Abstract
Background
Caudal anesthesia (CA) is widely recommended due to excellent analgesia in distal hypospadia repairs, but its potential side effect on urinary retention interferes with patient comfort. To objective is to determine the impact of CA versus penile block (PB) on postoperative micturition.
Methods
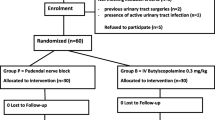
Sixty distal hypospadia repairs performed over a 48-month period were analyzed concerning the impact of applicated analgesia on postoperative micturition. Inclusion criteria were Mathieu or Snodgrass procedures, use of a non-dribbling urethral stent, CA or PB. Endpoint was first postoperative micturation (<6 h), or treatment of delayed postoperative micturation (>6 h).
Results
CA was used in 27 and PB in 33 cases. Compared groups had similar age (mean: 31 months, range 12–68 vs. 28 months, range: 14–145), weight (mean: 13 kg, range 9–18 vs. 15 kg, range 8–59), operation duration (mean 61 min, range 30–105 vs. mean 67 min, range 35–120) and surgical technique (Mathieu/Snodgrass: 7/20 CA vs. 19/14 PB). Micturation was significantly less impaired in the PB than CA group (5/33 vs. 15/27; p < 0.05). Delayed or non-micturation was successfully treated in 4 and 14 patients, respectively, by cholinergic agonists. One patient of each group required a suprapubic drain on the first operative day after unsuccessful medical treatment.
Conclusions
In our series, children undergoing distal hypospadia repair experienced significantly less impaired micturition when using penile block instead of caudal anesthesia. We recommend penile block as the first choice perioperative analgesia, when spontaneous postoperative micturition must be guaranteed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For decades, penile block anesthesia was widely and effectively used for various types of penile reconstructive surgery. Recently, due to improved composition, dosage and concentration of local anesthetics [1, 2], and low incidence of negative side effects such as motor blockade and postoperative nausea and vomiting [3], caudal anesthesia has become one of the most used and accepted regional blocks for children undergoing hypospadia repair [1, 4].
However, postoperative patient comfort is a major issue after distal hypospadia repair and depends on adequate analgesia and unimpaired micturition, especially when no suprapubic catheter is in place.
Micturition impairment and urinary retention is a known side effect of caudal block anesthesia and its incidence in larger series of infraumbilical surgical procedures ranged from 0.7 to 5.3%, while hypospadia repair seems to cause urinary retention more than other procedures [4, 5].
With routine use of caudal block anesthesia for hypospadia repair since 2003, we observed several cases of urinary retention after distal hypospadia repair. Therefore, we reintroduced penile block anesthesia for a consecutive series of children scheduled for distal hypospadia repair from the end of 2005.
The aim of our retrospective study was to compare the incidence of impaired postoperative micturition in a consecutive group of patients with penile block with a former caudal anesthesia group.
Patients and methods
Study population
The study included 60 distal hypospadia repairs from December 2003 to November 2007. Inclusion criteria were patients with distal penile, subcoronal and coronal type of hypospadia scheduled for Mathieu or Snodgrass repairs with an intermittent non-dribbling urethral stent for 7 days. Patients with glandular or proximal type, need of chordee excision, and placement of a suprapubic drain were excluded from the study. In addition, patients with successfully applicated regional anesthesia as described by Silvani et al. [2] were included. Patients not suitable for caudal anesthesia, due to underlying contraindicating disease, were excluded.
Until December 2005, distal hypospadia repair was performed under caudal anesthesia and penile anesthesia in a consecutive series thereafter. Three re-do procedures were performed within the penile block anesthesia period from December 2005, and after former caudal anesthesia in one patient.
Primary endpoint of the study was first postoperative micturition and the incidence of impairment. Secondary endpoints were type and duration of operation, postoperative pain assessment, stent problems, and type of medical or surgical treatment to relieve micturition impairment.
Anesthesia
General anesthesia was induced with sevoflurane in oxygen via facemask and remifentanil (1 μg kg−1) and rocuronium (0.5 mg kg−1) were used thereafter to facilitate tracheal intubation. Maintenance of anesthesia was routinely performed with sevoflurane in an oxygen/air mixture and a continuous intravenous infusion of remifentanil at a dosage of 0.1–0.5 μg kg−1 min−1. Additionally, each patient received an isotonic electrolyte solution (Jonosteril®, Fresenius, Bad Homburg, Germany) at a dosage of 5–10 ml kg−1 h−1, adding 1% glucose for children up to 2 years of age.
Caudal anesthesia was used in 27 patients from December 2003 to November 2007. At the end of the operation, we used the standard technique in lateral decubitus position and all patients received a “high volume, low concentration” caudal anesthesia (1 ml kg−1 ropivacaine 0.2%) [2, 4].
Penile block was used at the end of the surgical procedure in 33 patients (December 2005–November 2007) by applying 0.2 ml kg−1 bupivacaine 0.5% to anesthetize dorsal penile nerves subpubic via one puncture in the midline as described elsewhere [2, 6].
Surgical technique
All procedures were performed by pediatric surgeons experienced in penile reconstructive surgery. Details of the Mathieu and the modified Snodgrass techniques were performed as described elsewhere [7, 8]. To unburden the distal part of the urethra, we placed an 8 or 10 French urethral stent in the perineal part of the urethra at the end of the procedure to allow spontaneous micturition. The stent was removed after 7 days postoperative.
The first micturition was defined as delayed after 6 h postoperatively. Treatment of delayed micturition due to urinary retention included application of cholinergic agonists (carbachol; 0.05–0.1 mg kg−1 day−1 s.c.) or, if necessary, placement of a suprapubic drainage. Pain was assessed by the attending nurse using the Children’s and Infant’s Postoperative Pain Scale (CHIPPS) [9] in children younger than 4 years and the Smiley Scale and Visual Analogue Scale (VAS) in older children [10, 11]. Postoperative analgesia included paracetamol (max 90 mg kg−1 day−1), metamizole (max 40 mg kg −1day−1) and, in children weighing less than 10 kg ibuprofen (max 30 mg kg−1 day−1). Rescue analgesia treatment was provided with intravenous nalbuphine (100 μg kg−1 body-weight−1).
Statistical analysis
Data of patient characteristics are given as median, mean and range. Statistical comparison was performed using the Student t test after testing for normal distribution (SigmaStat-Software, Jandel Scientific). The incidence of impaired postoperative micturition was compared using the Chi-Square-test. Significance was assumed at a p value of less than 0.05.
Results
Patient demographics, including age and weight distribution and operation duration in compared regional anesthesia groups, were not statistically different and are shown in Table 1.
Micturition was considered unimpaired up to 6 h postoperative in 40 out of 60 distal hypospadia repairs (67%). Postoperative impaired micturition was noticed after 20 hypospadia repairs and its incidence was significantly higher after caudal block compared to penile block anesthesia [15/27(45%) vs. 5/33 (15%), P < 0.05] as shown in Table 2.
Twenty-six of 60 distal hypospadia repairs (43%) were Mathieu, whereas 34 (57%) were modified Snodgrass procedures. Distribution of the types of distal hypospadia was similar in compared regional anesthesia groups (caudal vs. penile: distal penile 3/5; subcoronal 15/17; coronal 9/11). Micturition impairment occurred in 7 Matthieu and 13 Snodgrass cases, with no significant difference between the type of surgical repair [7 of 26 (27%) vs. 13 of 34 (38%); n.s.], which excludes an impact of the surgical technique. There were no cases of catheter blockage.
Analysis of type of surgical repair within regional anesthesia groups revealed delayed micturition after 4 Mathieu/11 Snodgrass procedures in caudal versus 3 Mathieu/2 Snodgrass repairs in penile block groups. Urinary retention was the leading symptom in the majority of the 20 patients with delayed micturition (14 caudal, 5 penile block anesthesia). Treatment with cholinergic agonists was successful in 14 (3 Mathieu, 11 Snodgrass), respectively, in 4 (3 Mathieu, 1 Snodgrass) cases, whereas one patient of each regional anesthesia group required intermittent suprapubic drainage on the first postoperative day after Snodgrass repair (Table 2). Pain assessment, as well as applicated analgesics, revealed similarity in compared groups. Painful micturition was observed in one patient after caudal block anesthesia. No patient in our series required rescue analgesia with nalbuphine.
Discussion
Caudal block anesthesia has almost replaced the use of penile block anesthesia for various infraumbilical surgical procedures in children [1–4, 12, 13]. The majority of studies on caudal block anesthesia are focused on lasting analgesia and reduced side effects [1–4], but the problem of impaired postoperative micturition is somewhat underestimated in these reports. Moreover, the reported spectrum of the type of infraumbilical surgery and penile surgery was inhomogeneous in these series.
Our results indicate, for the first time, that the rate of impaired postoperative micturition was significantly higher in children undergoing caudal compared to penile block anesthesia. The association of micturition and regional anesthesia was given because of the homogeneity of compared regional anesthesia groups, as our results were affected neither by the type of the two surgical techniques nor by the distribution of distal hypospadia types.
Besides type of regional anesthesia, there are several other factors influencing postoperative voiding behavior. Postoperative voiding patterns in infants and children depend on the type of regional anesthesia, intraoperative application of additional analgesics, the grade of bladder distension, hydration, bladder capacity, psychomotor state of arousal, psychosocial status of the child and individual voiding habits, and a wide range of 2–20 daily voids in different age groups [14]. Koomen et al. [15] suggested ultrasound scan to detect postoperative urinary distension after caudal anesthesia. We have no data on postoperative bladder filling as we did not perform ultrasound studies, but we observed similar conditions in our groups such as operation duration, surgical technique and application of a standardized intraoperative fluid substitution regime. We defined impaired micturition as more than 6 h postoperative. This is in contrast to Koomen et al. who rated a normal postoperative voiding within 12 h [15], but this time interval might be too long and not acceptable, especially in younger infants.
In our series, regional block anesthesia was generally performed at the end of the operation. This is in contrast to reports by Chhibber et al. [16], who suggested penile block before and after penile surgery, as well as Silvani et al. [2], who recommended caudal block anesthesia at the beginning and the end of the operation. As we did not observe any need for rescue analgesics, we consider our regional block anesthesia regimen as sufficient.
In our series, micturition impairment was not related to the type of reconstructive procedure, i.e. Mathieu or Snodgrass and re-do procedures (3 patients). Placement of transurethral stents in distal hypospadia repair is a matter of debate [7, 17]. Like others [18], we unburden the distal urethra with intermittent urethral stents for one week.
A Cochrane Database Systemic Review from 2008 [19] comparing caudal epidural block versus other methods of postoperative pain relief for circumcision in boys revealed that there were no differences in the need for rescue analgesics between caudal, parenteral and penile block methods. The authors postulated that the evidence from trials is still limited by small numbers and poor methodology [19]. Similarly, there is still lack of comparable data for distal hypospadia repair in children. Therefore, a randomized prospective trial is needed.
Conclusions
In our series, children undergoing distal hypospadia repair experienced significantly less impaired micturition when penile block was used instead of caudal anesthesia. Thus, with regard to postoperative patient comfort, we recommend penile block as the first choice of perioperative analgesia, when spontaneous postoperative micturition is warranted.
References
Samuel M, Hampson-Evans D, Cunnington P (2002) Prospective to a randomized double-blind controlled trial to assess efficacy of double caudal analgesia in hypospadias repair. J Pediatr Surg 37:168–174. doi:10.1053/jpsu.2002.30247
Silvani P, Camporesi A, Agostino MR, Salvo I (2006) Caudal anesthesia in pediatrics: an update. Minerva Anestesiol 72:453–459
Sakellaris G, Georgogianaki P, Astyrakaki E, Michalakis M, Dede O, Alegakis A, Makatounaki K, Charissis G (2008) Prevention of post-operative nausea and vomiting in children-a prospective randomized double-blind study. Acta Paediatr 97:801–804. doi:10.1111/j.1651-2227.2008.00804.x
Aprodu GS, Munteanu V, Filciu G, Goţia DG (2008) Caudal anesthesia in pediatric surgery. Rev Med Chir Soc Med Nat Iasi 112:142–147
Pappas AL, Sukhani R, Hatch D (1997) Caudal anesthesia and urinary retention in ambulatory surgery. Anesth Analg 85:706. doi:10.1097/00000539-199709000-00044
Telgarsky B, Karovic D, Wassermann O, Ogibovicova E, Csomor D, Koppl J, Slobodnikova K, Podhoransky B, Brenner M, Liscak R, Gasparec P, Polak V, Trnka J, Sagat T, Trimmel H (2006) Penile block in children, our first experience. Bratisl Lek Listy (Tlacene Vyd) 107:320–322
Hakim S, Merguerian PA, Rabinowitz R, Shortliffe LD, McKenna PH (1996) Outcome analysis of the modified Mathieu hypospadias repair: comparison of stented and unstented repairs. J Urol 156:836–838. doi:10.1016/S0022-5347(01)65834-8
Stehr M, Lehner M, Schuster T, Heinrich M, Dietz HG (2005) Tubularized incised plate (TIP) urethroplasty (Snodgrass) in primary hypospadias repair. Eur J Pediatr Surg 15:420–424. doi:10.1055/s-2005-872924
Buttner W, Finke W, Hilleke M, Reckert S, Vsianska L, Brambrink A (1989) Development of an observational scale for assessment of postoperative pain in infants. Anasthesiol Intensivmed Notfallmed Schmerzther 33:353–361. doi:10.1055/s-2007-994263
Keck JF, Gerkensmeyer JE, Joyce BA, Schade JG (1996) Reliability and validity of the faces and word descriptor scales to measure procedural pain. J Pediatr Nurs 11:368–374. doi:10.1016/S0882-5963(96)80081-9
Reismann M, von Kampen M, Laupichler B, Suempelmann R, Schmidt AI, Ure BM (2007) Fast-track surgery in infants and children. J Pediatr Surg 42:234–238. doi:10.1016/j.jpedsurg.2006.09.022
Panjabi N, Prakash S, Gupta P, Gogia AR (2004) Efficacy of three doses of ketamine with bupivacaine for caudal analgesia in pediatric inguinal herniotomy. Reg Anesth Pain Med 29:28–31
Khalid A, Siddiqui SZ, Haider S, Aftab S (2007) Single dose caudal tramadol with bupivacaine and bupivacaine alone in pediatric inguinoscrotal surgeries. J Coll Physicians Surg Pak 17:519–522
Fisher QA, McComiskey CM, Hill JL, Spurrier EA, Voigt RE, Savarese AM, Beaver BL, Boltz MG (1993) Postoperative voiding interval and duration of analgesia following peripheral or caudal nerve blocks in children. Anesth Analg 76:173–177
Koomen E, Janssen S, Anderson BJ (2002) Use of ultrasound bladder monitoring in children after caudal anaesthesia. Paediatr Anaesth 12:738–741. doi:10.1046/j.1460-9592.2002.00946.x
Chhibber AK, Perkins FM, Rabinowitz R, Vogt AW, Hulbert WC (1997) Penile block timing for postoperative analgesia of hypospadias repair in children. J Urol 158:1156–1159. doi:10.1016/S0022-5347(01)64410-0
El-Sherbiny MT (2003) Tubularized incised plate repair of distal hypospadias in toilet-trained children: should a stent be left? BJU Int 92:1003–1005. doi:10.1111/j.1464-410X.2003.04513.x
Chen SC, Yang SS, Hsieh CH, Chen YT (2000) Tubularized incised plate urethroplasty for proximal hypospadias. BJU Int 86:1050–1053. doi:10.1046/j.1464-410x.2000.00966.x
Cyna AM, Middleton P (2008) Caudal epidural block versus other methods of postoperative pain relief for circumcision in boys. Cochrane Database Syst Rev 8:CD003005
Conflict of interest statement
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Metzelder, M.L., Kuebler, J.F., Glueer, S. et al. Penile block is associated with less urinary retention than caudal anesthesia in distal hypospadia repair in children. World J Urol 28, 87–91 (2010). https://doi.org/10.1007/s00345-009-0420-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-009-0420-2