Abstract
Objective
To assess the oncological safety of laparoscopic procedures for the management of urothelial carcinomas of the urinary tract.
Methods
Data on laparoscopic management of urothelial carcinomas in the literature were analysed using MEDLINE and by matching the following keywords: urological malignancies, upper tract tumours, bladder carcinomas, laparoscopic approach, recurrence, follow-up and metastasis site.
Results
Minimally invasive techniques are being used increasingly in the management of these tumours and successfully achieving the benefits of lower blood loss and more rapid patient recovery. To date, no evidence level 1 information is available and published series of these technically challenging cases are small and follow-up limited. Short to medium term follow-up appears encouraging in terms of recurrence and survival rates, but long-term data are immature compared to the established open techniques these procedures seek to duplicate. Specific concerns in terms of the oncologic safety of laparoscopy, especially with regard to the pneumoperitoneum, tumour manipulation and specimen extraction are addressed. Port-site metastases and tumour seeding are rare events and appear to be mainly related to the grade and stage of the tumour. Specific precautions are required to minimise these risks.
Conclusion
Oncological results of the laparoscopic approach are difficult to compare with those of open surgery. However, recent series have not reported unusual tumour dissemination or a higher rate of recurrence with this approach. Laparoscopic techniques are not yet standard of care in invasive urothelial carcinomas. Long-term assessment is ongoing and awaited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urothelial carcinomas are the fourth most common tumours after prostate (or breast) cancer, lung cancer and colorectal cancer. Bladder tumours account for 90–95% of urothelial carcinomas [1, 2]. It is the most common malignancy of the urinary tract and the second most common malignancy of the urogenital tract after prostate cancer. It accounts for 5–10% of all the cancers diagnosed every year in Europe [1, 2]. Bladder cancer is ranked the 11th most common cancer in the world and over 50% of cases occur in developed countries [1, 2]. Upper urinary tract urothelial cell carcinomas (UUT-UCCs) are scarce and account for only 5–10% of urothelial carcinomas [3, 4]. The estimated annual incidence in western countries is about 1–2 new cases/100,000 inhabitants. In 8–13% of cases, a synchronous bladder cancer is present. Recurrence in the bladder or the contralateral urinary tract occurs in 30–51% of UUT-UCCs [5, 6]. Open radical cystectomy and open nephroureterectomy (ONU) remain the gold standard procedures for the management of invasive bladder cancer or UUT-UCCs, respectively.
Radical prostatectomy and nephrectomy are currently being performed laparoscopically, with oncological results similar to those of open surgery [7, 8]. Laparoscopy reduces the length of the incision, surgical morbidity, postoperative pain, length of hospital stay and convalescence, and even cost. Urothelial carcinomas are tumours that disseminate readily and it has been feared that tumour dissection during laparoscopic procedures might be associated with a higher risk of recurrence, although this remains a matter of controversy [9–14]. It had been postulated initially that the high-pressure environment of the pneumoperitoneum might exacerbate tumour dissemination and result in a higher rate of recurrence, leading several groups to suggest that laparoscopic procedures should be avoided, in urothelial cancers, whenever the tumour invades the muscle wall [9, 10, 13, 15, 16]. Still, open surgery remains the standard of care for the management of urothelial cell carcinomas (UCCs) of the bladder and the upper urinary tract. Advances in laparoscopic techniques have increasingly challenged this concept. However, concern continues to exist regarding the oncological safety of laparoscopic procedures in the management of these tumours. Nevertheless, several centres of expertise have recently published good oncologic outcomes after laparoscopic surgery in UUT-UCCs and in bladder carcinomas [17–22]. Whether laparoscopic surgery will play a key role in the future remains to be seen. This review aims to define the present role of laparoscopic surgery in the management of invasive urothelial cell carcinoma based on the recent literature. The use and role of laparoscopy in the management of upper tract urothelial tumours are dealt with initially, followed by the current status of laparoscopic radical cystectomy.
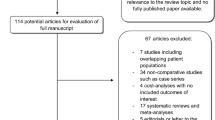
Methods
The literature was reviewed using the National Library of Medicine database (http://www.pubmed.gov). A MEDLINE search was performed with special emphasis on urothelial malignancies and laparoscopic surgical procedures using combinations of the following terms: urinary tract cancer, bladder carcinomas, urothelial carcinomas, upper urinary tract, renal pelvis, ureter prognosis, carcinoma, transitional cell, renal pelvis, ureter, bladder cancer, cystectomy, nephroureterectomy, minimally invasive surgery, recurrence, survival, port metastatis and laparoscopy. Basically articles were considered between 1990 and 2008. No evidence of level 1 information from prospective randomized trials was available. Due to paucity of randomized data, articles were selected for this review with regards to the following criteria: evolution of concepts, development and refinement of techniques, intermediate and long-term clinical outcomes, quality of the study and relevance. Older studies were included selectively if historically relevant or in case of scanty data in more recent publications.
Results
Upper urinary tract urothelial cell carcinomas (UUT-UCCs)
This section was based on 239 articles regarding laparoscopic nephroureterectomy.
Nephroureterectomy
The first laparoscopic nephroureterectomy (LNU) was performed in 1991 [23]. To date, several types of approach (transperitoneal, retroperitoneal, hand assisted) have been used with mid-term oncological outcomes similar to those for open nephroureterectomy (ONU) [20, 22, 24, 25]. However, the number of published studies is still limited and, with a few exceptions, the length of follow-up often does not exceed 4 years [26–28]. In most series, laparoscopy was performed using the transperitoneal approach. Patients were placed in the lumbotomy position. Port arrangement and initial dissection were as for routine laparoscopic nephrectomy, with early identification of the ureter. The urinary tract was dissected as distally as possible. A small iliac incision was made to retrieve the specimen en bloc and to perform the resection of bladder cuff.
Compared to open surgery, an increased risk of tumour cell spillage due to elevated pressure and lack of tactile control has been presumed [13, 29, 30]. In early experience, there have been reports of retroperitoneal metastatic dissemination and/or of dissemination along the trocar pathway when large tumours have been manipulated in a gas environment [13, 15, 29]. Cases of peritoneal cancer dissemination or early metastases at unusual metastatic sites have been reported, but always for high-grade invasive tumours. However, recent data have tended to demonstrate the lack of evidence regarding the laparoscopic approach [11, 12, 16]. Whether or not the high-pressure environment during laparoscopy is solely responsible for the development of unusual metastasis and/or early recurrence of the disease remains a moot point. In addition, recent data have strongly suggested that there was an important role between tumour type and host biologic mechanisms in the development of port-site metastasis [11].
However, it is now obvious that several precautionary measures have to be taken when operating in a pneumoperitoneal environment that may favour tumour spillage [19, 20, 30, 31]. Direct contact of the instruments with the tumour during dissection is avoided. The potential for tumour spill and seeding exists each time the urinary tract is entered during surgical resection of an urothelial tumour [32]. Therefore, LNU must take place in a closed system. The kidney and ureter must be removed en bloc and the bladder must remain intact when the bladder cuff is removed by laparoscopy. A retroperineoscopic approach has also been described but the safety rules remain identical [33, 34]. This approach may decrease the risk of colonic injury. Ever since these strict rules were established, LNU results have become equivalent to, or even better than, those for ONU [20, 25, 33, 35]. Good 5-year recurrence-free and specific survival rates have been published after for LNU with no significant difference between laparoscopic and ONU in recent series (Table 1). It is worth noting that indications tend to increase as operator skills increase, since most cases of LNU were performed from 2000. However, even if indications for laparoscopic and ONU are in principle the same, most teams still recommend that invasive, large (T3/T4 and or N+/M+) or multifocal tumours should be contraindications to laparoscopic NU, despite the eagerness of patients for minimally invasive surgery. According to the current European guidelines, ONU is still the gold standard treatment for UUT-UCCs [36]. Currently, LNU should be indicated for localised tumours, its indications being restricted to <pT2 tumours, especially if they are located in the ureter [6, 19, 24]. Laparoscopy continues to be evaluated; the absence of a risk of cancer spread is not yet definitively proven. Further prospective results are needed before LNU can become an alternative to ONU as the gold standard treatment for invasive UUT-UCC. Whilst it is reassuring that mid-term cancer control appears not to be affected by the use of laparoscopy, it must be noted that the highest level of evidence for LNU is, thus far, 2a.
Conservative surgery
Endoscopic ablation of low-risk tumours allows for the preservation of a portion of the upper urinary tract and renal unit whilst sparing the patient, the morbidity associated, with open surgery [37, 38]. However, one of the drawbacks of endoscopic approaches is the paucity of specimen available for pathologic evaluation when devices such as laser are used to treat the tumour. Segmental ureteral resection with wide margins, however, provides adequate pathologic specimen for definitive staging and grade analysis whilst also preserving the ipsilateral kidney. In fact, open segmental ureteral resection results in equivalent oncologic outcomes to more extensive resection (i.e. radical NU) in patients with low-grade tumours, but is associated with the same morbidities noted in open surgery [37, 38]. One early case report has shown that an entire laparoscopic ureterectomy is feasible [39], and recent short series have described partial laparoscopic ureteral resection and anastomosis for the conservative management of low-grade UUT-UCC in the distal ureter [38, 40, 41]. The reported intermediate term recurrence and cancer-specific survival results were equivalent to those reported following either ONU or endoscopic ablation in a highly select cohort of patients with low-grade upper tract tumours.
Before considering conservative management, appropriate staging examinations should be performed in a patient with an UUT filling defect in order to decide upon the most fitting surgical procedure. Staging errors are common as contrast imaging cannot evaluate wall infiltration by an UUT-UCC [42]. The work up should therefore always include diagnosis by ureteroscopic biopsy [43]. At presentation, 30–55% of UUT-UCCs are invasive [3]. On the other hand, patients with tumours understaged by imagery and that are likely to recur after conservative treatment (i.e. high-grade invasive tumours) could undergo early radical treatment.
UCC recurrence within the bladder occurs in 20–40% of patients following ONU, reinforcing the importance of close surveillance in the management of urothelial tumours. Following segmental resection and upper tract conservation for UUT, this is particularly crucial. The literature advocates repeat conservative surgery whenever possible for local recurrence [37, 44]. Once again, in order to prevent possible tumour spill and dissemination, strict adherence to techniques aimed at isolating the tumour and preventing the flow of urine from the affected ureter into the peritoneal cavity is strongly advocated [38, 40, 41]. During the ureteral dissection, direct contact with the tumour should be rigorously avoided. Second, ligation of the ureter proximal and distal to the tumour prior to transection of the ureteral wall is essential. Third, intraoperative frozen sections are imperative for oncological safety in order to check surgical margins before opening the bladder to perform any reimplantation. A double-J stent is then placed in most cases intraoperatively through a 5 mm port prior to completion of ureteral reimplant. A direct reimplantation of the ureter is then performed laparoscopically. Laparoscopic segmental resection and direct ureteral reimplantation do not preclude future surveillance ureteroscopy. The refluxing reimplantation technique allows for ureteroscopic access to the upper tract with minimal risk of obstruction or stenosis at the uretero-vesical anastomosis. However, an anti-refluxive ureteral reimplantation may also be considered for a stronger oncological safety. Even though, ureteroscopic surveillance could, thereafter, be more difficult, reflux of tumour cells in the bladder would be theoretically diminished [38, 40, 41]. This technique should still be considered as experimental regarding low data available.
Bladder tumours
This section was based on 106 articles regarding laparoscopic radical cystectomy.
The gold standard of treatment for organ-confined muscle invasive or high-risk superficial bladder cancer remains open radical cystoprostatectomy with several large series demonstrating excellent long-term cancer control [21, 45]. Efforts to reduce the often considerable morbidity of this treatment have led several specialist centres to explore the role of laparoscopic surgery for radical cystectomy. The first case report of a laparoscopic radical cystectomy (LRC) was published in 1993 [46]. Since then, several centres have established that the procedure is technically feasible and reproducible, and small series of either pure or robotically assisted laparoscopic cystectomies have been reported with a variety of urinary diversions constructed either entirely intracorporeally or through a small incision. Whilst more than 700 LRCs have been performed at approximately 20 institutions between 1999 and 2008, the numbers in individual series are small and long-term oncological data are scarce [18].
Peri-operative details
The potential benefits of lower blood loss and more rapid patient recovery that have been observed in minimally invasive prostate and kidney surgery have encouraged the development of similar techniques in cystectomy. To date, the largest published experience of LRC is that of Huang et al. from China with 85 cases [47]. Overall the numbers in series range from 10 to 85 patients [17, 48–51]. Mean operating time is between 244 and 485 min, and mean blood loss ranges from less than 150 to 550 ml. Three of the studies report on robotically assisted procedures (RRCs) with a combined number of 70 patients [52–54].
Complication rates vary between the series. DeGer et al. had 2 patients of 20 who required re-operation for urine leak and recto-vaginal fistula [49], whilst Cathelineau et al. report an 18% complication rate including 1 pulmonary embolus, 3 conservatively managed pelvic haematoma, and 2 urinary fistula, one of which was managed conservatively [17]. Complications post LRC have been analysed in detail by Haber et al. in their series of 54 patients, who concluded that complications were largely due to the urinary diversion. Patients who underwent an open-assisted laparoscopic procedure (i.e. extracorporeal formation of the urinary diversion) had superior results in terms of operative times, blood loss, transfusion rates, time to ambulation, time to oral intake and postoperative complications, compared with those who had a purely laparoscopic procedure (i.e. intracorporeal formation of the diversion). They conclude that a steep learning curve exists for both procedures but that the open-assisted procedure is technically more efficient and has a quicker recovery profile with decreased complication rates [18, 55]. LRC seems to be associated with decreased blood loss and transfusion rates, and quicker recovery when compared to open surgery, but operative times appear to be longer. Porpiglia et al. through a prospective comparative study compared 20 LRCs with 20 ORCs [56]. No significant difference was observed between the two groups with respect to intraoperative and postoperative parameters. The LRC group had less analgesic consumption and a more rapid postoperative return to oral intake. Hospital stays may or may not be shorter, but these results can be affected by the socioeconomic demographics of the patient cohort described [57].
Oncological outcomes
Amongst the longest follow-up yet published, in terms of oncological outcomes is from Haber and Gill with 37 consecutive patients and a mean follow-up of 31 months [18]. Only eight patients (22%) had completed ≥5 years of follow-up, reflecting the paucity of long-term data generally available. The 5-year actuarial overall, cancer-specific and recurrence-free survival were 63, 92 and 92%, respectively. However, if seven patients with unknown current status were presumed to have died, the recalculated 5-year overall and cancer-specific survivals were 58 and 68%, respectively. Oncological outcomes are summarised in Table 2.
Surgical margin positivity was seen in two patients in Haber and Gill’s study (5%) in patients who had pT3a and pT4a pathology [18]. Hemal et al. reported a positive urethral margin in 1 patient of 48, who went on to have a urethrectomy 2 weeks later [50]. In a series comparing RRC with open radical cystectomy, Wang et al. reported 2 positive margins out of 33 in the RRC group, versus 3 out of 21 in the open group, but all these patients had high stage disease and the difference was not significant [54]. In a multicentre collaboration, surgical margin was reported in 13 patients (8%) out of 162 who underwent RRCs [58]. Only 3 studies to date have reported on local recurrence, with 5 out of 84 cases, 3 out of 85 cases and 1 out of 48 cases [17, 50]. Huang et al. have reported one case of trocar site seeding amongst 85 cases [47]. Obviously, as longer follow-up becomes available, more local recurrence may occur in other series.
Recent studies have emphasised the importance of extended lymph node dissection in open radical cystectomy series and the importance of actual lymph node numbers retrieved in terms of survival. Haber and Gill have shown the feasibility of laparoscopic extended lymph node dissection in their most recent 26 patients with a median of 21 (range 11–24) nodes excised in those that had extended dissections [18]. Pruthi and Wallen demonstrated that extended node dissection (mean yield of 19 nodes) was possible in RRC, and Wang et al. found no differences were found in the number of nodes retrieved between the RRC group and those having open cystectomy [53, 54]. However, as soon as an extended lymph node dissection is performed, it increases significantly the length of the procedure. On the other hand, the lack of a proper lymph node dissection limits staging and possibility of adjuvant treatment.
Long-term survival data for large series of open radical cystectomy are well documented. Stein et al. reported recurrence-free and overall 5-year survival at 68 and 66%, respectively. Five-year recurrence-free survival for pT1, pT2, pT3a, pT3b and pT4 disease was 80, 81, 68, 47 and 44%, respectively [21]. However, this study did not provide long-term follow-up on all muscle invasive patients included initially. Therefore, it presents numerous drawbacks that could be criticised afterwards when compared ultimately to minimally invasive surgery.
The outcome data summarised in Table 2 reflect the very short duration of follow-up in all of the published series, as well as the relatively small number of patients in each. In addition, it is essential to underline the strong heterogeneity of patients within and between actual series [45, 46, 58–60]. Consequently, it is currently impossible to compare oncologic data between open and laparoscopic data based on recent series.
The same oncological precautions described previously for laparoscopic management of UUT-UCCs must be observed in undertaking LRC [32]. The technique of LRC is now approaching standardisation and duplicates the established open operation. The same concerns exist with regard to peritoneal spillage of urine and most describe the importance of closure of the urethra with clips or ligature prior to transaction [59, 60]. Similarly, both ureters are closed with clips prior to transaction. Once the dissection is completed and the urethra transacted the intact specimen is immediately placed in an entrapment bag of sufficient size. The specimen is typically retrieved via a minilaparotomy midline incision, which is then used for the extracorporeal construction of the urinary diversion. It may also be extracted through the vagina, or by the way of a slight extension of the umbilical port site in the case of an intracorporeal construction of the diversion. One clinical case has described subcutaneous metastases after laparoscopic lymphadenectomy for a bladder carcinoma with lymphatic invasion [61]. Indeed, there has been only one report of a port-site metastasis occurring directly after RRC [10]. In an extensive review of port-site metastasis and tumour seeding in oncologic laparoscopic urology, Castillo and Vitagliano find that of the 31 reported cases, 14 correspond to UCC, but only one of these was after cystectomy [62]. They conclude that port-site metastasis is a rare occurrence and that aggressive tumour biology seemed to be the main contributory factor. Most cases were high-grade UCC. Other factors such as absence of bag retrieval and morcellation may have also contributed [62].
LRC is being increasingly performed in many centres worldwide [17, 18, 48, 49, 63, 64]. Worldwide experience continues to increase as over 700 surgeries have already been performed as mentioned in the international laparoscopic cystectomy registry so far [65]. That the procedure is technically feasible and reproducible has been shown beyond doubt, though reported operative times from centres already skilled in minimally invasive surgery give clues to the complexity and difficulty of the operation. Complications, when they occur, seem largely to arise from the urinary diversion, and an extracorporeal approach to its construction seems to confer improved outcomes.
Data on long-term overall, disease-specific and recurrence-free survival are still immature compared with the standard of care which must remain open radical cystectomy so far. To prove the non-inferiority of laparoscopy compared with open surgery regarding outcome, multicentre prospective trials are strongly needed. The highest level of evidence for laparoscopic radical cystectomy is 2a.
Conclusions
There is currently not enough evidence in the available literature to suggest that laparoscopic procedures could be a convincing alternative to open techniques in urothelial carcinomas. Therefore, although absolute indications for each surgical approach are not clearly defined, tumour risk factors such as stage, grade, location and size, as well as the patient’s existing co-morbidities, should all be factored into the determination of the optimal intervention. Accurate preoperative staging is essential in order to determine the most appropriate surgical procedure. The basic requirement for laparoscopic surgery in urothelial carcinomas is to maintain the oncologic principles and duplicate established open surgical techniques. No prospective data comparing open and laparoscopic techniques are available so far. It is still too early to state that laparoscopy is or will be the new gold standard for treatment of bladder carcinomas or of UUT-UCCs. However, there is at least no evidence from the recent published data that LNU or laparoscopic cystectomy are inferior to open surgery with regard to oncologic outcomes provided that the appropriate precautionary measures are taken both when manipulating such tumours in the environment of the pneumoperitoneum, and extracting the final specimens. To definitively prove the non-inferiority of laparoscopy compared with open surgery regarding outcome, multicentre prospective randomised trials that would provide evidence level 1 informations are strongly needed.
References
Chopin DK, Gattegno B (2002) Superficial bladder tumors. Eur Urol 42:533–541. doi:10.1016/S0302-2838(02)00466-9
Kirkali Z, Chan T, Manoharan M, Algaba F, Busch C, Cheng L et al (2005) Bladder cancer: epidemiology, staging and grading, and diagnosis. Urology 66:4–34. doi:10.1016/j.urology.2005.07.062
Hall MC, Womack S, Sagalowsky AI, Carmody T, Erickstad MD, Roehrborn CG (1998) Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology 52:594–601. doi:10.1016/S0090-4295(98)00295-7
Tawfiek ER, Bagley DH (1997) Upper-tract transitional cell carcinoma. Urology 50:321–329. doi:10.1016/S0090-4295(97)00230-6
Olgac S, Mazumdar M, Dalbagni G, Reuter VE (2004) Urothelial carcinoma of the renal pelvis: a clinicopathologic study of 130 cases. Am J Surg Pathol 28:1545–1552. doi:10.1097/00000478-200412000-00001
van der Poel HG, Antonini N, van Tinteren H, Horenblas S (2005) Upper urinary tract cancer: location is correlated with prognosis. Eur Urol 48:438–444
Rassweiler J, Tsivian A, Kumar AV, Lymberakis C, Schulze M, Seeman O et al (2003) Oncological safety of laparoscopic surgery for urological malignancy: experience with more than 1,000 operations. J Urol 169:2072–2075. doi:10.1097/01.ju.0000067469.01244.5c
Touijer K, Guillonneau B (2006) Laparoscopic radical prostatectomy: a critical analysis of surgical quality. Eur Urol 49:625–632. doi:10.1016/j.eururo.2006.01.018
Cicco A, Salomon L, Hoznek H, Alame W, Saint F, Bralet MP et al (2000) Carcinological risks and retroperitoneal laparoscopy. Eur Urol 38:606–612. doi:10.1159/000020339
El-Tabey NA, Shoma AM (2005) Port site metastases after robot-assisted laparoscopic radical cystectomy. Urology 66:1110
Highshaw RA, Vakar-Lopez F, Jonasch E, Yasko AW, Matin SF (2005) Port-site metastasis: the influence of biology. Eur Urol 47:357–360. doi:10.1016/j.eururo.2004.11.008
Micali S, Celia A, Bove P, De Stefani S, Sighinolfi MC, Kavoussi LR et al (2004) Tumor seeding in urological laparoscopy: an international survey. J Urol 171:2151–2154. doi:10.1097/01.ju.0000124929.05706.6b
Ong AM, Bhayani SB, Pavlovich CP (2003) Trocar site recurrence after laparoscopic nephroureterectomy. J Urol 170:1301. doi:10.1097/01.ju.0000084660.73614.da
Paolucci V, Schaeff B, Schneider M, Gutt C (1999) Tumor seeding following laparoscopy: international survey. World J Surg 23:989–997. doi:10.1007/s002689900613
Mondet F, Boyer C, Esterni JP (2004) Early metastatic dissemination after nephro-ureterectomy for upper urinary tract tumour: a possible role of laparoscopy? Prog Urol 14:1203–1205
Naderi N, Nieuwenhuijzen JA, Bex A, Kooistra A, Horenblas S (2004) Port site metastasis after laparoscopic nephro-ureterectomy for transitional cell carcinoma. Eur Urol 46:440–441. doi:10.1016/j.eururo.2003.12.018
Cathelineau X, Arroyo C, Rozet F, Barret E, Vallancien G (2005) Laparoscopic assisted radical cystectomy: the montsouris experience after 84 cases. Eur Urol 47:780–784. doi:10.1016/j.eururo.2005.04.001
Haber GP, Gill IS (2007) Laparoscopic radical cystectomy for cancer: oncological outcomes at up to 5 years. BJU Int 100:137–142. doi:10.1111/j.1464-410X.2007.06865.x
Rassweiler JJ, Schulze M, Marrero R, Frede T, Palou Redorta J, Bassi P (2004) Laparoscopic nephroureterectomy for upper urinary tract transitional cell carcinoma: is it better than open surgery? Eur Urol 46:690–697. doi:10.1016/j.eururo.2004.08.006
Roupret M, Hupertan V, Sanderson KM, Harmon JD, Cathelineau X, Barret E et al (2007) Oncologic control after open or laparoscopic nephroureterectomy for upper urinary tract transitional cell carcinoma: a single center experience. Urology 69:656–661. doi:10.1016/j.urology.2007.01.007
Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S et al (2001) Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol 19:666–675
Tsujihata M, Nonomura N, Tsujimura A, Yoshimura K, Miyagawa Y, Okuyama A (2006) Laparoscopic nephroureterectomy for upper tract transitional cell carcinoma: comparison of laparoscopic and open surgery. Eur Urol 49:332–336. doi:10.1016/j.eururo.2005.11.013
Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, Albala DM (1991) Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg 1:343–349
Bariol SV, Stewart GD, McNeill SA, Tolley DA (2004) Oncological control following laparoscopic nephroureterectomy: 7-year outcome. J Urol 172:1805–1808. doi:10.1097/01.ju.0000140995.44338.58
Muntener M, Nielsen ME, Romero FR, Schaeffer EM, Allaf ME, Brito FA et al (2007) Long-term oncologic outcome after laparoscopic radical nephroureterectomy for upper tract transitional cell carcinoma. Eur Urol 51:1639–1644. doi:10.1016/j.eururo.2007.01.038
Argyropoulos AN, Tolley DA (2007) Upper urinary tract transitional cell carcinoma: current treatment overview of minimally invasive approaches. BJU Int 99:982–987. doi:10.1111/j.1464-410X.2007.06870.x
Chung SD, Chueh SC, Lai MK, Huang CY, Pu YS, Yu HJ et al (2007) Long-term outcome of hand-assisted laparoscopic radical nephroureterectomy for upper-tract urothelial carcinoma: comparison with open surgery. J Endourol 21:595–599. doi:10.1089/end.2006.9948
Kawauchi A, Fujito A, Ukimura O, Yoneda K, Mizutani Y, Miki T (2003) Hand assisted retroperitoneoscopic nephroureterectomy: comparison with the open procedure. J Urol 169:890–894. doi:10.1097/01.ju.0000046453.38141.dd
Chueh SC, Tsai ID, Lai MK (2004) Solitary port-site metastasis after laparoscopic bilateral nephroureterctomy for transitional cell carcinoma in a renal transplant recipient. Transpl Proc 36:2697–2698. doi:10.1016/j.transproceed.2004.09.074
Klingler HC, Lodde M, Pycha A, Remzi M, Janetschek G, Marberger M (2003) Modified laparoscopic nephroureterectomy for treatment of upper urinary tract transitional cell cancer is not associated with an increased risk of tumour recurrence. Eur Urol 44:442–447. doi:10.1016/S0302-2838(03)00314-2
Jarrett TW, Chan DY, Cadeddu JA, Kavoussi LR (2001) Laparoscopic nephroureterectomy for the treatment of transitional cell carcinoma of the upper urinary tract. Urology 57:448–453. doi:10.1016/S0090-4295(00)01043-8
Tanaka K, Hara I, Takenaka A, Kawabata G, Fujisawa M (2008) Incidence of local and port site recurrence of urologic cancer after laparoscopic surgery. Urology 71:728–734. doi:10.1016/j.urology.2007.10.054
Hattori R, Yoshino Y, Gotoh M, Katoh M, Kamihira O, Ono Y (2006) Laparoscopic nephroureterectomy for transitional cell carcinoma of renal pelvis and ureter: Nagoya experience. Urology 67:701–705. doi:10.1016/j.urology.2005.10.022
Salomon L, Hoznek A, Cicco A, Gasman D, Chopin DK, Abbou CC (1999) Retroperitoneoscopic nephroureterectomy for renal pelvic tumors with a single iliac incision. J Urol 161:541–544. doi:10.1016/S0022-5347(01)61945-1
Hsueh TY, Huang YH, Chiu AW, Huan SK, Lee YH (2007) Survival analysis in patients with upper urinary tract transitional cell carcinoma: a comparison between open and hand-assisted laparoscopic nephroureterectomy. BJU Int 99:632–636. doi:10.1111/j.1464-410X.2006.06665.x
Oosterlinck W, Solsona E, van der Meijden AP, Sylvester R, Bohle A, Rintala E et al (2004) EAU guidelines on diagnosis and treatment of upper urinary tract transitional cell carcinoma. Eur Urol 46:147–154. doi:10.1016/j.eururo.2004.04.011
Pohar KS, Sheinfeld J (2001) When is partial ureterectomy acceptable for transitional-cell carcinoma of the ureter? J Endourol 15:405–409. doi:10.1089/089277901300189439
Roupret M, Harmon JD, Sanderson KM, Barret E, Cathelineau X, Vallancien G et al (2007) Laparoscopic distal ureterectomy and anastomosis for management of low-risk upper urinary tract transitional cell carcinoma: preliminary results. BJU Int 99:623–627. doi:10.1111/j.1464-410X.2006.06688.x
Chandhoke PS, Clayman RV, Kerbl K, Figenshau RS, McDougall EM, Kavoussi LR et al (1993) Laparoscopic ureterectomy: initial clinical experience. J Urol 149:992–997
Gerber E, Dinlenc CZ, Wagner JR (2003) Laparoscopic distal ureterectomy for low grade transitional cell carcinoma. J Urol 169:2295. doi:10.1097/01.ju.0000060883.54360.cd
Simforoosh N, Mosapour E, Maghsudi R (2005) Laparoscopic ureteral resection and anastomosis for management of low-grade transitional-cell carcinoma. J Endourol 19:287–289. doi:10.1089/end.2005.19.287
Scolieri MJ, Paik ML, Brown SL, Resnick MI (2000) Limitations of computed tomography in the preoperative staging of upper tract urothelial carcinoma. Urology 56:930–934. doi:10.1016/S0090-4295(00)00800-1
Elliott DS, Segura JW, Lightner D, Patterson DE, Blute ML (2001) Is nephroureterectomy necessary in all cases of upper tract transitional cell carcinoma? Long-term results of conservative endourologic management of upper tract transitional cell carcinoma in individuals with a normal contralateral kidney. Urology 58:174–178. doi:10.1016/S0090-4295(01)01109-8
Roupret M, Hupertan V, Traxer O, Loison G, Chartier-Kastler E, Conort P et al (2006) Comparison of open nephroureterectomy and ureteroscopic and percutaneous management of upper urinary tract transitional cell carcinoma. Urology 67:1181–1187. doi:10.1016/j.urology.2005.12.034
Oosterlinck W, Lobel B, Jakse G, Malmstrom PU, Stockle M, Sternberg C (2002) Guidelines on bladder cancer. Eur Urol 41:105–112. doi:10.1016/S0302-2838(01)00026-4
Sanchez de Badajoz E, Gallego Perales JL, Reche Rosado A, Gutierrez de la Cruz JM, Jimenez Garrido A (1995) Laparoscopic cystectomy and ileal conduit: case report. J Endourol 9:59–62
Huang J, Lin T, Xu K, Huang H, Jiang C, Han J et al (2008) Laparoscopic radical cystectomy with orthotopic ileal neobladder: a report of 85 cases. J Endourol 22:939–946. doi:10.1089/end.2007.0298
Basillote JB, Abdelshehid C, Ahlering TE, Shanberg AM (2004) Laparoscopic assisted radical cystectomy with ileal neobladder: a comparison with the open approach. J Urol 172:489–493. doi:10.1097/01.ju.0000129662.83162.2e
DeGer S, Peters R, Roigas J, Wille AH, Tuerk IA, Loening SA (2004) Laparoscopic radical cystectomy with continent urinary diversion (rectosigmoid pouch) performed completely intracorporeally: an intermediate functional and oncologic analysis. Urology 64:935–939. doi:10.1016/j.urology.2004.07.004
Hemal AK, Kolla SB, Wadhwa P, Dogra PN, Gupta NP (2008) Laparoscopic radical cystectomy and extracorporeal urinary diversion: a single center experience of 48 cases with three years of follow-up. Urology 71:41–46. doi:10.1016/j.urology.2007.08.056
Vaessen C, Mouzin M, Malavaud B, Game X, Berrogain N, Rischmann P (2004) Laparoscopic cystoprostatectomy, initial experience: 13 patients. Prog Urol 14:590–593
Menon M, Hemal AK, Tewari A, Shrivastava A, Shoma AM, El-Tabey NA et al (2003) Nerve-sparing robot-assisted radical cystoprostatectomy and urinary diversion. BJU Int 92:232–236. doi:10.1046/j.1464-410X.2003.04329.x
Pruthi RS, Wallen EM (2007) Robotic assisted laparoscopic radical cystoprostatectomy: operative and pathological outcomes. J Urol 178:814–818. doi:10.1016/j.juro.2007.05.040
Wang GJ, Barocas DA, Raman JD, Scherr DS (2008) Robotic vs open radical cystectomy: prospective comparison of perioperative outcomes and pathological measures of early oncological efficacy. BJU Int 101:89–93
Haber GP, Campbell SC, Colombo JR Jr, Fergany AF, Aron M, Kaouk J et al (2007) Perioperative outcomes with laparoscopic radical cystectomy: “pure laparoscopic” and “open-assisted laparoscopic” approaches. Urology 70:910–915. doi:10.1016/j.urology.2007.07.012
Porpiglia F, Renard J, Billia M, Scoffone C, Cracco C, Terrone C et al (2007) Open versus laparoscopy-assisted radical cystectomy: results of a prospective study. J Endourol 21:325–329. doi:10.1089/end.2006.0224
Hemal AK, Kolla SB (2007) Comparison of laparoscopic and open radical cystoprostatectomy for localized bladder cancer with 3-year oncological followup: a single surgeon experience. J Urol 178:2340–2343. doi:10.1016/j.juro.2007.08.020
Guru KA, Pruthi RS, Wallen EM, Muhltaler F, Mohler JL, Kim HL et al (2008) International robot-assisted cystectomy consortium (IRCC): immediate oncologic results after one hundred and sixty-two cases. J Urol 179 (Abstract 850)
Elbahnasy AM, Hoenig DM, Shalhav A, McDougall EM, Clayman RV (1998) Laparoscopic staging of bladder tumor: concerns about port site metastases. J Endourol 12:55–59
Simonato A, Gregori A, Lissiani A, Bozzola A, Galli S, Gaboardi F (2003) Laparoscopic radical cystoprostatectomy: a technique illustrated step by step. Eur Urol 44:132–138. doi:10.1016/S0302-2838(03)00214-8
Stolla V, Rossi D, Bladdou F, Rattier C, Ayuso D, Serment G (1994) Subcutaneous metastases after coelioscopic lymphadenectomy for vesical urothelial carcinoma. Eur Urol 26:342–343
Castillo OA, Vitagliano G (2008) Port site metastasis and tumor seeding in oncologic laparoscopic urology. Urology 71:372–378. doi:10.1016/j.urology.2007.10.064
Castillo OA, Abreu SC, Mariano MB, Tefilli MV, Hoyos J, Pinto I et al (2006) Complications in laparoscopic radical cystectomy. The South American experience with 59 cases. Int Braz J Urol 32:300–305
Simonato A, Gregori A, Lissiani A, Bozzola A, Galli S, Gaboardi F (2005) Laparoscopic radical cystoprostatectomy: our experience in a consecutive series of 10 patients with a 3 years follow-up. Eur Urol 47:785–792. doi:10.1016/j.eururo.2005.02.011
Fergany AF, Gill IS (2008) Laparoscopic radical cystectomy. Urol Clin N Am 35:455–466, viii–ix. doi:10.1016/j.ucl.2008.05.002
Conflict of interest statement
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
“Comité de Cancérologie de l’Association Française d’Urologie” (CC-AFU) as French national group of experts in urothelial carcinomas of the French Urological Association advisory board 2007–2009: Stephane Bernardini, Catherine Mazerolles, Catherine Roy, Christine Théodore.
Rights and permissions
About this article
Cite this article
Rouprêt, M., Smyth, G., Irani, J. et al. Oncological risk of laparoscopic surgery in urothelial carcinomas. World J Urol 27, 81–88 (2009). https://doi.org/10.1007/s00345-008-0349-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-008-0349-x