Abstract
Purpose
To evaluate the postoperative and functional results of the laparoscopic dismembered pyeloplasty (LDP).
Patients and methods
Between May 2000 and April 2008, we performed in our department 105 LDP. All patients presented an ureteropelvic junction obstruction with dilatation of renal calyx system with an enlarged renal pelvis. Demographic data (age, gender), perioperative and postoperative parameters, including operating time, estimated blood loss, complications, length of hospital stay, functional outcome were collected and evaluated.
Results
The mean operative time for LDP was 150 min (range 120–180 min) and the mean estimated blood loss was negligible in all patients. The mean hospital stay was 4 days (4–8). No conversion to open surgery occurred. In the follow-up, we noted a successful rate in 96.2% of the patients.
Conclusion
Laparoscopic dismembered pyeloplasty, if performed by expert surgeons in high-volume centres, presents results that are comparable with open surgery, with a lower surgical trauma for the patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the early 1990s, laparoscopic techniques have undergone a dramatic development in urology and other surgical disciplines. Today, euphoria is giving way to a more sober approach to a concrete evaluation of the benefits for the patient. The idea behind the application of a minimally invasive technique such as laparoscopy is to achieve the same result with the same safety for the patient and less traumatization when compared to open surgical procedures [1]. Since first described by Schuessler et al. in 1993, laparoscopic pyeloplasty has emerged as a valid technique to correct ureteropelvic junction obstruction (UPJO), with a success rate of more than 90% [2]. In this study, we describe our technique and report our results in 105 patients who underwent a laparoscopic dismembered pyeloplasty (LDP) for UPJO.
Patients and methods
Between May 2000 and April 2008, we performed in our department 105 LDP. All patients presented an UPJO with dilatation of renal calyx system with an enlarged renal pelvis. The preoperative diagnosis included a detailed anamnesis with particular attention to the nature of pain, sonography, excretory urography, renal scintigraphy and retrograde pyelography with placement of a double-J stent just before the operation. Demographic data (age, gender), perioperative and postoperative parameters, including operating time, estimated blood loss, complications, length of hospital stay, functional outcome were collected and evaluated. Data were expressed as mean ± standard deviation (SD) and statistical significance was accepted at p < 0.05. Statistical analysis was performed using SigmaPlot® software version 13.0 (SPSS Inc., Chicago, IL, USA) and Graphpad Prism 5 (Graphpad Software, CA, USA).
All surgical procedures were performed by two surgeons (P.F., F.G.) who had completed at least 40 LDP each before the beginning of the study, thus reducing the learning-curve effect.
Patients with previous abdominal surgeries were excluded from this study.
Surgical technique
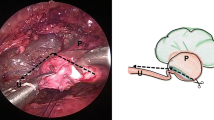
Following the induction of general anaesthesia, a cystoscopy and retrograde pyelography were performed in each patient and a 7 F double-J stent was placed. A nasogastric tube and transurethral catheter were inserted to decompress the stomach and bladder. The patients were secured to the operating table in a full flank position. In all patients, a transperitoneal approach was used. A Veress needle was inserted periumbilically to establish the pneumoperitoneum using carbon dioxide. With an initial intra-abdominal pressure of 12–15 mmHg, a 12-mm trocar was placed supraumbilically after removal of the Veress needle. The endoscopic 0° camera is introduced and after inspection of the abdominal cavity three other trocars were inserted under direct vision: two 12-mm trocars in the ipsilateral mid-clavicular line and a 10-mm trocar were placed just between the xyphoid and the first port. Occasionally, a fifth trocar (5-mm) was used in the anterior axillary line below the umbilicus. Then, the intra-abdominal pressure was lowered to 10–12 mmHg and maintained at this level. The peritoneum was incised along the Toldt’s line using electrosurgical scissors and grasping forceps. After mobilization of the colon, the ureter was identified above its cross over the iliac vessels. The proximal ureter and the renal pelvis were completely mobilized (Fig. 1). The renal pelvis was dismembered with the proximal ureter and the stenotic segment was resected. Then the ureter was medially spatulated (Fig. 2). The renal pelvis was reduced, removing the enlarged segment. If crossing vessels were presented, the ureter and the renal pelvis were transposed ventrally. Then the anastomosis was performed with interrupted 4-0 vicryl sutures, starting from the deepest point of the spatulated ureter and from both flap corners of its end with the corresponding sites of the renal pelvis. After completing the posterior wall, the 7 F stent was replaced in the pelvis and the anterior wall of the anastomosis was completed (Fig. 3). At the end, a 15 F Robinson drain was placed though the trocar into the pararenal space. The trocars were removed under laparoscopic visualization and the fasciae of the trocars’ sites were closed with interrupted absorbable sutures. The skin was approximated with clips.
Results
Mean age in patients who underwent LDP was 38 years (20–56). Of these patients, 48 were male and 57 women and the mean body mass index was 26.8 kg/m2.
The mean operative time for LDP was 150 min (range 120–180 min) and the mean estimated blood loss was negligible in all patients. The mean hospital stay was 4 days (4–8).
No conversion to open surgery occurred.
In 57% of the patients, crossing vessels with an anterior course to the ureteropelvic junction were identified. The bladder catheter was removed 3 days after the operation while the ureteral stents were removed after 6 weeks. After removing of the double-J stent, all the patients underwent an intravenous urography and sonography. The mean follow-up was 51 months (range 6–96). Follow-up was calculated from the date of surgery to the date of the most recent documented examination. No patient was lost to follow-up. Clinical successful outcome was defined as complete resolution of preoperative flank pain and radiographic successful outcome was defined as adequate renal excretion (T 1/2, 20 min) and preserved or improved ipsilateral renal function on MAG-3 diuretic renal scan.
Four patients (3.8%) presented a recurrence of UPJO 6, 9, 11 and 16 months after surgery and they underwent successfully open surgery. In two patients (1.9%), there was an injury of the renal artery of lower pole. In the following renal Doppler sonography and renal scintigraphy, a reduction of renal function of 4 and 7% in each patient was noted, but in both patients no stricture formation after the surgery was reported. After 2 years, both patients presented a normal renal function (creatinine: 92 and 86 μmol/l).
Six patients (5.7%) developed a postoperative haematoma; nevertheless, in no case, a surgical revision was necessary.
An urinoma was identified in seven patients (6.6%), and a mono-J stent was postoperatively placed under radiologic guide; in two patients, a laparoscopic re-operation with suturing of the insufficiently closed anastomosis was necessary; in the other patients, the urinoma solved spontaneously and a new double-J stent was replaced and left in situ for 8 weeks.
Intra- and postoperative data are summarized in Table 1.
In the follow-up, we noted a successful rate in 96.2% of the patients, who did not present any flank pain.
Discussion
The ideal treatment for UPJO would be minimally invasive with a low complication and failure rate. Therapy of UPJ stenosis has been significantly influenced by various minimally invasive techniques, including percutaneous and ureteroscopic endopyelotomy, cutting transvesical balloon dilatation as well as laparoscopic pyeloplasty. All of these procedures were introduced with the goal to meet the standard of open dismembered pyeloplasty providing long-term success rates between 93 and 97%, with a lower surgical trauma for the patients [2].
Laparoscopic pyeloplasty is a minimally invasive alternative in the treatment of UPJ obstruction and was developed in the early 1990s and after an initial period of development, actually it can duplicate the high success rates achieved with open pyeloplasty, if performed by expert surgeons in centres with high laparoscopic expertise [3, 4].
Nowadays, the overall complication rates for open and laparoscopic pyeloplasty were similar, with a trend towards fewer chest complications in the laparoscopic group, which did not reach significance [4, 5].
The success rates after LDP are 73–100% in literature [2–20].
Already at the begin of the development of laparoscopic pyeloplasty, Türk et al. [3] reported a success rate in 97.7% of the patients, value that perfectly reflects the results obtained after open surgery, with an incidence of complications of 2%.
In 2006, Eden [16] published a review about the results associated with the minimal invasive treatment of UPJO. In the laparoscopic series, he reported no significant differences between the retroperitoneal and transperitoneal approach, noting that with a transperitoneal technique there is the advantage to have a better visualization of anatomy and greater workspace to suture. Moreover, he pointed that in contrast with the 3–11% transfusion rate following endourologic UPJO incision, transfusion following laparoscopic pyeloplasty is rare.
In our study, 105 patients underwent a LDP for UPJO. The mean operation time of 150 min is in accordance with literature [2–20].
The mean estimated blood loss was negligible in all patients and no conversion to open surgery occurred.
The mean follow-up was 51 months. Postoperative evaluation included retrograde pyelography at the time of stent removal, clinical history, excretory urography (6–8 weeks postoperatively and then every 3 months) and ultrasonography. In 96.2% of patients, a complete successful rate was registered.
Conclusion
Laparoscopic pyeloplasty is a technically demanding procedure, which requires a great laparoscopic experience. Nevertheless, if performed by expert surgeons in high-volume centres, it presents results that are comparable with open surgery, with a lower surgical trauma for the patients.
References
Fornara P, Doehn C, Seyfarth M, Jocham D (2000) Why is urological laparoscopy minimally invasive? Eur Urol 37:241–250
Rassweiler J, Subotic S, Feist-Schwenk M et al (2007) Minimally invasive treatment of ureteropelvic junction obstruction: long-term experience with an algorithm for laser endopyelotomy and laparoscopic retroperitoneal pyeloplasty. J Urol 177:1000–1005
Türk IA, Davis JW, Winkelmann B (2002) Laparoscopic dismembered pyeloplasty: the method of choice in the presence of an enlarged renal pelvis and crossing vessels. Eur Urol 42:268–275
Rassweiler J, Teber D, Frede T (2008) Complications of laparoscopic pyeloplasty. World J Urol 26:539–547
Calvert RC, Morsy MM, Zellhof B, Rhodes M, Burgess NA (2008) Comparison of laparoscopic and open pyeloplasty in 100 patients with pelvi-ureteric junction obstruction. Surg Endosc 22:411–414
Ramakumar S, Lancini V, Chan DY, Parsons JK, Kavoussi LR, Jarrett TW (2002) Laparoscopic pyeloplasty with concomitant pyelolithotomy. J Urol 167:1378–1380
Davenport K, Minervini A, Timoney AG, Keeley FX Jr (2005) Our experience with retroperitoneal and transperitoneal laparoscopic pyeloplasty for pelvi-ureteric-junction obstruction. Eur Urol 48:973–977
Maynes LJ, Levin BM, Webster TM, Baldwin D, Herrell SD (2008) Measuring the true success of laparoscopic pyeloplasty. J Endourol 22:1193–1198
Porpiglia F, Billia M, Volpe A, Morra I, Scarpa RM (2007) Transperitoneal left laparoscopic pyeloplasty with transmesocolic access to the pelvi-ureteric junction: technique description and results with a minimum follow-up of 1 year. BJU Int 101:1024–1028
Klinger HC, Remzi M, Janetschek G, Kratzik C, Marberger MJ (2003) Comparison of open vs. laparoscopic pyeloplasty techniques in treatment of uretero-pelvic junction obstruction. Eur Urol 44:340–345
Troxel S, Das S, Helfer E, Nugyen M (2006) Laparoscopy versus dorsal lumbotomy for ureteropelvic junction obstruction repair. J Urol 176:1073–1076
Yanke BV, Lallas CD, Pagnani C, McGinnis DE, Bagley DH (2008) The minimal invasive treatment of ureteropelvic junction obstruction: a review of our experience during the last decade. J Urol 180:1397–1402
Shoma AM, El Nahas AR, Bazeed MA (2007) Laparoscopic pyeloplasty: a prospective randomized comparison between the transperitoneal approach and retroperitoneoscopy. J Urol 178:2020–2024
Adeyoju AB, Hrouda D, Gill IS (2004) Laparoscopic pyeloplasty: the first decade. BJU Int 94:264–267
Bachmann A, Ruszat R, Forster T et al (2006) Retroperitoneoscopic pyeloplasty for ureteropelvic junction obstruction (UPJO): solving the technical difficulties. Eur Urol 49:264–272
Eden CG (2007) Minimally invasive treatment for ureteropelvic junction obstruction: a critical analysis of results. Eur Urol 52:983–989
Vijayanad D, Hasan T, Rix D, Soomro N (2006) Laparoscopic transperitoneal dismembered pyeloplasty for ureteropelvic junction obstruction. J Endourol 20:1050–1053
Papalia R, Simone G, Leonardo C et al (2009) Retrograde placement of ureteral stent and ureteropelvic anastomosis with two running sutures in transperitoneal laparoscopic pyeloplasty: tips of success in our learning curve. J Endourol 23:847–852
Kaouk JH, Kuang W, Gill IS (2002) Laparoscopic dismembered tabularized flap pyeloplasty: a novel technique. J Urol 167:229–231
Eden CG, Cahill D, Allen JD (2001) Laparoscopic dismembered pyeloplasty: 50 consecutive cases. BJU Int 88:526–531
Conflict of interest statement
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wagner, S., Greco, F., Inferrera, A. et al. Laparoscopic dismembered pyeloplasty: technique and results in 105 patients. World J Urol 28, 615–618 (2010). https://doi.org/10.1007/s00345-009-0483-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-009-0483-0