SJ, Vite G, Kramer R, Gottardis MM (2009) Discovery of BMS-641988, a novel and potent inhibitor of androgen receptor signaling for the treatment of prostate cancer. Cancer Res 69:6522–6530
Rathkopf D, Liu G, Carducci MA, Eisenberger MA, Anand A, Morris MJ, Slovin SF, Sasaki Y, Takahashi S, Ozono S, Fung NK, Cheng S, Gan J, Gottardis M, Obermeier MT, Reddy J, Zhang S, Vakkalagadda BJ, Alland L, Wilding G, Scher HI, Prostate Cancer Clinical Trials Consortium (2011) Phase I dose-escalation study of the novel antiandrogen BMS-641988 in patients with castration-resistant prostate cancer. Clin Cancer Res 17:880–887
Estébanez-Perpiñá E, Arnold LA, Nguyen P, Rodrigues ED, Mar E, Bateman R, Pallai P, Shokat KM, Baxter JD, Guy RK, Webb P, Fletterick RJ (2007) A surface on the androgen receptor that allosterically regulates coactivator binding. Proc Natl Acad Sci USA 104:16074–16079
Nishimura K, Ting HJ, Harada Y, Tokizane T, Nonomura N, Kang HY, Chang HC, Yeh S, Miyamoto H, Shin M, Aozasa K, Okuyama A, Chang C (2003) Modulation of androgen receptor transactivation by gelsolin: a newly identified androgen receptor coregulator. Cancer Res 63:4888–4894
Joseph JD, Wittmann BM, Dwyer MA, Cui H, Dye DA, McDonnell DP, Norris JD (2009) Inhibition of prostate cancer cell growth by second-site androgen receptor antagonists. Proc Natl Acad Sci USA 106:12178–12183
Jones JO, Bolton EC, Huang Y, Feau C, Guy RK, Yamamoto KR, Hann B, Diamond MI (2009) Non-competitive androgen receptor inhibition in vitro and in vivo. Proc Natl Acad Sci USA 106:7233–7238
Sadar MD (1999) Androgen-independent induction of prostate-specific antigen gene expression via cross-talk between the androgen receptor and protein kinase a signal transduction pathways. J Biol Chem 274:7777–7783
Ueda T, Bruchovsky N, Sadar MD (2002) Activation of the androgen receptor N-terminal domain by interleukin-6 via MAPK and STAT3 signal transduction pathways. J Biol Chem 277:7076–7085
Guo Z, Yang X, Sun F, Jiang R, Linn DE, Chen H, Chen H, Kong X, Melamed J, Tepper CG, Kung HJ, Brodie AM, Edwards J, Qiu Y (2009) A novel androgen receptor splice variant is up-regulated during prostate cancer progression and promotes androgen depletion-resistant growth. Cancer Res 69:2305–2313
Hu R, Dunn TA, Wei S, Isharwal S, Veltri RW, Humphreys E, Han M, Partin AW, Vessella RL, Isaacs WB, Bova GS, Luo J (2009) Ligand-independent androgen receptor variants derived from splicing of cryptic exons signify hormone-refractory prostate cancer. Cancer Res 69:16–22
Sun S, Sprenger CC, Vessella RL, Haugk K, Soriano K, Mostaghel EA, Page ST, Coleman IM, Nguyen HM, Sun H, Nelson PS, Plymate SR (2010) Castration resistance in human prostate cancer is conferred by a frequently occurring androgen receptor splice variant. J Clin Invest 120:2715–2730
Hörnberg E, Ylitalo EB, Crnalic S, Antti H, Stattin P, Widmark A, Bergh A, Wikström P (2011) Expression of androgen receptor splice variants in prostate cancer bone metastases is associated with castration-resistance and short survival. PLoS One 6:e19059
Quayle SN, Mawji NR, Wang J, Sadar MD (2007) Androgen receptor decoy molecules block the growth of prostate cancer. Proc Natl Acad Sci USA 104:1331–1336
Metallo SJ (2010) Intrinsically disordered proteins are potential drug targets. Curr Opin Chem Biol 14:481–488
Sadar MD, Williams DE, Mawji NR, Patrick BO, Wikanta T, Chasanah E, Irianto HE, Soest RV, Andersen RJ (2008) Sintokamides A to E, chlorinated peptides from the sponge Dysidea sp. that inhibit transactivation of the N-terminus of the androgen receptor in prostate cancer cells. Org Lett 10:4947–4950
Andersen RJ, Mawji NR, Wang J, Wang G, Haile S, Myung JK, Watt K, Tam T, Yang YC, Bañuelos CA, Williams DE, McEwan IJ, Wang Y, Sadar MD (2010) Regression of castrate-recurrent prostate cancer by a small-molecule inhibitor of the amino-terminus domain of the androgen receptor. Cancer Cell 17:535–546
Acknowledgments
This work was supported by grants from the Canadian Institutes of Health Research (MOP-79308, PPP-102189) and the US National Cancer Institute (2R01 CA105304).
Conflict of interest
MDS receives compensation from ESSA Pharma Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sadar, M.D. Advances in small molecule inhibitors of androgen receptor for the treatment of advanced prostate cancer. World J Urol 30, 311–318 (2012). https://doi.org/10.1007/s00345-011-0745-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-011-0745-5