Abstract
Purpose
Interest in laparoendoscopic single-site (LESS) surgery has increased in recent years. The aim of this study was to evaluate the feasibility and safety of transumbilical LESS adrenalectomy and to elucidate the technical differences between LESS and conventional laparoscopic surgery.
Methods
This study was comparing 10 consecutive transumbilical LESS adrenalectomies and 10 conventional laparoscopic adrenalectomies performed between March 2006 and April 2010 for benign adrenal tumors. Perioperative parameters were compared, and we reviewed our surgical videos and analyzed technical characteristics of the surgeries.
Results
There was no open conversion in laparoscopic group, no additional port placement in LESS group, and no perioperative complications in either group. No significant differences in operative time, estimated blood loss, or resumption of oral intake were observed between two groups. Pneumoperitoneum time did not differ between LESS and laparoscopic groups (91.2 vs. 74.3 min, P = 0.257). In LESS group only, time was needed for adjustment of roticulator (14.5 ± 8.1 min). After subtracting the time needed for adjustment, operative time between two groups was more comparable (76.7 vs. 74.3 min, P = 0.880). One-handed manipulation time in LESS group decreased in a time-dependent manner (r = −0.806, P < 0.0049). Tissue re-grasping during operation was more frequently observed in LESS group (16.2 vs. 2.2 times, P < 0.001).
Conclusions
Transumbilical LESS adrenalectomy is feasible and comparable to conventional laparoscopic adrenalectomy. There are still obvious technical difficulties associated with LESS surgery, and it is essential that these be overcome in order to improve this surgical technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Various types of tumors, both benign and malignant, occur in the adrenal gland, and open surgery requires a large incision and has anatomical difficulties with respect to approach. Since laparoscopic adrenalectomy was first reported in 1992 by Ganger et al. [1], and this surgical procedure has become a widely accepted mode of treatment for adrenal tumors. Several studies have compared laparoscopic adrenalectomy with open adrenalectomy, documenting decreased complications, a shorter postoperative hospital stay, and reduced costs of the laparoscopic approach [2–5]. Therefore, laparoscopic surgery is becoming the gold standard for adrenalectomy.
Current laparoscopic techniques require at least 3 ports to complete laparoscopic surgery. Although laparoendoscopic single-site (LESS) surgery has been reported for cholecystectomy [6] and appendectomy [7] since 1998, the approach has not gained momentum because of its technical difficulties. However, these challenges have been minimized by advancements in laparoscopic instruments, mainly through the introduction of flexible 5-mm laparoscopes with excellent image display and flexible/bent instruments [8].
We attempted to determine the technical differences between LESS and conventional laparoscopic adrenalectomy by examining our surgical results and videos taken during surgery.
Materials and methods
This was a retrospective case–control study comparing the experience of a single surgeon (A.M.) with 10 consecutive transumbilical LESS adrenalectomies (cases) performed between December 2009 and April 2010 and 10 consecutive conventional laparoscopic adrenalectomies performed between March 2006 and October 2009 (controls). Data were collected prospectively following Institutional Review Board approval.
The conventional laparoscopic adrenalectomy technique has been described previously [9]. A multichannel port (SILS™ port), bent laparoscopic instrument (Roticulator Endo Grasp™), and Opti4™ laparoscopic electrodes were obtained from Covidien (Mansfield, MA, USA). The SILS™ port was placed through a 2-cm incision at the inner edge of the umbilicus. The anterior rectus fascia was sharply incised, and four corner fascial stay sutures were placed. A 5-mm flexible laparoscope (Olympus Surgical, Tokyo) was introduced to keep the scope away from the operator’s instruments, and it enabled the operator to perform manipulations in a wide working space and to avoid “sword fighting”. Bent instruments were required to create the operative angle because these insertion points were quite close to each other. The adrenal vein was controlled with at least two Ligamax™ (Ethicon Endo-Surgery, OH, USA) proximally and one distally. The specimen was extracted using an EndoCatch™ bag (Covidien). We did not need to extend the umbilical incision to remove adrenal specimens. Hemostasis was carefully maintained, and no drainage tubes were left in any of the cases. The fascial incisions were closed with absorbable suture, and the umbilicus was restored to its original state with absorbable cutaneous stitches. In right LESS adrenalectomies, we introduced an additional 2-mm needle port to just lift up the liver. To prevent injury to the liver, gauze was placed at the tip of the narrow forceps.
The primary aim of this study was to evaluate the feasibility and safety of LESS adrenalectomy. Therefore, various parameters, including age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) class risk, operative side, perioperative complications, operative time, estimated blood loss, resumption of oral intake, and length of hospital stay, were collected.
The secondary aim was to compare the technical differences between LESS and conventional laparoscopic adrenalectomy. For this purpose, we reviewed our surgical videos and analyzed the technical characteristics of the surgeries.
Differences in clinical and surgical results were examined using the Mann–Whitney U-test for continuous variables and the chi-square test for categorical variables. The correlation between the proportion of one-handed manipulation time and the operative experiences was assessed with Spearman correlation analysis. All P-values were two-sided, and data were considered statistically significant at P < 0.05.
Results
Patient characteristics are summarized in Table 1. No significant differences in sex, age, BMI, ASA class risk, or operative side were observed between the groups.
Table 2 shows the surgical outcomes for patients undergoing LESS or conventional laparoscopic adrenalectomy. There was no conversion to open surgery in the conventional laparoscopic group nor additional port placement in the LESS group. No significant differences were observed in mean total operative time (from insertion of port to skin closure) (125.2 vs. 119.7 min, P = 0.678), estimated blood loss (12.4 vs. 15.3 ml, P = 0.849), and resumption of oral intake (1 vs. 1 day, P = 1.000) between the LESS group and conventional laparoscopy group. The number of postoperative hospital days was significantly shorter in the LESS group, with a mean of 5.2 days (range 4–6 days), compared with 6.9 days (range 5–12 days) in the conventional laparoscopic group (P = 0.028). Tumor size was larger, but not significantly, in the conventional laparoscopic group than in the LESS group (2.8 vs. 4.5 cm in diameter, P = 0.087).
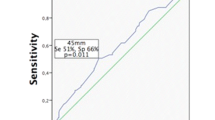
Pneumoperitoneum time (from introduction to removal of endoscope) did not differ between the LESS and laparoscopic groups (91.2 vs. 74.3 min, P = 0.257) (Fig. 1). In the LESS group, time was needed to adjust the roticulator (14.5 ± 8.1 min). If the time for this adjustment was subtracted, the operative time between the two groups was comparable (76.7 vs. 74.3 min, P = 0.880). The ratio of the time for adjustment of the roticulator to the pneumoperitoneum time was almost constant. In the conventional laparoscopic group, most of the operative manipulation was two-handed, while one-handed manipulation was performed more often in the LESS group (Fig. 2). The one-handed manipulation time in the LESS group gradually decreased as the number of surgical experiences increased (r = −0.806, P < 0.0049). Tissue re-grasping during an operation was more frequently observed in the LESS group than in the conventional laparoscopic group (16.2 vs. 2.2 times, P < 0.001).
Learning curve for the proportion of time for one-handed manipulation. Solid line represents LESS adrenalectomy. Dotted line represents the latest 10 conventional laparoscopic adrenalectomy cases. The one-handed manipulation time in the LESS group gradually decreased as the number of surgical experiences increased (r = −0.806, P < 0.0049)
Comments
LESS surgery has become quite widely used in the treatment of urological diseases in recent years, and several reports have demonstrated its feasibility as well as safety that is equivalent to that of conventional laparoscopic surgery [10–12]. Although these studies compared operative outcomes such as operative time, transfusion rate, and complication rate between LESS and conventional laparoscopic surgery, no report has discussed technical differences between the two procedures. However, the improvement in surgical devices, such as flexible endoscopes and bent instruments, has made it easier to perform LESS surgery, although various technical difficulties associated with the surgery still remain. Therefore, in this study, we performed a case–control comparison by analyzing the technical features of transumbilical LESS and conventional laparoscopic adrenalectomy.
No differences in total operative time, estimated blood loss, or resumption of oral intake were observed between the LESS group and conventional laparoscopic group. Because the clinical pathway for laparoscopic adrenalectomy was revised and the postoperative hospital stay was shortened from October 2007, the average number of postoperative hospital days in the conventional laparoscopic group was longer than in the LESS group. Although this study included only 10 LESS cases, there was no conversion to conventional laparoscopic surgery or perioperative complications. These results indicate that LESS adrenelectomy is both feasible and comparable to conventional laparoscopic adrenalectomy.
The difference in pneumoperitoneum time between the LESS group and the conventional laparoscopic group was not statistically significant, although the average time in the LESS group was longer than in the conventional group. We focused on this discrepancy and attempted to elucidate the technical differences between these two methods that are strongly correlated with technical difficulties. The difficulties encountered in LESS surgery mainly arise from the “sword fighting” of the instruments [13] (Fig. 3a), and we can reduce this “fighting” by using bent instruments. However, the angle of the bent instruments needs to be adjusted, and these maneuvers require quite a bit of time. In our study, the operative time was almost the same in the two groups if the time needed to adjust the roticulator was subtracted. In endoscopic surgery, one hand performs dissection while the other hand performs traction, thus making it necessary to coordinate bimanual motions. Even though bent instruments have been introduced, the sword fighting problem is still an obstacle in LESS surgery. In the early phase of our experience with LESS adrenalectomy, one-handed manipulation (Fig. 3b) required a certain amount of time in order to avoid the sword fighting, but the time has gradually decreased as our experience has increased. Because the distance from the port to the tissue in the transumbilical approach is longer than in the conventional laparoscopic approach, the approach becomes more tangential in direction in LESS surgery (Fig. 3c, d). The different angle of approach of the instrument definitely feels different compared with conventional laparoscopic surgery, and there is a tendency to grasp the second- or third-best site because it is difficult to approach the target tissue in a straightforward manner (Fig. 3e). This might contribute to an increase in tissue re-grasping due to the inadequate or insufficient counter-traction. Furthermore, because the gripping power of the roticulator grasp was not sufficiently strong to keep grasping the tissue, improved instruments in which the tissue does not slip out of the roticulator are needed.
“Sword fighting” of instruments (a) and one-handed manipulation (b). Side view schematic of the conventional laparoscopic surgery (c) and transumbilical LESS (d). Difficulties encountered concerning the approach to the optimal site of grasping (e). The forceps crossed the other instrument and grasped the site that could not provide the optimal counter retraction
This study has several limitations. First, it is a retrospective study and is therefore susceptible to all limitations and biases inherent in a retrospective design. Second, the conventional laparoscopic group included larger tumors and more pheochromocytomas than the LESS group. A training system for laparoscopic surgery has been developed at our institution [14], and many conventional laparoscopic adrenalectomies are performed by residents. Therefore, only the difficult cases, such as large tumors and pheochromocytomas, are performed by our experienced laparoscopic surgeon. Nevertheless, we operated on two cases with a high BMI (30.2 and 33.8 kg/cm2) and two cases of pheochromocytoma using LESS adrenalectomy. These results suggest that virtually the same surgical indications may be applied for LESS adrenalectomy and conventional laparoscopic adrenalectomy when the operation is performed by an experienced laparoscopic surgeon.
We evaluated the feasibility and safety of LESS adrenalectomy and have elucidated some technical differences. These differences must be overcome in order to improve LESS surgery. Since transumbilical LESS surgery has advantages, such as scars that are only barely visible, that improve the quality of life of the patient, we are confident that further improvements to this procedure will lead to an expanded indication for this surgery.
References
Gagner M, Lacroix A, Bolté E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327:1033
Bonjer HJ, Lange JF, Kazemier G, de Herder WW, Steyerberg EW, Bruining HA (1997) Comparison of three techniques for adrenalectomy. Br J Surg 84:679–682
Guazzoni G, Montorsi F, Bocciardi A, Da Pozzo L, Rigatti P, Lanzi R, Pontiroli A (1995) Transperitoneal laparoscopic versus open adrenalectomy for benign hyperfunctioning adrenal tumors: a comparative study. J Urol 153:1597–1600
Schell SR, Talamini MA, Udelsman R (1999) Laparoscopic adrenalectomy for nonmalignant disease: improved safety, morbidity, and cost-effectiveness. Surg Endosc 13:30–34
Winfield HN, Hamilton BD, Bravo EL, Novick AC (1998) Laparoscopic adrenalectomy: the preferred choice? A comparison to open adrenalectomy. J Urol 160:325–329
Piskun G, Rajpal S (1999) Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A 9:361–364
Esposito C (1998) One-trocar appendectomy in pediatric surgery. Surg Endosc 12:177–178
Kaouk JH, Haber GP, Goel RK, Desai MM, Aron M, Rackley RR, Moore C, Gill IS (2008) Single-port laparoscopic surgery in urology: initial experience. Urology 71:3–6
Suzuki K, Kageyama S, Ueda D, Ushiyama T, Kawabe K, Tajima A, Aso Y (1993) Laparoscopic adrenalectomy: clinical experience with 12 cases. J Urol 150:1099–1102
Raman JD, Bagrodia A, Cadeddu JA (2009) Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol 55:1198–1204
Jeong BC, Park YH, Han DH, Kim HH (2009) Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol 23:1957–1960
Park YH, Park JH, Jeong CW, Kim HH (2010) Comparison of laparoendoscopic single-site radical nephrectomy with conventional laparoscopic radical nephrectomy for localized renal-cell carcinoma. J Endourol 24:997–1003
Tracy CR, Raman JD, Cadeddu JA, Rane A (2008) Laparoendoscopic single-site surgery in urology: where have we been and where are we heading? Nat Clin Pract Urol 5:561–568
Miyajima A, Hasegawa M, Takeda T, Tamura K, Kikuchi E, Nakagawa K, Oya M (2010) How do young residents practice laparoscopic surgical skills? Urology 76:352–356
Conflict of interest
The authors declare that they have no conflict of interest in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ishida, M., Miyajima, A., Takeda, T. et al. Technical difficulties of transumbilical laparoendoscopic single-site adrenalectomy: comparison with conventional laparoscopic adrenalectomy. World J Urol 31, 199–203 (2013). https://doi.org/10.1007/s00345-010-0636-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-010-0636-1