Abstract
Objectives
To investigate the symptomatic and quality of life (QoL) response to treatment with tolterodine extended release (ER) in subgroups of male patients with Overactive Bladder Syndrome (OAB) and LUTS suggestive of non-obstructive benign prostatic hyperplasia (BPH) according to age, symptom severity, diabetes mellitus status, and concomitant treatment for LUTS.
Methods
Patients treated with tolterodine ER 4 mg/day for OAB symptoms, alone or added to unsuccessful alpha-blocker treatment of ≥6 weeks duration, and presumed non-obstructive BPH (Q max ≥ 15 ml/s) were observed for 12 weeks in a non-interventional study. Patients completed the International Prostate Symptom Score (IPSS) and Overactive Bladder Questionnaire (OAB-q) at baseline and after 12 weeks.
Results
52.4% of 741 patients were aged ≤65 years; 4, 64, and 32% had mild, moderate, and severe symptoms, respectively, according to IPSS; 14% had diabetes mellitus, and in 42% tolterodine was added to alpha blockers. In the various subgroups, mean IPSS total scores improved by 2.8–11.1 points, IPSS QoL scores by 1.8–2.4 points, and all OAB-q subscores by more than 14 points. Only IPSS and OAB-q baseline scores had a relevant impact on changes during treatment, benefits were greatest in patients with more severe symptoms and bother.
Conclusions
In men with symptoms of OAB and LUTS suggestive of non-obstructive BPH of all IPSS severity classes, aged ≤65 years or above, with or without concomitant diabetes or alpha-blockers, symptoms and QoL improved markedly during treatment with tolterodine ER.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive Bladder Syndrome (OAB) defined as urgency, frequency, and nocturia, with or without incontinence, affects 15.6% of men aged 40 years and older in European countries [1]. While muscarinic receptor antagonists like tolterodine are widely used in women with OAB symptoms [2], they are not regularly used in men with OAB symptoms and LUTS suggestive of benign prostatic hyperplasia (BPH). However, recent evidence suggests that they can be used successfully for symptom control in this male population [3–6].
To investigate the symptomatic and quality of life (QoL) outcome of treatment with the antimuscarinic tolterodine extended release (ER) in subgroups of patients according to age, symptom severity, the presence or absence of diabetes mellitus, and concomitant treatment for LUTS, a non-interventional study was carried out. In this study, 1,080 men with OAB symptoms and LUTS suggestive for non-obstructive BPH were observed for 12 weeks on treatment with tolterodine ER, either alone or added to alpha-blocker therapy, shown to be unsuccessful over a period of at least 6 weeks.
Methods
Study design
This was a prospective, non-interventional observational study. Such studies investigate the use of approved drugs administered under routine conditions, i.e., all diagnostic and therapeutic procedures are those applied in clinical routine. Treatment modalities are not defined by a clinical trial protocol but by the physician’s clinical decisions. The observational protocol only defines the characteristics of patients to be observed in the study and the set of data to be collected systematically.
Patient population
Participating office-based urologists were asked to document male patients suffering from LUTS suggestive of BPH, for whom they had decided to treat OAB symptoms of frequency, urgency, or urgency incontinence with tolterodine ER. Diagnosis of LUTS suggestive of BPH had to be based on the current guidelines of the German urological association on Benign Prostatic Syndrome [7]. Patients could be enrolled if either there was no clinical suspect of bladder outlet obstruction (BOO) or storage symptoms had not sufficiently improved after at least 6 weeks’ treatment with an alpha-blocker according to the opinion of the treating physician. The patient’s maximum urinary flow rate (Q max) was required to be at least 15 ml/s. Patients with suspected or confirmed prostate cancer were excluded. Other exclusion criteria were previous treatment with an anticholinergic agent, surgical treatment of BPH or a history of surgical intervention in the bladder or urethra, history of AUR, chronic urinary retention, acute UTI, chronic UTI, prostatitis caused by bacteria or history of recurrent UTIs, history of interstitial cystitis, concomitant medication that may cause urinary retention (e.g., tricyclic antidepressants, neuroleptic agents, antihistamine drugs, and antiParkinson drugs), indwelling catheter or intermittent use of self-catheterization. Demographic data and medical history, Q max and ultrasound assessment of PVR were collected at the baseline visit before treatment with tolterodine ER was started.
Efficacy variables
Patients completed questionnaires on voiding problems (International Prostate Symptom Score, IPSS) and on symptom bother and condition-specific QoL (Overactive Bladder Questionnaire; OAB-q), at baseline and after 12 weeks of treatment.
Statistics
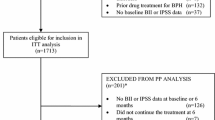
The Full analysis set (FAS) was defined as all patients who have received at least one dose of study treatment during the observation period, have a Q max of at least 15 ml/s and who have not fulfilled any of the exclusion criteria. This population was used for the analyses of efficacy data.
The following subject strata or subgroups analyses were planned age (>65 or ≤65 years), symptom severity [mild (IPSS < 8), moderate (IPSS 8–19), and severe (IPSS 20–35)], diabetes mellitus (yes/no), and concomitant alpha-blocker, phyto drugs or 5-alpha reductase inhibitor treatment for LUTS (yes/no). However, due to the low numbers of patients treated with phyto drugs or 5-alpha reductase inhibitors, only concomitant alpha-blocker treatment was analyzed.
To identify variables associated with change of IPSS total score exploratory multiple linear regression analysis was performed for the baseline/final change including terms of the IPSS total score at baseline, HRQL total score at baseline, age group, residual urine at baseline, diabetes mellitus, concomitant alpha-blocker treatment, Q max, and duration of OAB. Variables associated with change of OAB-q (HRQL total score and bother score) were explored using regression analysis with the independent variables of the respective score at baseline, IPSS total score at baseline, age group, residual urine at baseline, diabetes mellitus, concomitant alpha-blocker treatment, Q max, and duration of OAB. R 2 statistics was used to estimate the impact of these factors. R 2 can be thought of as the proportion of variation in the dependent variable that can be explained or predicted by the independent variable and has a range from 0 (no impact) to 1 (fully explained).
All analyses were descriptive and exploratory. Percentages for categorical variables were to be based on all non-missing values (=100%). Summary measures are reported as mean ± SD or median values. P values of baseline/final changes were calculated with the t test. A sensitivity analysis with the non-parametric Wilcoxon test was performed for the IPSS and QoL.
All statistical analyses were performed by the biometrics group at Pfizer Pharma and SAS (version 8.2) was used to analyze the data for this study.
Results
A total of 1,080 patients were documented between January 2004 and June 2005 and 741 patients fulfilled all criteria for the FAS. At baseline, the mean age in the FAS was 65.2 ± 9.2 years. Patient characteristics and concomitant medical conditions documented in >1% of patients are shown in Table 1. The mean duration of OAB was 1.5 years and the mean duration of LUTS was 3.1 years. Mean Q max was 18.7 ± 3.7 ml/s and mean PVR was 29.3 ± 30.9 ml.
IPSS
Following 12 weeks of tolterodine ER, the total IPSS score improved from 17.2 ± 5.5 to 9.9 ± 4.6, with a change of −7.3 ± 5.2 (P < 0.0001). Table 2 shows the change of IPSS in the different subgroups. Regression analyses of those variables that met the 0.15 significance level for entry into the model indicated that only baseline IPSS (R 2 = 0.39; P < 0.001) had a relevant impact on change, as shown in Table 4. The negative estimate indicates that higher baseline IPSS values were associated with larger improvements in IPSS. Concomitant diabetes mellitus and baseline PVR had no significant effect. IPSS QoL also improved after tolterodine ER treatment, from a baseline value of 3.9 ± 1.0 to a final value of 1.9 ± 1.1 after 12 weeks of treatment; with a change of −2.1 ± 1.4 (P < 0.0001). Table 2 shows the changes from baseline in IPSS QoL score in the different subgroups of patients.
OAB-q
Table 3 shows the change in scores from baseline to final (after 12 weeks of tolterodine therapy) in the OAB-q. All subscales show a relative change from baseline of at least 40% (all P < 0.0001). In every analyzed subgroup, mean improvement in all subscales was >14 points. Results of regression analyses of factors influencing OAB-q scores are shown in Table 4. Only bother score at baseline had a relevant (R 2 > 0.1) influence on the improvement in bother score, and HRQL baseline scores on improvement of HRQL. Greater improvements were seen in patients with severe baseline symptoms than in patients with mild baseline symptoms (Table 3), but even in the subgroup with mild symptoms according to IPSS, mean improvements >14 points were seen in all OAB-q subscores.
Discussion
This non-interventional observational study demonstrated that in patients with OAB and LUTS suggestive of non-obstructive BPH (Q max ≥ 15 ml/s), 12 weeks’ treatment with tolterodine ER alone or added to failed alpha-blocker therapy resulted in clinically meaningful reductions in symptoms as assessed by the IPSS. Overall, the OAB-q and IPSS QoL also indicated a marked improvement in QoL with tolterodine ER.
The aim of treatment of LUTS is primarily to provide a rapid and sustained improvement in symptoms [8]. The results from this study suggest that OAB symptoms in this group of LUTS patients were relieved during 12 weeks of tolterodine ER therapy. These results complement previous experience with tolterodine ER: Tolterodine has also improved frequency, nocturia, and AUA symptom scores in a study with LUTS patients after failed alpha-blocker treatment [9] and a reduction in symptoms and improved QoL under treatment with tolterodine and the alpha-blockers tamsulosin or doxazosin have been seen in patients with BOO and detrusor overactivity [3, 4]. Reduced urinary frequency was also demonstrated in studies of LUTS patients treated with tolterodine [9] or the muscarinic antagonist propiverine alone or in combination with tamsulosin, respectively [10]. The safety of tolterodine in the treatment of patients with BOO and confirmed detrusor overactivity has recently been demonstrated in a placebo-controlled study [11].
Regression analysis of IPSS change indicated a relevant impact only on the baseline IPSS. Likewise, regression analyses of the changes in HRQL and bother score of the OAB-q showed that only their baseline values had a meaningful impact. Although larger improvements were seen in patients with more severe symptoms and bother, even patients with a baseline IPSS <8 demonstrated an improvement in the mean IPSS QoL index from 3.0 to 1.2, in the mean OAB-q bother score from 34.3 to 11.7, and in the OAB-q HRQL score from 76.7 to 93.6. Since an IPSS QoL score of 1 means delight in the urinary condition, while a score of 3 represents mixed feelings, and a change of >10 points in the OAB-q subscales has been demonstrated to be the Minimally Important Difference, i.e., the smallest change that patients perceive as beneficial [12], clinically meaningful improvements in QoL have been seen even in patients with mild symptoms. While current guidelines recommend watchful waiting as a preferred option for patients with mild symptoms [13, 14], our data suggest that such patients can benefit from treatment, too.
Because the current analysis is based on the results of an open-label, observational study without placebo control, interpretation of the data is limited. However, the study type has certain advantages, such as being of sufficient size to allow analysis of multiple subgroups and, as the treatment data were obtained under real-life conditions, the findings are likely to be applicable to general practice [15–17].
Conclusions
In this study of men with OAB and LUTS suggestive of non-obstructive BPH, symptoms and QoL improved markedly during treatment with tolterodine ER. Although larger improvements were seen in patients with more severe symptoms, meaningful QoL improvements were also seen with baseline IPSS values <8.
Age group, concomitant diabetes mellitus, concomitant alpha-blocker treatment, duration of symptoms, and baseline Q max (beyond 15 ml/s) and PVR did not appear to have a relevant effect on the symptomatic response to treatment, which suggests that a wide variety of patients can benefit from tolterodine treatment.
References
Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ (2001) How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int 87:760–766
Abrams P, Cardozo L, Khoury S, Wein A (2005) Incontinence, vol 2. Management Health Publication Ltd, Plymouth
Lee JY, Kim HW, Lee SJ, Koh JS, Suh HJ, Chancellor MB (2004) Comparison of doxazosin with or without tolterodine in men with symptomatic bladder outlet obstruction and an overactive bladder. BJU Int 94:817–820
Athanasopoulos A, Gyftopoulos K, Giannitsas K, Fisfis J, Perimenis P, Barbalias G (2003) Combination treatment with an alpha-blocker plus an anticholinergic for bladder outlet obstruction: a prospective, randomized, controlled study. J Urol 169:2253–2256
Kaplan SA (2004) Use of muscarinic receptor antagonists as monotherapy in men with lower urinary tract symptoms who failed previous therapy with alpha blockers. J Urol 171(Suppl):917 (abstract)
Lim E, Chia SJ (2005) Combination therapy using alpha-blocker and antimuscarinic drugs in men with lower urinary tract symptoms suggestive of bladder outlet obstruction and an overactive bladder: is it safe and efficacious? Neurourol Urodyn 24(5–6):205 (abstract)
Berges R, Dreikorn K, Höfner K, Jonas U, Laval KU, Madersbacher S, Michel MC, Muschter R, Oelke M, Pientka L, Tschuschke C, Tunn U (2003) Leitlinien der Deutschen Urologen zur Diagnostik des benignen Prostatasyndroms (BPS). Urologe A 42:584–590
Roehrborn CG (2006) Drug treatment for LUTS and BPH: new is not always better. Eur Urol 49:5–7
Kaplan SA, Walmsley K, Te AE (2005) Tolterodine extended release attenuates lower urinary tract symptoms in men with benign prostatic hyperplasia. J Urol 174:2273–2275 (discussion 2275–2276)
Saito H, Yamada T, Oshima H et al (1999) A comparative study of the efficacy and safety of tamsulosin hydrochloride alone and combination of propiverine hydrochloride and tamsulosin in the benign prostatic hypertrophy with pollakiuria and/or urinary incontinence. Jpn J Urol Surg 12:525–536
Abrams P, Kaplan S, De Koning Gans HJ, Millard R (2006) Safety and tolerability of tolterodine for the treatment of overactive bladder in men with bladder outlet obstruction. J Urol 175:999–1004 (discussion 1004)
Coyne KS, Matza LS, Thompson CL (2005) The responsiveness of the overactive bladder questionnaire (OAB-q). Qual Life Res 14:849–855
Roehrborn CG, McConnell JD, Barry MJ, Benaim E, Bruskewitz RC, Blute ML, Holtgrewe HL (2006) AUA guideline on the Management of Benign Prostatic Hyperplasia. http://www.auanet.org/guidelines/bph.cfm, Accessed June 19, 2006
Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ (2004) EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol 46:547–554
Michel MC, de la Rosette JJ, Piro M, Goepel M (2004) Does concomitant stress incontinence alter the efficacy of tolterodine in patients with overactive bladder? J Urol 172:601–604
Michel MC, Schneider T, Krege S, Goepel M (2002) Does gender or age affect the efficacy and safety of tolterodine? J Urol 168:1027–1031
Michel MC, de la Rosette JJ, Piro M, Schneider T (2005) Comparison of symptom severity and treatment response in patients with incontinent and continent overactive bladder. Eur Urol 48:110–115
Acknowledgments
We are indebted to the 284 investigators who documented the patients in this trial.
Conflict of interest statement
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Höfner, K., Burkart, M., Jacob, G. et al. Symptomatic and quality of life response to tolterodine in subgroups of men with overactive bladder symptoms and presumed non-obstructive benign prostatic hyperplasia. World J Urol 28, 353–357 (2010). https://doi.org/10.1007/s00345-009-0460-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-009-0460-7