Abstract
Objectives
The purpose of this agreement was to establish evidence-based consensus statements on imaging of distal radioulnar joint (DRUJ) instability and triangular fibrocartilage complex (TFCC) injuries by an expert group using the Delphi technique.
Methods
Nineteen hand surgeons developed a preliminary list of questions on DRUJ instability and TFCC injuries. Radiologists created statements based on the literature and the authors’ clinical experience. Questions and statements were revised during three iterative Delphi rounds. Delphi panelists consisted of twenty-seven musculoskeletal radiologists. The panelists scored their degree of agreement to each statement on an 11-item numeric scale. Scores of “0,” “5,” and “10” reflected complete disagreement, indeterminate agreement, and complete agreement, respectively. Group consensus was defined as a score of “8” or higher for 80% or more of the panelists.
Results
Three of fourteen statements achieved group consensus in the first Delphi round and ten statements achieved group consensus in the second Delphi round. The third and final Delphi round was limited to the one question that did not achieve group consensus in the previous rounds.
Conclusions
Delphi-based agreements suggest that CT with static axial slices in neutral rotation, pronation, and supination is the most useful and accurate imaging technique for the work-up of DRUJ instability. MRI is the most valuable technique in the diagnosis of TFCC lesions. The main indication for MR arthrography and CT arthrography are Palmer 1B foveal lesions of the TFCC.
Clinical relevance statement
MRI is the method of choice for assessing TFCC lesions, with higher accuracy for central than peripheral abnormalities. The main indication for MR arthrography is the evaluation of TFCC foveal insertion lesions and peripheral non-Palmer injuries.
Key points
• Conventional radiography should be the initial imaging technique in the assessment of DRUJ instability. CT with static axial slices in neutral rotation, pronation, and supination is the most accurate method for evaluating DRUJ instability.
• MRI is the most useful technique in diagnosing soft-tissue injuries causing DRUJ instability, especially TFCC lesions.
• The main indications for MR arthrography and CT arthrography are foveal lesions of the TFCC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Distal radioulnar joint (DRUJ) instability and triangular fibrocartilage complex (TFCC) lesions are frequent clinical conditions that are often misdiagnosed and cause ulnar-sided wrist pain and dysfunction [1-6].
The critical function of the DRUJ is the pronosupination of the forearm through a complex interaction of the bones and soft tissue stabilizers with the proximal radioulnar joint, radiocapitellar joint, and interosseous membrane [1-4].
The etiology of DRUJ instability is multifactorial, and distal radius fractures, ulnar styloid fractures, and TFCC injuries are the leading causes. TFCC lesions are the primary cause of ulnar-sided wrist pain, and if the insertion of the distal radioulnar ligaments is injured, DRUJ instability can develop [1-4].
Imaging is key to the diagnostic workup for DRUJ instability and TFCC injuries. A variety of static and dynamic diagnostic imaging techniques are being proposed for the work-up of DRUJ instability and TFCC injuries, including radiography, computed tomography (CT), magnetic resonance imaging (MRI), CT arthrography, and MR arthrography [7-10]. Although there is increasing research, there are substantial uncertainties regarding the optimal diagnostic imaging work-up of wrist instability in clinical practice [1, 2, 11, 12].
The I-WRIST 2021 group of radiologists and hand surgeons was established to provide interdisciplinary consensus statements on imaging of post-traumatic wrist instability. The current work belongs to a two-part series. The first part was focused on scapholunate joint instability [13].
The purpose of this research was to establish evidence-based consensus statements on the imaging of DRUJ instability and TFCC injuries by experts using the Delphi technique for consensus building.
Materials and methods
Methods of the present article were identical and simultaneous to the first part of this project [13]. Panelist selection, questions to hand surgeons, literature research, literature database distribution to the panelists, project leader and task group nomination, Delphi process, and statistical analysis were performed at the same time as the first project. Details are provided in the appendix.
Questions
In the first step, hand surgeons were asked to submit questions to the radiologists on potentially problematic or controversial issues related to the imaging of DRUJ instability and TFCC injuries.
The surgeons were also asked to select the most relevant clinical classifications to illustrate to radiologists the clinical relevance of imaging in the surgical decision-making process.
A preliminary list of nine questions regarding DRUJ instability and TFCC injuries was developed (Table 1). The selected classifications were the Palmer classification of TFCC lesions [14] (Table 2), the Atzei classification of peripheral tears of the TFCC [15-17] (Table 3), and the del Piñal classification of Palmer class 1B injuries [18] (Table 4).
Bibliographic search strategy
A word search of MEDLINE and the Cochrane Library using the terms “imaging,” “radiographs,” “magnetic resonance imaging,” “computed tomography,” “ultrasonography,” “TFCC injury,” “TFCC tear,” “DRUJ instability,” and “DRUJ injury” revealed 894 articles published between January 2010 and January 2020. Subsequently, radiologists were asked to supplement the literature database with additional publications.
This left three meta-analyses, 90 articles, and 6 book chapters that formed the evidence base for the Delphi process and were archived in a cloud-based directory accessible to radiologists.
Task groups
The project leaders (T.D., I.S.S.) nominated experts into separate task groups. For consecutive Delphi rounds, each task group developed one statement as an answer to the assigned question in Table 1, followed by a short discussion and a list of references. The scientific evidence level according to the 5-point scale developed by the Oxford Centre for Evidence-Based Medicine was assigned to every article of the discussion by the experts of each task group [19].
The panelists were asked to classify their degree of agreement with each statement according to an 11-point Likert-type scale, in which 0 reflects complete disagreement, 5 reflects neither agreement nor disagreement, greater than or equal to 8 (≥ 8) reflects agreement, and 10 reflects complete agreement.
The end of the Delphi process was predetermined at a maximum of three rounds or achievement of group consensus for each statement, whichever came first [13, 20].
In the first Delphi round, the panelists were invited to comment on the phrasing or content of the thirteen preliminary questions and statements listed in Table 1, particularly if their rating did not reflect full agreement (scoring ≤ 7). The feedback of the panelists was used to insert additional questions and rephrase the statements for the next Delphi rounds [20]. The second and third Delphi rounds included the revised and extended questions and statements and the corresponding questions and statements of the former round.
Questions and statements nos. 7–11 were added in the second Delphi round in response to panelists’ feedback to elaborate on the initial questions and statements. The final fourteen questions and statements (no. 1–no. 14) of the second and third Delphi rounds are listed in Table 5. The third and final Delphi round was limited to one question that did not achieve group consensus in the previous rounds.
Statistical analysis
Threshold values for consensus of the Delphi method have not been established [21]. A systematic review showed a broad range between 50 and 97% as the threshold for consensus in various Delphi studies, the median was 75% [22]. In general, a higher level of agreement implicates more powerful statements. Therefore, the 80% threshold value for group consensus was also used in previous ESSR-associated consensus statements on femoroacetabular impingement [23].
Group consensus of the present survey was defined as 80% or more of the panelists rating their agreement level as “8,” “9,” or “10” [13, 22]. Median and interquartile range (IQR) values are provided as measures of polarization among the panelists [21].
Results
Literature research on diagnostic imaging of DRUJ instability and TFCC injuries revealed a heterogeneous spread of scientific evidence between level 1 and level 5 according to criteria of the Oxford Centre for Evidence-Based Medicine (Table 5) [19]. Three statements achieved group consensus in the first Delphi round (statement no. 3, no. 9, no. 10), and ten in the second Delphi round (statement no. 1, no. 2, no. 4, no. 5, no. 6, no. 7, no. 8, no. 11, no. 12, no. 14). The remaining statement achieved group consensus in the third Delphi round (statement no. 13). The final questions and statements including the percentages, medians, and IQRs of agreement of the Delphi panelists are provided in Table 5.
Discussion
DRUJ instability
-
Statement no. 1: The most useful imaging technique in DRUJ instability is CT (axial CT slices of the DRUJ in neutral, pronation, and supination positions). Conventional radiography, although generally used as an initial assessment method, has significant limitations in DRUJ instability. MRI, especially MR arthrography and CT arthrography, allows the assessment of TFCC injuries causing DRUJ instability.
-
Statement no. 2: CT is the most appropriate imaging technique for providing reliable information on the shape of the sigmoid notch of the radius at the DRUJ. MRI also facilitates the evaluation of the radial sigmoid notch morphology despite limited evidence.
The DRUJ is an incongruent joint with different radii of curvature of the articular surfaces that allow rotation of the sigmoid notch of the radius on the head of the ulna and anteroposterior sliding of the articular surfaces [1, 4]. In extreme pronosupination movements, contact of the articular surfaces is limited to the volar and dorsal margins of the radial sigmoid notch, contributing significantly to DRUJ stability [24, 25]. The dorsal bone margin typically forms an acute angle, while the volar margin is more rounded, although augmented by a fibrocartilaginous ridge. In post-traumatic fractures or deficiencies of the DRUJ margins, joint stability is significantly compromised [26].
The main stabilizers of the DRUJ are soft tissues such as the joint capsule, ECU tendon, pronator quadratus muscle, and interosseous membrane, in contrast to osseous structures that contribute to only 20% of its stability [1-4, 25, 27].
Conventional radiography with two standardized projections (PA and lateral) is the initial imaging method of the DRUJ. It helps assess fractures, DRUJ joint space, degenerative changes of the DRUJ, alignment of articular surfaces, and ulnar variance [1, 2, 4].
CT is the imaging method of choice for the diagnosis of DRUJ instability (Fig. 1). CT allows evaluation of the articular surface morphology [1, 2, 28]. Dynamic assessment is the most useful technique and can be performed using static positions in neutral rotation, pronation, or supination [1, 2, 28].
A 24-year-old male with ulnar wrist pain after a motorcycle crash. a–c CT reconstructions in the coronal, axial, and 3D planes showing a fracture of the base of the ulnar styloid process with static distal radioulnar instability. Note the joint space widening (arrow in a) and the dorsal subluxation of the ulnar head (arrows in b and c)
A real-time dynamic four-dimensional CT study with variable loads makes it possible to study the movement of the joint and the interaction of its bony and soft tissue components, although its actual role needs to be better defined [1, 29].
Ultrasound assessment of DRUJ instability under load has been described but has not yet reached a significant spread [30].
The primary role of MRI, CT arthrography, and MR arthrography in DRUJ instability is the evaluation of soft tissue injuries, especially of the TFCC [1, 2].
-
Statement no. 3: Plain radiography with an appropriate measuring method and positioning provides reliable information on the ulnar variance.
The term ulnar variance refers to the relative length of the distal articular surfaces of the ulna and radius [31]. The standardized posteroanterior wrist radiograph is the reference standard method for determining ulnar variance [32, 33]. However, this measurement can usually be reliably performed in CT and MRI studies, with minor differences that are not clinically significant [32, 33].
TFCC injuries
-
Statement no. 4: High-resolution MRI, MR arthrography, and CT arthrography allow an accurate assessment of the location and extent of full-thickness Palmer class 1 TFCC injuries. MR arthrography and high-resolution CT 3D arthrography techniques with radial reconstruction centered on the ulnar styloid process provide a precise evaluation of the different types of noncommunicating partial thickness lesions of the TFCC.
Palmer classification of TFCC lesions (Table 2) divides TFCC injuries into traumatic (class 1) and degenerative (class 2) injuries. Traumatic injuries are subdivided based on the anatomical location of the injury into four subtypes (A–D) [14]. Class 1A and 1B injuries are the most frequent subtypes of traumatic injuries [34], although class 2 derangements become particularly frequent in older adults [35].
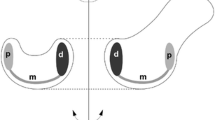
Traumatic lesions of the TFCC might be stable or unstable, causing instability of DRUJ. Palmer class 1A injuries are stable. Complete or partial foveal Palmer 1B lesions, 1C lesions, and 1D lesions, when they affect the insertion of the distal radioulnar ligaments, with or without fracture, produce DRUJ instability to a greater or lesser degree [3, 5] (Fig. 2).
Diagrams illustrating the primary unstable lesions of the TFCC: Palmer class 1B lesion unstable subtypes (a–d). a Foveal TFCC tear. b Foveal TFCC tear associated with ulnar styloid process fracture or pseudoarthrosis. c Complete TFCC ulnar detachment. d Complete TFCC ulnar detachment associated with styloid fracture or pseudoarthrosis. Palmer class 1D lesion unstable subtypes (e–h). e Radial avulsion of the dorsal distal radioulnar ligament. f Radial avulsion of the volar distal radioulnar ligament. g Avulsion of the distal radioulnar ligament (volar or dorsal) with associated fracture. h Complete radial detachment of the TFCC (so-called floating styloid)
Few studies have analyzed the diagnostic efficacy of MRI, MR arthrography, and CT arthrography in traumatic injuries of the TFCC with arthroscopic or surgical correlation as a “gold standard” [35-42]. Three published meta-analyses [11, 12, 42] and one systematic review [43] show significant methodological shortcomings in most of the studies reviewed and generally lack robust analysis of the diagnostic accuracy of the different subtypes of TFCC lesions.
The most recent meta-analysis by Treiser et al [12] included 28 studies comparing the diagnostic accuracy of MRI, MR arthrography, and CT arthrography in assessing TFCC lesions with arthroscopic or open surgical findings as the gold standard. This meta-analysis demonstrated MRI, MR arthrography, and CT arthrography sensitivities of 0.76, 0.78, and 0.89, respectively, with specificities of 0.82, 0.85, and 0.89. CT arthrography and MR arthrography had statistically equivalent sensitivity and specificity for diagnosing TFCC lesions. In all imaging modalities, diagnostic accuracy was higher in central TFCC lesions than in peripheral lesions [12].
-
Statement no. 5: Conventional MRI has a low accuracy in the diagnosis of foveal tears of TFCC (Atzei class 3). MR arthrography, with an injection of the distal radioulnar compartment, shows only moderate diagnostic accuracy in these injuries. Future research is needed.
-
Statement no. 6: Both conventional radiography and CT detect DRUJ osteoarthritis in advanced stages with subchondral remodeling. MRI and especially MR arthrography and CT arthrography allow the evaluation of osteoarthritis in early stages.
-
Statement no. 7: There is currently no evidence that imaging can assess vascularization of the peripheral TFCC or provide information on the vascularization/quality of peripheral TFCC tears.
-
Statement no. 8: The main indications for direct MR arthrography in suspected TFCC injuries are to delineate central and peripheral tears (foveal vs styloid attachment) of the TFCC and differentiate between partial- and full-thickness tears.
The ulnar insertion of the TFCC has a vertical proximal lamina inserted in the ulnar fovea and a horizontal distal lamina inserted in the ulnar styloid process [44]. Foveal insertion is the most important biomechanically. It represents the convergent point of insertion of the distal radioulnar and ulnocarpal ligaments, critical stabilizers of both the DRUJ and the ulnocarpal joint [44, 45].
Atzei has classified Palmer class 1B lesions into five subtypes, depending on which structures are affected, providing a guide for their therapeutic management (Table 3) [15-17]. Complete (Atzei class 2) and foveal (Atzei class 3) tears of the TFCC ulnar attachment lead to DRUJ instability and DRUJ osteoarthritis (Atzei class 5) [15-17].
Palmer class 1B lesions affecting the foveal insertion (Atzei class 3) are unstable lesions in which the DRUJ and radiocarpal compartments do not communicate due to the integrity of the styloid lamina [15, 46].
The MRI assessment of the foveal insertion of the TFCC requires high-quality studies [5, 46-48] (Fig. 3). Proper wrist positioning is key to assessing foveal attachment on MRI. The MRI study should be performed either with the patient prone in the “superman” position with the wrist pronated or with the patient supine, the arm at the patient’s side, and the wrist coil in a horizontal position with the wrist pronated and the palm down [5].
A 28-year-old male paddle tennis player with ulnar wrist pain. a, b Coronal and sagittal PD fat-suppressed images showing a tear of the foveal lamina of the TFCC (arrow), respecting the styloid insertion (arrowhead in a). c Axial T1 image reveals a static distal radioulnar joint instability. The ulnar head is dorsally subluxated (arrow)
No studies specifically analyze the diagnostic accuracy of MRI in class 1B foveal lesions in a significant number of patients. The actual usefulness of MRI in foveal tears of TFCC still needs to be determined [34, 49]. Detection of foveal lesions is the main indication for MR arthrography. It requires injection of the DRUJ compartment, with a reported sensitivity of 85% and a specificity of 76% [50] (Fig. 4). The assessment of the foveal lamina of the TFCC could be improved with 3D sequences and radial reconstructions centered on the ulnar fovea in both MR arthrography and CT arthrography [36, 51, 52].
A 29-year-old male professional tennis player with ulnar wrist pain. Conventional MRI studies are not conclusive. a, b Coronal and sagittal T1 fat-suppressed MR arthrography images (bicompartmental MR arthrography with distal radioulnar and midcarpal joint injection) show a rupture of the foveal insertion of the TFCC (arrows). The styloid lamina is respected (arrowhead in a). This is a noncommunicating lesion without contrast passage from the distal radioulnar joint to the radiocarpal compartment. Accurate assessment of Palmer 1B noncommunicating foveal tear is one of the main indications for MR arthrography of the wrist
The peripheral 10–40% of the TFCC is vascularized, with the central area being avascular [53], which has important therapeutic implications. MRI, MR arthrography, and CT arthrography can demonstrate retraction of Palmer 1B injuries (Atzei class 4) but do not allow assessment of vascularity or viability of TFCC lesions [17].
-
Statement no. 9: The diagnosis of horizontal and longitudinal split tears of the ulnotriquetral ligament remains challenging. On conventional MRI and MR arthrography, they are usually undetected. The diagnostic accuracy of imaging methods for Palmer class 1C lesions needs to be established.
Palmer class 1C injury (carpal avulsion of the ulnocarpal ligaments) or longitudinal tears of the ulnotriquetral ligament are rare injuries [18, 54, 55]. These lesions cause pain and possibly a component of instability of the ulnocarpal joint and, to a lesser degree, of the DRUJ [5, 18].
MRI shows poor sensitivity and specificity for detecting the longitudinal split type of ulnotriquetral ligament tear, with an overall sensitivity of 44% and specificity of 60% [55]. The diagnostic accuracy of imaging methods for Palmer class 1C lesions needs to be established [34, 54].
-
Statement no. 10: MRI and MR arthrography demonstrate partial- and full-thickness injury of the radial attachment of the volar and dorsal distal radioulnar ligaments. Associated fracture avulsion of the sigmoid notch of the radius is quite uncommon and is better demonstrated on CT or CT arthrography.
Palmer’s original description of class 1D lesions was complete avulsion of the TFCC from the radial attachment. Nakamura subdivided these 1D lesions into four subtypes [56]. Most 1D lesions are ruptures of the TFC proper attachment in the hyaline cartilage of the radial sigmoid notch (stable lesions). Less frequently, 1D lesions could extend to the dorsal or volar radioulnar ligaments, with or without avulsion fracture (unstable lesions) [56, 57].
MRI and MR arthrography facilitate an accurate diagnosis of distal radioulnar ligament tears. CT and CT arthrography better demonstrate radial avulsion fractures of these ligaments [5, 57].
-
Statement no. 11: MRI, MR arthrography, and CT arthrography can delineate and characterize additional TFCC injuries not included in Palmer’s classification (non-Palmer injuries); however, as of now, the diagnostic accuracy for these types of TFCC injuries has only been validated for MRI.
-
Statement no. 12: MRI and MR arthrography allow evaluation of capsular lesions of TFCC, although imaging accuracy has not been established.
Recent advances in arthroscopy and imaging methods have led to the description of new TFCC lesion patterns not included in the Palmer classification. These non-Palmer injuries include traumatic, degenerative, and combined injuries, such as capsular, horizontal, flap, or bucket-handle tears [18, 34, 58-62]. Del Piñal [18] described and systematized capsular lesions for the first time, differentiating between dorsal capsular detachment, volar capsular detachment, and dorsal capsular detachment from the triquetrum with focal synovitis (Nishikawa lesion) (Table 5). Dorsal capsular lesions affecting the capsular insertion of the dorsal radioulnar ligament and/or the ECU subsheath are the most common non-Palmer lesions [18, 63, 64]. Volar capsular detachments and Nishikawa’s lesions are rare [18].
Few studies with a small number of cases have analyzed the diagnostic capacity of MRI in diagnosing lesions not included in Palmer’s classification. MRI, MR arthrography, and CT arthrography could facilitate the diagnosis of these lesions, although more studies are needed to demonstrate this [34].
Other soft-tissue stabilizers of the DRUJ
-
Statement no. 13: None of the imaging techniques have been shown to be reliable at assessing the interosseous membrane.
-
Statement no. 14: Dynamic ultrasound and MRI with stress maneuvers (e.g., maximum supination) provide information about extensor carpi ulnaris tendon stability.
Injury to secondary stabilizing soft tissue structures, such as the DRUJ joint capsule, distal oblique band of the forearm interosseous membrane (DOB), ECU, and pronator quadratus muscle, may contribute to DRUJ instability [1-4, 27].
The DOB is a secondary stabilizer of the DRUJ with an anatomical and functional relationship to the TFCC [1-4]. The DOB can be visualized with ultrasound and MRI [65, 66]. However, the accuracy of imaging methods to assess the DOB lesion in patients with DRUJ instability has not been studied.
ECU subluxation is secondary to rupture or attenuation of the infratendinous extensor retinaculum or subsheath of the ECU [67, 68]. The diagnosis of ECU instability is initially clinical. ECU instability can be constitutional and, if asymptomatic, does not require treatment [69, 70]. Symptomatic patients present with ulnar wrist pain and/or painful dynamic snapping. Ultrasound is the imaging method of choice in diagnosing ECU instability allowing dynamic examination in pronosupination. ECU displacement is maximal in supination, especially if combined with wrist flexion [71] (Fig. 5). MRI can accurately show ECU subsheath injuries and associated injuries [68]. Real-time dynamic MRI or static MRI in fixed positions could be useful in diagnosing ECU and DRUJ instability but is infrequently performed [69].
A 25-year-old recreational tennis player with painful dynamic snapping. a Axial ultrasound image of the dorsal aspect of the wrist showing a slight irregularity of the radial aspect of the subsheath of the extensor carpi ulnaris tendon (arrow in a). The extensor carpi ulnaris tendon maintains a normal position in the sigmoid notch with the wrist in pronation. b Corresponding axial ultrasound image in supination and flexion of the wrist showing dynamic dislocation of the extensor carpi ulnaris tendon (arrow in b)
There are limitations to this study that are inherent to the Delphi process. Empirical peer-reviewed evidence is preferred whenever diagnostic and management pathways are being considered but when this is absent then expert opinion must be substituted. Opinion may vary from clinician to clinician, and between institutes, countries, and healthcare systems. The Delphi method, when properly applied, provides a systematic, structured process to aggregate, evaluate, and summarize limited scientific evidence in which a majority of experts can converge towards an optimal answer [20]. The process reduces the impact of marginal opinions on the final consensus statements. The large number of panelists (n = 27) from eleven different countries including the USA and most of Europe ensured that the consensus statements were based on broad expert opinions and that the opinion is likely to be generalizable across these medical communities. However, most musculoskeletal radiologists with an academic background were from Europe. Therefore, the expert panel may bias against the perspective of non-academic radiologists, particularly outside Europe.
Conclusions
Conventional radiography should be the initial imaging method to assess DRUJ instability. CT with static axial slices in neutral rotation, pronation, and supination is the method of choice in evaluating DRUJ instability. MRI is the most useful technique in the diagnosis of soft-tissue injuries, especially TFCC lesions. The main indication for MR arthrography and CT arthrography are the suspicion of noncommunicating foveal lesions.
Imaging studies with arthroscopy correlation as the standard of reference are needed to determine the actual diagnostic performance of MRI, MR arthrography, and CT arthrography for the detection of Palmer 1B noncommunicating injuries, injuries at the radial attachments of the distal radioulnar ligaments, capsular injuries, and other non-Palmer injuries.
Abbreviations
- CT:
-
Computed tomography
- DOB:
-
Distal oblique band of the interosseous membrane
- DRUJ:
-
Distal radioulnar joint
- ECU:
-
Extensor carpi ulnaris
- IQR:
-
Interquartile range
- I-WRIST 2021:
-
International Wrist Radiologic evaluation for the Instability of the Scapholunate and DRUJ/TFCC
- MRI:
-
Magnetic resonance imaging
- TFCC:
-
Triangular fibrocartilage complex
References
Gulati A, Wadhwa V, Ashikyan O, Cerezal L, Chhabra A (2019) Current perspectives in conventional and advanced imaging of the distal radioulnar joint dysfunction: review for the musculoskeletal radiologist. Skeletal Radiol 48(3):331–348
Amrami KK, Moran SL, Berger RA, Ehman EC, Felmlee JP (2010) Imaging the distal radioulnar joint. Hand Clin 26(4):467–475
Nakamura T (2012) Anatomy and biomechanics of the distal radioulnar joint (DRUJ). In: del Piñal F, Mathoulin C, Nakamura T (eds) Arthroscopic Management of Ulnar Pain. Springer, Heidelberg, pp 15–23
Kleinman WB (2007) Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am 32(7):1086–1106
Cerezal L, de Dios B-M, Canga A et al (2012) MR and CT arthrography of the wrist. Semin Musculoskelet Radiol 16(1):27–41
Cody ME, Nakamura DT, Small KM, Yoshioka H (2015) MR imaging of the triangular fibrocartilage complex. Magn Reson Imaging Clin N Am 23(3):393–403
Kirchberger MC, Mühldorfer-Fodor M, Hahn P et al (2015) Update TFCC: histology and pathology, classification, examination and diagnostics. Arch Orthop Trauma Surg 135(3):427–437
Jens S, Luijkx T, Smithuis FF, Maas M (2017) Diagnostic modalities for distal radioulnar joint. J Hand Surg Eur Vol 42(4):395–404
Lee RK, Ng AW, Tong CS et al (2013) Intrinsic ligament and triangular fibrocartilage complex tears of the wrist: comparison of MDCT arthrography, conventional 3-T MRI, and MR arthrography. Skeletal Radiol 42(9):1277–1285
Moser T, Khoury V, Harris PG, Bureau NJ, Cardinal E, Dosch JC (2009) MDCT arthrography or MR arthrography for imaging the wrist joint? Semin Musculoskelet Radiol 13(1):39–54
Wang ZX, Chen SL, Wang QQ et al (2015) The performance of magnetic resonance imaging in the detection of triangular fibrocartilage complex injury: a meta-analysis. J Hand Surg Eur Vol 40(5):477–484
Treiser MD, Crawford K, Iorio ML (2018) TFCC injuries: meta-analysis and comparison of diagnostic imaging modalities. J Wrist Surg 7(3):267–272
Dietrich TJ, Toms AP, Cerezal L et al (2021) Interdisciplinary consensus statements on imaging of scapholunate joint instability. Eur Radiol 31(12):9446–9458
Palmer AK (1989) Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am 14:594–606
Atzei A (2009) New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol 34(5):582–591
Atzei A, Luchetti R (2011) Foveal TFCC tear classification and treatment. Hand Clin 27(3):263–272
Atzei A, Luchetti R, Garagnani L (2017) Classification of ulnar triangular fibrocartilage complex tears. A treatment algorithm for Palmer type IB tears. J Hand Surg Eur Vol 42(4):405–414
del Piñal F (2012) The 1B Constellation: an attempt to classify Palmer 1B class. In: del Piñal F, Mathoulin C, Nakamura T (eds) Arthroscopic management of ulnar pain. Springer, Heidelberg, pp 87–97
Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence (2011) Centre for Evidence-Based Medicine, Oxford. Available via https://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf. Accessed January 14, 2021
Steurer J (2011) The Delphi method: an efficient procedure to generate knowledge. Skeletal Radiol 40(8):959–961
von der Gracht HA (2012) Consensus measurement in Delphi studies: review and implications for future quality assurance. Technol Forecast Soc Chang 79:1525–1536
Diamond IR, Grant RC, Feldman BM et al (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67(4):401–409
Mascarenhas VV, Castro MO, Rego PA et al (2020) The Lisbon Agreement on Femoroacetabular Impingement Imaging-part 1: overview. Eur Radiol 30:5281–5297
Tolat AR, Stanley JK, Trail IA (1996) A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg Br 21(5):587–994
af Ekenstam F, Hagert CG (1985) Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg 19(1):17–25
Wallwork NA, Bain GI (2001) Sigmoid notch osteoplasty for chronic volar instability of the distal radioulnar joint: a case report. J Hand Surg Am 26:454–459
Watanabe H, Berger RA, An KN, Berglund LJ, Zobitz ME (2004) Stability of the distal radioulnar joint contributed by the joint capsule. J Hand Surg Am 29(6):1114–1120
Mespreuve M, Vanhoenacker F, Verstraete K (2015) Imaging findings of the distal radio-ulnar joint in trauma. J Belg Soc Radiol 99(1):1–20
Carr R, MacLean S, Slavotinek J, Bain GI (2019) Four-dimensional computed tomography scanning for dynamic wrist disorders: prospective analysis and recommendations for clinical utility. J Wrist Surg 8(2):161–167
Hess F, Sutter R, Nagy L, Schweizer A (2016) Stability and clinical outcome after reconstruction of complete triangular fibrocartilage disruption. J Wrist Surg 5(2):124–130
Cerezal L, del Piñal F, Abascal F, García-Valtuille R, Pereda T, Canga A (2002) Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics 22(1):105–121
Serfaty A, Costa HP, Foelker CE, Filho ENK, Souza FF, Bordalo-Rodrigues M (2020) Evaluation of ulnar variance on wrist MR imaging: is it a reliable measure? Skeletal Radiol 49(5):723–730
Laino DK, Petchprapa CN, Lee SK (2012) Ulnar variance: correlation of plain radiographs, computed tomography, and magnetic resonance imaging with anatomic dissection. J Hand Surg Am 37(1):90–97
Zhan H, Bai R, Qian Z, Yang Y, Zhang H, Yin Y (2020) Traumatic injury of the triangular fibrocartilage complex (TFCC)-a refinement to the Palmer classification by using high-resolution 3-T MRI. Skeletal Radiol 49(10):1567–1579
Nozaki T, Rafijah G, Yang L et al (2017) High-resolution 3 T MRI of traumatic and degenerative triangular fibrocartilage complex (TFCC) abnormalities using Palmer and Outerbridge classifications. Clin Radiol 72(10):904.e1-904.e10
Lee YH, Choi YR, Kim S, Song HT, Suh JS (2013) Intrinsic ligament and triangular fibrocartilage complex (TFCC) tears of the wrist: comparison of isovolumetric 3D-THRIVE sequence MR arthrography and conventional MR image at 3 T. Magn Reson Imaging 31(2):221–226
Magee T (2009) Comparison of 3-T MRI and arthroscopy of intrinsic wrist ligament and TFCC tears. AJR Am J Roentgenol 192(1):80–85
Petsatodis E, Pilavaki M, Kalogera A, Drevelegas A, Agathangelidis F, Ditsios K (2019) Comparison between conventional MRI and MR arthrography in the diagnosis of triangular fibrocartilage tears and correlation with arthroscopic findings. Injury 50(8):1464–1469
Bille B, Harley B, Cohen H (2007) A comparison of CT arthrography of the wrist to findings during wrist arthroscopy. J Hand Surg Am 32(6):834–841
De Filippo M, Pogliacomi F, Bertellini A et al (2010) MDCT arthrography of the wrist: diagnostic accuracy and indications. Eur J Radiol 74(1):221–225
Schmitt R, Christopoulos G, Meier R et al (2003) Direct MR arthrography of the wrist in comparison with arthroscopy: a prospective study on 125 patients. Rofo 175(7):911–919
Smith TO, Drew B, Toms AP, Jerosch-Herold C, Chojnowski AJ (2012) Diagnostic accuracy of magnetic resonance imaging and magnetic resonance arthrography for triangular fibrocartilaginous complex injury: a systematic review and meta-analysis. J Bone Joint Surg Am 94(9):824–832
Andersson JK, Andernord D, Karlsson J, Fridén J (2015) Efficacy of magnetic resonance imaging and clinical tests in diagnostics of wrist ligament injuries: a systematic review. Arthroscopy 31(10):2014–2020
Nakamura T, Makita A (2000) The proximal ligamentous component of the triangular fibrocartilage complex. J Hand Surg Br 25(5):479–486
Haugstvedt JR, Berger RA, Nakamura T, Neale P, Berglund L, An KN (2006) Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am 31(3):445–451
Ehman EC, Hayes ML, Berger RA, Felmlee JP, Amrami KK (2011) Subluxation of the distal radioulnar joint as a predictor of foveal triangular fibrocartilage complex tears. J Hand Surg Am 36(11):1780–1784
Zhan H, Zhang H, Bai R, Qian Z, Liu Y, Zhang H, Yin Y (2017) High-resolution 3-T MRI of the triangular fibrocartilage complex in the wrist: injury pattern and MR features. Skeletal Radiol 46(12):1695–1706
Ringler MD (2013) MRI of wrist ligaments. J Hand Surg 38(10):2034–2046
Haims AH, Schweitzer ME, Morrison WB et al (2002) Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol 178(2):419–422
Rüegger C, Schmid MR, Pfirrmann CW, Nagy L, Gilula LA, Zanetti M (2007) Peripheral tear of the triangular fibrocartilage: depiction with MR arthrography of the distal radioulnar joint. AJR Am J Roentgenol 188(1):187–192
Moritomo H, Arimitsu S, Kubo N, Masatomi T, Yukioka M (2015) Computed tomography arthrography using a radial plane view for the detection of triangular fibrocartilage complex foveal tears. J Hand Surg Am 40(2):245–251
Grunz J-P, Gietzen CH, Luetkens K et al (2020) The importance of radial multiplanar reconstructions for assessment of triangular fibrocartilage complex injury in CT arthrography of the wrist. BMC Musculoskelet Disord 21(1):286
Bednar MS, Arnoczky SP, Weiland AJ (1991) The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg 16(6):1101–1105
Tanaka T, Yoshioka H, Ueno T, Shindo M, Ochiai N (2006) Comparison between high-resolution MRI with a microscopy coil and arthroscopy in triangular fibrocartilage complex injury. J Hand Surg Am 31(8):1308–1314
Ringler MD, Howe BM, Amrami KK, Hagen CE, Berger RA (2013) Utility of magnetic resonance imaging for detection of longitudinal split tear of the ulnotriquetral ligament. J Hand Surg Am 38(9):1723–1727
Nakamura T (2010) Radial side tear of the triangular fibrocartilage complex. In: del Piñal F, Mathoulin C, Luchetti R (eds) Arthroscopic management of distal radius fractures. Springer, Heidelberg, pp 89–98
Morisawa Y, Nakamura T, Tazaki K (2007) Dorsoradial avulsion of the triangular fibrocartilage complex with an avulsion fracture of the sigmoid notch of the radius. J Hand Surg European 32(6):705–708
Estrella EP, Hung LK, Ho PC, Tse WL (2007) Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy 23(7):729–737
Abe Y, Tominaga Y, Yoshida K (2012) Various patterns of traumatic triangular fibrocartilage complex tear. Hand Surg 17(2):191–198
Schmitt R, Grunz JP, Langer M (2022) Triangular fibrocartilage complex injuries - limitations of the current classification systems and the proposed new “CUP” classification. J Hand Surg Eur Vol 13:17531934221121932
Jose J, Arizpe A, Barrera CM et al (2018) MRI findings in bucket-handle tears of the triangular fibrocartilage complex. Skeletal Radiol 47(3):419–424
Boutin RD, Fritz RC (2021) Displaced flap tears of the triangular fibrocartilage complex: frequency, flap Location, and the “comma” sign on wrist MRI. AJR Am J Roentgenol 217(3):707–708
Abe Y, Moriya A, Tominaga Y, Yoshida K (2016) Dorsal tear of triangular fibrocartilage complex: clinical features and treatment. J Wrist Surg 5(1):42–46
Haugstvedt JR, Søreide E (2017) Arthroscopic management of triangular fibrocartilage complex peripheral injury. Hand Clin 33(4):607–618
Kim YH, Gong HS, Park JW et al (2017) Magnetic resonance imaging evaluation of the distal oblique bundle in the distal interosseous membrane of the forearm. BMC Musculoskelet Disord 18(1):47
Okada K, Moritomo H, Miyake J et al (2014) Morphological evaluation of the distal interosseous membrane using ultrasound. Eur J Orthop Surg Traumatology 24(7):1095–1100
MacLennan AJ, Nemechek NM, Waitayawinyu T, Trumble TE (2008) Diagnosis and anatomic reconstruction of extensor carpi ulnaris subluxation. J Hand Surg Am 33(1):59–64
Jeantroux J, Becce F, Guerini H et al (2011) Athletic injuries of the extensor carpi ulnaris subsheath: MRI findings and utility of gadolinium-enhanced fat-saturated T1-weighted sequences with wrist pronation and supination. Eur Radiol 21(1):160–166
Luijkx T, Buckens CF, van Seeters T, Pegge SA, Maas M (2019) ECU tendon subluxation: a nonspecific MRI finding occurring in all wrist positions irrespective of ulnar-sided symptoms? Eur J Radiol 116:192–197
Petchprapa CN, Meraj S, Jain N (2016) ECU tendon “dislocation” in asymptomatic volunteers. Skeletal Radiol 45(6):805–812
Lee KS, Ablove RH, Singh S et al (2009) Ultrasound imaging of normal displacement of the extensor carpi ulnaris tendon within the ulnar groove in 12 forearm–wrist positions. AJR Am J Roentgenol 193(3):651–655
Funding
This study has received funding by The European Society of Musculoskeletal Radiology, which covered the expenses for the statistician of the I-WRIST 2021 interdisciplinary consensus statement project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Luis Cerezal (first author), Iwona Sudoł-Szopińska and Tobias Dietrich (senior authors).
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Małgorzata Mańczak kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was not required for this study because neither patients nor volunteers were directly included as participants.
Ethical approval
Institutional Review Board approval was not required because required because patients nor volunteers were directly included as participants. Thus, Institutional Review Board approval was not required because the present study fulfills the conditions for not requiring official approval for operation according the Swiss Federal Act on Research Involving Human Beings (Human Research Act).
Methodology
• prospective
• not applicable
• multicenter study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cerezal, L., del Piñal, F., Atzei, A. et al. Interdisciplinary consensus statements on imaging of DRUJ instability and TFCC injuries. Eur Radiol 33, 6322–6338 (2023). https://doi.org/10.1007/s00330-023-09698-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09698-7