Abstract
Objectives
To quantify hepatocellular carcinoma (HCC) and liver parenchyma stiffness using MR elastography (MRE) and serum alpha fetoprotein (AFP), before and 6 weeks (6w) after 90Y radioembolisation (RE), and to assess the value of baseline tumour and liver stiffness (TS/LS) and AFP in predicting response at 6w and 6 months (6 m).
Methods
Twenty-three patients (M/F 18/5, mean age 68.3 ± 9.3 years) scheduled to undergo RE were recruited into this prospective single-centre study. Patients underwent an MRI exam at baseline and 6w following RE (range 39–47 days) which included MRE using a prototype 2D EPI sequence. TS, peritumoural LS/LS remote from the tumour, tumour size, and AFP were measured at baseline and at 6w. Treatment response was determined using mRECIST at 6w and 6 m.
Results
MRE was technically successful in 17 tumours which were classified at 6w as complete response (CR, n = 7), partial response (PR, n = 4), and stable disease (SD, n = 6). TS and peritumoural LS were significantly increased following RE (p = 0.016, p = 0.039, respectively), while LS remote from tumour was unchanged (p = 0.245). Baseline TS was significantly lower in patients who achieved CR at 6w (p = 0.014). Baseline TS, peritumoural LS (both AUC = 0.857), and AFP (AUC = 0.798) showed fair/excellent diagnostic performance in predicting CR at 6w, but were not significant predictors of OR or CR at 6 m.
Conclusion
Our initial results suggest that HCC TS and peritumoural LS increase early after RE. Baseline TS, peritumoural LS, and AFP were all significant predictors of CR to RE at 6w. These results should be confirmed in a larger study.
Key Points
• Magnetic resonance elastography–derived tumour stiffness and peritumoural liver stiffness increase significantly at 6 weeks post radioembolisation whereas liver stiffness remote from the tumour is unchanged.
• Baseline tumour stiffness and peritumoural liver stiffness are lower in patients who achieve complete response at 6 weeks post radioembolisation.
• Baseline tumour size is significantly correlated with baseline tumour stiffness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most prevalent primary liver cancer and is treated with liver transplant or resection in the early stages. However, in cases of advanced HCC, these options are often not possible. Locoregional therapy such as Yttrium 90 (90Y) radioembolisation (RE) has been used to successfully downstage HCC tumours for local tumour control or to serve as a bridge to liver transplantation [1]. At our institution, early-stage patients planned for liver transplantation also undergo locoregional therapy while waiting. During RE, 90Y glass microspheres are administered through intra-arterial hepatic infusion in a segmental or lobar fashion. The diameter of the glass microspheres is too large to pass to venous circulation and they become trapped in the tumour capillary bed, delivering a high radiation dose to the arterially perfused tumour while sparing the predominantly portal-venously perfused liver parenchyma [2].
Previous reports have highlighted radiological findings following RE [3]. The standard criteria for HCC response are the modified response evaluation criteria in solid tumours (mRECIST) and more recently LI-RADS response criteria, which rely upon contrast-enhanced CT or MRI [4,5,6]. At our institution, patients who have received RE routinely undergo imaging at 6 weeks (6w) to assess technical efficiency and early tumour response. Non-invasive quantitative imaging techniques which can predict tumour response would be of great clinical benefit by informing clinicians on the likelihood of positive therapy outcomes. This could lead to changes in clinical management e.g. only performing therapies with likelihood of success rather than high risk, expensive treatments with very low chance of patient benefit. Diffusion-weighted imaging (DWI) is one technique which has shown promise as a predictor of tumour response post-RE [7, 8]. In addition to changes in cellularity, radiation effects include perivascular oedema, inflammation, extracellular matrix remodelling, and peritumoural liver fibrosis [9, 10]. These changes are likely to influence the mechanical microenvironment and may be measurable as a change in tissue stiffness. Tumour stiffness is determined by factors such as interstitial pressure and extracellular matrix reorganisation. These factors may impact the efficacy of RE and predict the degree of necrosis achieved following RE. MR elastography (MRE) enables the quantification of tissue stiffness and has become a widely used tool for staging liver fibrosis [11,12,13,14]. Several studies have assessed liver lesions using MRE and found it useful for lesion characterisation [15,16,17], differentiating HCC tumour grades [18], and predicting HCC recurrence [19]. There are limited reports on the use of MRE in HCC after locoregional therapy [20] and immunotherapy [21]. The cross-sectional study by Gordic et al [20] reported lower tumour stiffness (TS) in treated vs untreated HCCs (in different groups of patients), while a prospective, longitudinal study of HCC response to immunotherapy reported no significant difference in tumour stiffness at 6w following immunotherapy [21]. There is currently a lack of longitudinal studies investigating the change in stiffness of HCC tumours and surrounding liver parenchyma following RE.
The aim of our initial study was to quantify early changes in HCC and liver parenchyma stiffness using MRE and serum AFP, before and 6w after RE, and to assess the value of baseline tumour and liver stiffness (TS/LS) and AFP in predicting treatment response at 6w and 6 months (6 m).
Methods
Patients
This single-centre prospective study was compliant with the Health Insurance Portability and Accountability Act and approved by the local institutional review board. Between July 2016 and December 2017, a signed informed consent was obtained from 23 treatment-naïve patients (M/F 18/5, mean age 68.3 ± 9.3 years, range 55–93 years) with radiologically diagnosed HCC who were scheduled to undergo clinically indicated RE. Of the 23 patients, 3 declined to undergo repeat research imaging at 6w so only baseline data were available. The mean duration between baseline MRI and RE was 37 ± 25 days (range 3–117 days), with follow-up MRI occurring 42 ± 2 days (range 39–47 days) after RE. Patient clinical and demographic information is shown in Table 1. The patient recruitment flow chart is shown in Fig. 1.
RE treatment
Prior to RE, all patients underwent a mapping procedure with Tc-99m macroaggregated albumin (MAA). Utilising Tc-99m MAA as a surrogate for 90Y microspheres enables approximate mapping of hepatic vasculature, highlighting any arterial shunting which could cause unintended radiation dose to other areas in the body. Mapping occurred 17 ± 8 days (range 8–39 days) before RE. During RE, a microcatheter was inserted into the hepatic artery and advanced to the level of the lobar artery (n = 4) or further into segmental arterial branches (n = 19). 90Y glass microspheres (TheraSphere, Boston Scientific) were delivered through the catheter and travelled through the arterial vasculature until they were trapped in the feeding arterioles of the tumour, delivering a concentrated radiation dose. The average administered dose was 1.74 ± 0.91 GBq (range 0.80–3.77 GBq).
MRI acquisition
Baseline and follow-up imaging exams were performed on a 1.5-T MRI system (Aera, Siemens Healthineers) using an 18-channel flexible body array coil and an integrated 32-channel spine coil. Patients were instructed to fast for 4 h prior to imaging. The 2D MRE data in this study were acquired using a work-in-progress (WIP) prototype single-shot spin-echo echo-planar imaging (SE-EPI) sequence. A trapezoidal motion-encoding gradient (MEG) is inserted between the excitation and refocusing pulse which encodes motion in the slice-select direction into the MR phase signal. The frequency of the MEG was matched to the vibration frequency (60 Hz). The onset of the MEG is shifted in fixed increments, equal to the period of external vibration divided by the number of phase offsets acquired (4), relative to the external vibration. Thus, the shear wave propagation is evenly sampled over a vibration period. A 19-cm plastic paddle was placed lateral to the xiphoid process over the upper-right thorax and connected to an active pneumatic driver located outside the scan room. Sixty-hertz vibrations were applied throughout the data acquisition. Ten axial slices were acquired centred over the index lesion. Imaging parameters were repetition time 1500 ms, time to echo 48 ms, matrix size 128 × 128, field of view 360–400 mm2, slice thickness 3 mm, iPAT factor 2, and bandwidth 1502 Hz/px. Four offsets of the wave propagation were obtained in the through-plane direction in acquisition time of 15 s. Acquired 2D MRE data were reconstructed inline using a commercially available 2D multi-model direct inversion (MMDI) algorithm [22]. The algorithm produced magnitude, phase, colorised wave propagation, and elastogram images. A confidence mask was also produced which, when overlaid on the elastogram, highlighted regions of reliable measurement.
In addition to MRE, the multiparametric MRI protocol included axial and coronal T2-weighted turbo-spin-echo (HASTE), axial in- and out-of-phase, T2*/T1 mapping, and DWI. 3D T1-VIBE was acquired pre- and 1, 10, and 20 min post-injection of gadoxetic acid (0.025 mmol/kg, Eovist/Primovist). Dynamic contrast-enhanced (DCE)-MRI was also acquired during and after contrast administration. DWI and DCE-MRI data are reported elsewhere [23].
MRE image analysis
All HCC lesions on baseline and follow-up exams were identified by an abdominal radiologist (SL, observer 1) with 8 years’ experience in body MRI. An MR physicist (PK, observer 2) with 4 years of experience drew regions of interest (ROIs) in index lesions, peritumoural liver parenchyma (1.5-cm donut-shaped ROI around the lesion where possible, avoiding vessels and staying 1 cm away from the liver capsule) and in liver parenchyma remote to the treated liver segment/lobe on the MRE magnitude images using the ImageJ software (NIH) [23]. MRE ROI location was confirmed to be appropriate by observer 1. Stiffness was measured for each ROI in all captured slices with a mean value recorded, weighted by ROI size. Care was taken to include only regions within the 95% confidence map with visible wave propagation. If more than 2 lesions were identified, the largest lesion receiving RE was chosen. Necrotic tumour regions were included in the ROIs both at baseline and follow-up. Percentage stiffness change was calculated as: [(post-RE stiffness - baseline stiffness)/baseline stiffness × 100%)] for tumour (TS) and liver parenchyma (LS) peritumourally and remote to the tumour.
Assessment of tumour response
Tumour size at baseline and 6w was measured on pre-/post-contrast 3D T1-weighted images by observer 1, with the longest diameter of viable tumour recorded. Treatment response was assessed on imaging obtained at 6w and 6m following RE by observer 1. Tumour response was based on modified response evaluation criteria in solid tumours (mRECIST) using the following classifications: complete response (CR): no intratumoural arterial enhancement; partial response (PR): ≥ 30% decrease in the sum of the diameters of viable (arterially enhancing) target lesions; stable disease (SD): any case that does not qualify for either PR or progressing disease and; progressive disease (PD): ≥ 20% increase in the sum of the diameters of viable (arterially enhancing) target lesions. Patients who achieved CR or PR were classified as having an objective response (OR). The degree of tumour necrosis was determined from subtracted post-contrast 3D T1-weighted images by observer 1 [5]. The presence of haemorrhage following RE was also assessed by observer 1 based on qualitative assessment of pre-contrast T1-weighted images (as present/absent T1 hyperintense signal in the tumour). Arterial enhancement was assessed at 25–35 s post-contrast administration on DCE-MR images.
Statistical analysis
Pre- and post-RE TS and peritumoural/remote LS were compared using Wilcoxon signed-rank tests. A Kruskal-Wallis test was used to compare TS and peritumoural/remote LS at baseline. Mann-Whitney U tests were used to compare TS, peritumoural/remote LS, tumour size, and AFP (all at baseline) based on OR vs SD and CR vs PR/SD. The difference in TS at 6w in tumours with/without haemorrhage was also assessed using Mann-Whitney U tests. Spearman correlation analysis was used to determine the relationships between baseline TS and tumour size, post-treatment TS, and degree of necrosis at 6w as well as tumour size at 6w. ROC analysis was used to determine the ability of TS and peritumoural/remote LS, changes in TS and LS, tumour size, and AFP to predict response at 6w and 6m. The DeLong test was used to determine differences between AUC values. Stepwise binary logistic regression was used to identify significant combinations of MRE measures, tumour size, and AFP for prediction of response. Statistical analysis was performed using SPSS (v20, IBM Corporation). The DeLong test was performed using MedCalc (v19.2, MedCalc Software). A p value < 0.05 was considered significant.
Results
Technical success of MRE
MRE was technically successful in 20/23 (87%) patients. MRE failed in 3/23 (13%) patients due to massive ascites (n = 2) and interposed colon attenuating shear waves (n = 1). In the 20 patients with MRE at baseline, MRE data were available in tumours (n = 17), peritumoural liver parenchyma (n = 16), and liver parenchyma remote from tumour (n = 18). Three patients declined research follow at 6w. Six-week follow-up MRE data were available in tumours (n = 14), peritumoural liver parenchyma (n = 13), and liver parenchyma remote from tumour (n = 14). Factors affecting data availability were the location of MRE imaging plane, deep-lying tumours causing wave attenuation and hence poor stiffness confidence, and large tumour in the dome of liver allowing only TS measurement. Thus, pre- and post-RE MRE data were available for tumours in 14 patients, peritumoural liver parenchyma in 13 patients, and liver parenchyma remote from the tumour in 14 patients.
Tumour response
The mean tumour size at baseline was 3.6 ± 1.7 cm (range 1.5–6.3 cm). Among the patients with successful baseline TS measurements, 11/17 (65%) achieved OR (CR (n = 7), PR (n = 4)) at 6w (Fig. 2). Six patients were classified as having SD (2 had retreatment with RE, 1 had retreatment with chemoembolisation, 2 were not subsequently imaged at our institution again, and 1 was deceased before further follow-up). One patient classified as PR was lost to follow-up at 6m. Therefore, 6m follow-up clinical imaging was performed on 10/17 patients with baseline TS measures who did not undergo interval treatment, all of which achieved OR (CR (n = 7), PR (n = 3)).
Baseline stiffness
Example pre- and post-RE images are shown in Fig. 3. At baseline, mean LS remote to the tumour and in peritumoural region were not significantly different from TS (5.4 ± 2.1 vs 4.5 ± 1.3 vs 5.4 ± 2.6 kPa, respectively, p = 0.562). The mean baseline ROI size per slice was 16.1 ± 9.5 cm2 (range 35.7–6.8 cm2) for LS remote to the tumour, 4.8 ± 2.5 cm2 (range 9.3–2.2 cm2) for peritumoural LS and 4.2 ± 2.6 cm2 (range 9.6–1.4 cm2) for tumour. Combining over all slices in which the target region was included, the mean baseline volume of interest (VOI) size was 65.8 ± 44.0 cm3 (range 160.7–19.6 cm2) for LS remote to the tumour, 11.5 ± 8.1 cm3 (range 31.2–4.1 cm3) for peritumoural LS, and 12.2 ± 9.8 cm3 (range 31.6–2.4 cm2) for tumour. Baseline TS was found to significantly correlate with baseline tumour size (r = 0.746, p = 0.001; Fig. 4), while there was no significant correlation between post-RE tumour size and TS post-RE (r = 0.179, p = 0.541; Fig. 4).
MRI and MRE images from a 76-year-old female patient with cryptogenic cirrhosis and HCC pre- (top) and 6 weeks post radioembolization (RE, bottom). Top: Contrast-enhanced T1-weighted images post gadoxetate injection demonstrate arterial phase hyperenhancement (arrow) (a) and hypointensity (b) on hepatobiliary phase, with areas of increased signal (compatible with haemorrhage). c Stiffness map obtained with 2D-EPI MRE sequence illustrates ROIs for tumour (white outline), peritumoural liver tissue (black outline), and remote liver tissue (red outline). Calculated tumour stiffness was 4.1 ± 0.8 kPa, with peritumoural LS of 2.3 ± 0.6 kPa and LS remote from the tumour of 2.7 ± 0.4 kPa. Bottom: Contrast-enhanced T1-weighted images post gadoxetate injection demonstrate no arterial phase hyperenhancement (arrow) (d) and peritumoural decreased uptake (e) on hepatobiliary phase image. f Stiffness map obtained with 2D-EPI MRE sequence shows increased tumour stiffness at 8.0 ± 1.3 kPa. Similarly, peritumoural liver stiffness increased to 6.7 ± 1.4 kPa, while liver stiffness away from tumour (red outline) was grossly unchanged (2.3 ± 0.4 kPa). 6w scan included spleen MRE hence the apparent elevated spleen stiffness
Effect of RE on TS and LS
Baseline and post-RE measurements are displayed in Table 2. TS was found to significantly increase at 6w post-RE (p = 0.016; Fig. 5) by an average of 49.3 ± 62.8%. Specifically, TS increased in 12/14 (61.7 ± 58.9%) and decreased in 2 tumours (- 25.4 ± 2.9%). Peritumoural LS was also found to significantly increase following treatment (p = 0.039; Fig. 5) by an average of 38.3 ± 62.5%. Specifically, peritumoural LS increased in 10/13 patients (56.7 ± 59.3%) and decreased in 3 patients (- 22.6 ± 19.1%). LS remote from the tumour did not significantly change following RE (− 2.9 ± 17.4%, p = 0.245; Fig. 5). Post-RE TS did not correlate with the degree of tumour necrosis at 6w (r = − 0.242, p = 0.444). At 6w, 10/14 tumours were classified as haemorrhagic (based on native T1 signal). Post-RE TS was not significantly different in tumours with haemorrhage compared to those without (p = 0.242). Mean 6w ROI size per slice was 15.8 ± 5.8 cm2 (range 24.5–5.6 cm2) for LS remote to the tumour, 4.3 ± 2.9 cm2 (range 10.5–2.0 cm2) for peritumoural LS and 2.9 ± 1.7 cm2 (range 7.1–1.4 cm2) for tumours. Combining overall slices in which the target region was included, the mean baseline VOI size was 65.8 ± 44.0 cm3 (range 160.7–19.6 cm2) for LS remote to the tumour, 11.5 ± 8.1 cm3 (range 31.2–4.1 cm3) for peritumoural LS, and 12.2 ± 9.8 cm3 (range 31.6–2.4 cm2) for tumours. There was no significant difference between pre- and post-treatment ROI and VOI size for LS remote to the tumour (p = 0.075 for both), peritumoural LS (p = 0.155 and p = 0.477 respectively), and TS (p = 0.064 for both).
Linked plots showing changes in stiffness of tumour (left), peritumoural liver parenchyma (middle), and remote liver parenchyma (right) following radioembolization. Patients with tumours classified as objective response (including complete and partial response) at 6w are highlighted in blue and those classified as stable disease are highlighted in orange. TS was increased by an average of 49.3% (12/14 increased), peritumoural LS was increased by an average of 38.3% (10/13 increased), and LS remote to the tumour was reduced by an average of 2.9% (10/14 reduced)
Prediction of response at 6w and 6m
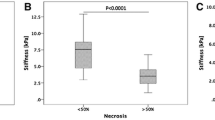
Patients who achieved CR at 6w had significantly lower baseline TS (p = 0.014) and peritumoural LS (p = 0.016) compared to patients classified as PR/SD (Table 2; Fig. 6). Although baseline TS in patients who achieved CR at 6m was lower than in those who did not, the difference was not statistically significant (p = 0.067). There was no significant difference in TS, LS, peritumoural LS, or the change in TS, LS, and peritumoural LS post-RE in patients who achieved OR vs those classified as SD (p > 0.122, Table 2). Baseline serum AFP was significantly lower in patients who achieved OR (p = 0.041) and CR (p = 0.025) at 6w compared to those who did not. There was no significant difference in serum AFP between patients who achieved CR at 6m vs those who did not (p = 0.217). Baseline tumour size was not significantly different in patients who achieved OR at 6w (p = 0.633) and CR at 6w (p = 0.193) or 6m (p = 0.067).
Box plots illustrating the difference in baseline tumour stiffness in patients who achieved OR vs SD (a), patients who achieved CR vs PR and SD (c), and patients in all three response groups (e). Peritumoural liver stiffness in patients who achieved OR vs SD (b), patients who achieved CR vs PR and SD (d), and patients in all three response groups (f) is also shown. CR, complete response; PR, partial response; SD, stable disease; OR, objective response (CR + PR)
The results from ROC analyses are displayed in Table 3. ROC analysis showed that baseline TS and baseline peritumoural LS were both significant predictors of CR at 6w (AUC 0.857, p = 0.015, AUC 0.857, p = 0.017, respectively), although these factors proved not to be significant predictors of OR at 6w or CR at 6m. LS remote from the tumour was not predictive of response at 6w or 6m. Changes in TS and peritumoural/remote LS were not associated with OR at 6w and CR at 6w or 6m (AUC 0.432–0.572, p = 0.232–0.838). Baseline tumour size was not significantly associated with response (AUC 0.577–0.630, p = 0.526–0.710). Baseline serum AFP was a significant predictor of OR (AUC 0.798, p = 0.039) and CR (AUC 0.798, p = 0.025) at 6w but was not a significant predictor of response at 6m. DeLong tests found no significant differences between the diagnostic performance of MRE parameters and AFP in predicting CR at 6w (p = 0.76–0.91). Logistic regression identified no significant combinations of baseline measures of TS/LS, tumour size, or AFP for prediction of OR or CR at 6w or 6m.
Discussion
In this study, we assessed the changes in HCC and liver parenchyma stiffness before and after RE in patients with well-compensated liver disease. We found that TS and peritumoural LS significantly increased following RE, while LS remote from the tumour did not change following treatment. A significant correlation between baseline tumour size and TS was observed. Baseline TS and peritumoural LS as well as serum AFP were significant predictors of CR at 6w (patients who achieved CR at 6w were found to have significantly lower baseline TS and peritumoural LS and lower AFP than those who did not).
There are no prior published reports of longitudinal stiffness changes in HCC following RE. A recent study reported no significant change in HCC TS at 6w following immunotherapy [21]. The authors did note a significant positive correlation between change in TS following therapy and both overall survival and time to recurrence. We did not assess overall survival and time to recurrence in our study; however, we did not find that change in TS following therapy was a predictor of response at 6w or 6m. This may be due to the differing mechanisms of action between immunotherapy and RE. A recent study assessed TS in colorectal liver metastases after chemoembolisation and found a significant increase in TS at 6w following therapy, similar to our study [24]. These results indicate that chemoembolisation and RE both produce an early increase in TS in liver tumours following treatment. It has been previously suggested from in vitro atomic force microscopy studies that anti-cancer therapy results in increased tumour cell stiffness [25, 26]. However, at the macroscopic level probed by MRE, characteristic effects of RE such as perivascular oedema, inflammation, necrosis, and extracellular matrix restructuring [10, 27] are likely to affect measured stiffness. We see evidence of this in our results, with peritumoural liver parenchyma also demonstrating increased stiffness following RE. This change is potentially due to the radiation effect on surrounding liver parenchyma by the 90Y microspheres embedded in the tumour periphery and associated oedema and inflammation. We found no significant change in liver parenchyma stiffness remote to the tumour following RE, which supports this hypothesis.
A cross-sectional study by Gordic et al (16) reported lower TS in HCCs treated with different locoregional treatments (RE, chemoembolisation, radiofrequency ablation) vs untreated HCCs in different populations of patients. Our study has several differences from the study by Gordic et al, such as the acquisition of pre- and post-treatment stiffness data and a shorter interval between treatment and imaging (42 vs 84 days). Another difference is that of the 52 patients who underwent locoregional therapy in the study by Gordic et al, 20/52 received RE and 32 received combined chemoembolisation/radiofrequency ablation. The time course of TS changes following RE is not known. However, it is possible that a reduction in inflammation, interstitial pressure, and perivascular oedema in tumours more than 6w following RE may result in decreasing TS over time.
Baseline TS and peritumoural LS were lower in patients who achieved CR at 6w, i.e. 100% tumour necrosis. The lower baseline TS finding is in agreement with a recent ultrasound elastography study which found that lower baseline HCC stiffness resulted in a better response to chemoembolisation [28]. Another ultrasound elastography study of tumour response to neoadjuvant chemotherapy in breast cancer noted softer tumours showed greater response than stiffer tumours [29]. Basic research studies have shown that tumour extracellular matrix cross-linking modulates tumour progression in breast cancer cells [30] and elevated stiffness promotes proliferation and resistance to chemotherapy in HCC cells [31]. The finding of lower baseline peritumoural LS in patients who achieved CR at 6w suggests the surrounding liver parenchyma was less fibrotic with potentially lower inflammation than the peritumoural parenchyma in patients who did not achieve CR at 6w. A recent pre-clinical study found that HCCs developed in stiffer livers grew faster and had markedly elevated Ki-67 expression compared to HCCs in less stiff environments [32], which may reduce the efficacy of RE. Additionally, elevated parenchymal stiffness is a sign of advanced fibrosis/liver cirrhosis which can result in increased hepatic vascular resistance. Our results indicate that high TS or peritumoural LS at baseline may indicate lower chances of achieving complete response with RE and prompt consideration of adjuvant systemic therapies such as immune checkpoint inhibitors or tyrosine kinase inhibitors [33, 34]. In addition to reducing unnecessary radiation dose to the patient and potential expense associated with the treatment, an early indication of potential treatment response may ultimately allow more rapid successful treatment by obviating the need to wait for tumour size changes which may take weeks or months to occur following therapy.
We report that baseline serum AFP was a predictor of tumour response at 6w. Serum AFP has been considered a marker of tumour burden; however, several studies have reported poor performance in detecting HCC [35, 36]. The literature contains conflicting evidence regarding the utility of serum AFP in predicting both overall survival and radiological response following RE [37,38,39,40]. Further research in a larger cohort is required to confirm our results and determine whether MRE provides an advantage over (or in combination) with serum AFP. A high proportion of HCCs are unresectable; thus, predictive imaging biomarkers of tumour response such as tissue stiffness may provide a clinical benefit by informing treatment strategies and can potentially offer additional information regarding tumour biology over other measures such as serum AFP.
We found a significant correlation between tumour size and TS at baseline. This is in agreement with other studies which reported a significant [21, 41] or non-significant correlation [15] between tumour size and stiffness. Two other studies noted no significant relationship between tumour size and stiffness; however, in one study, it is not clear if the comparison was performed on untreated HCCs alone [20] and, in the other, non-enhancing or necrotic tumour regions were not included in the MRE ROI (which differs from our methodology) and the mean tumour size was larger than that found in our cohort (5.3 vs 3.2 cm) [18]. HCCs are known to display inter- and intra-tumour heterogeneity [42] and so for larger tumours, stiffness variability may occur owing to heterogenous tumour components.
In this study, all included tumours were confirmed HCCs and so there was no requirement for classification between malignant and benign tumours. Previous MRE work has shown that tumour viscoelastic properties such as storage modulus, loss modulus, and phase angle (also referred to as damping ratio in the literature) may provide additional benefit over the traditionally reported tumour stiffness (based on the magnitude of the complex shear modulus) [16, 17]. In both previous studies assessing tumour viscoelasticity, 3D MRE methods were applied which is not the case in the current study. In addition, MRE data in the current study were reconstructed using a commercial MRE inversion algorithm which does not provide additional viscoelastic parameter outputs. The change in tumour viscoelastic properties following RE and their utility for prediction of response to RE would be of interest and should be explored in future studies.
Our study has several limitations. The first is the small sample size, with only 23 subjects included in analysis, of which 14 had complete pre- and post-RE data. The second issue is a lack of pathological analysis of the lesions, as it is not common to biopsy tumours once clinical imaging criteria for HCC have been met. The third issue is a lack of MRE after 6w, which would have provided additional information about dynamic changes over time. Further prospective studies are required to inform this. The final issue is, as previously mentioned, the use of 2D MRE for tumour stiffness measurement. In 2D MRE, only the wave propagation in the through-plane axis is encoded into the MR phase image. This method has been shown to provide excellent accuracy in predicting global liver fibrosis measurement [11, 13]; however, in heterogenous tissues such as a tumour embedded in liver parenchyma, the wave propagation can become disrupted and produce aberrant stiffness measures in tumour and peritumoural parenchyma. 3D MRE captures the wave field in all three orthogonal directions and can address the issue of non-planar wave propagation. The role of 3D MRE in predicting response to therapy should be explored in future studies.
Conclusion
Our initial results indicate that there are measurable changes in TS and peritumoural LS following RE. Baseline TS, peritumoural LS, and serum AFP appear to be fair/excellent predictors of CR of HCC to RE at 6w. The exact mechanisms and time scales of TS variation following treatment have yet to be fully elucidated and prospective longitudinal studies incorporating pathological correlation with MRE stiffness measurements would be valuable.
Abbreviations
- AFP:
-
Alpha fetoprotein
- LS:
-
Liver stiffness
- MRE:
-
Magnetic resonance elastography
- RE:
-
90Y radioembolisation
- TS:
-
Tumour stiffness
- VOI:
-
Volume of interest
References
Kulik LM, Atassi B, van Holsbeeck L et al (2006) Yttrium-90 microspheres (TheraSphere) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol 94:572–586
Lewandowski RJ, Geschwind JF, Liapi E, Salem R (2011) Transcatheter intraarterial therapies: rationale and overview. Radiology 259:641–657
Semaan S, Makkar J, Lewis S, Chatterji M, Kim E, Taouli B (2017) Imaging of hepatocellular carcinoma response after (90)Y radioembolisation. AJR Am J Roentgenol 209:W263–W276
Lencioni R, Llovet JM (2010) Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 30:52–60
Gordic S, Corcuera-Solano I, Stueck A et al (2017) Evaluation of HCC response to locoregional therapy: validation of MRI-based response criteria versus explant pathology. J Hepatol 67:1213–1221
Elsayes KM, Hooker JC, Agrons MM et al (2017) 2017 Version of LI-RADS for CT and MR imaging: an update. Radiographics 37:1994–2017
Deng J, Miller FH, Rhee TK et al (2006) Diffusion-weighted MR imaging for determination of hepatocellular carcinoma response to yttrium-90 radioembolisation. J Vasc Interv Radiol 17:1195–1200
Gordic S, Wagner M, Zanato R et al (2019) Prediction of hepatocellular carcinoma response to (90)Yttrium radioembolisation using volumetric ADC histogram quantification: preliminary results. Cancer Imaging 19:29
Barker HE, Paget JT, Khan AA, Harrington KJ (2015) The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nat Rev Cancer 15:409–425
Ibrahim SM, Nikolaidis P, Miller FH et al (2009) Radiologic findings following Y90 radioembolisation for primary liver malignancies. Abdom Imaging 34:566–581
Kennedy P, Wagner M, Castera L et al (2018) Quantitative elastography methods in liver disease: current evidence and future directions. Radiology 286:738–763
Chang W, Lee JM, Yoon JH et al (2016) Liver fibrosis staging with MR elastography: comparison of diagnostic performance between patients with chronic hepatitis B and those with other etiologic causes. Radiology 280:88–97
Morisaka H, Motosugi U, Glaser KJ et al (2016) Comparison of diagnostic accuracies of two- and three-dimensional MR elastography of the liver. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25425:n/a-n/a
Yin M, Glaser KJ, Talwalkar JA, Chen J, Manduca A, Ehman RL (2016) Hepatic MR elastography: clinical performance in a series of 1377 consecutive examinations. Radiology 278:114–124
Venkatesh SK, Yin M, Glockner JF et al (2008) MR elastography of liver tumors: preliminary results. AJR Am J Roentgenol 190:1534–1540
Garteiser P, Doblas S, Daire J-L et al (2012) MR elastography of liver tumours: value of viscoelastic properties for tumour characterisation. Eur Radiol 22:2169–2177
Shahryari M, Tzschatzsch H, Guo J et al (2019) Tomoelastography distinguishes noninvasively between benign and malignant liver lesions. Cancer Res 79:5704–5710
Thompson SM, Wang J, Chandan VS et al (2017) MR elastography of hepatocellular carcinoma: correlation of tumor stiffness with histopathology features-preliminary findings. Magn Reson Imaging 37:41–45
Wang J, Shan Q, Liu Y et al (2019) 3D MR elastography of hepatocellular carcinomas as a potential biomarker for predicting tumor recurrence. J Magn Reson Imaging 49:719–730
Gordic S, Ayache JB, Kennedy P et al (2017) Value of tumor stiffness measured with MR elastography for assessment of response of hepatocellular carcinoma to locoregional therapy. Abdom Radiol (NY). https://doi.org/10.1007/s00261-017-1066-y:1-10
Qayyum A, Hwang KP, Stafford J et al (2019) Immunotherapy response evaluation with magnetic resonance elastography (MRE) in advanced HCC. J Immunother Cancer 7:329
Silva AM, Grimm RC, Glaser KJ et al (2015) Magnetic resonance elastography: evaluation of new inversion algorithm and quantitative analysis method. Abdom Imaging 40:810–817
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675
Vogl TJ, Martin SS, Johnson AA, Haas Y (2020) Evaluation of MR elastography as a response parameter for transarterial chemoembolisation of colorectal liver metastases. Eur Radiol
Lam WA, Rosenbluth MJ, Fletcher DA (2007) Chemotherapy exposure increases leukemia cell stiffness. Blood 109:3505–3508
Raudenska M, Kratochvilova M, Vicar T et al (2019) Cisplatin enhances cell stiffness and decreases invasiveness rate in prostate cancer cells by actin accumulation. Sci Rep 9:1660
Spina JC, Hume I, Pelaez A, Peralta O, Quadrelli M, Garcia Monaco R (2019) Expected and unexpected imaging findings after (90)Y transarterial radioembolisation for liver tumors. Radiographics 39:578–595
Chen R, Kong W, Gan Y et al (2019) Tumour stiffness associated with tumour response to conventional transarterial chemoembolisation for hepatocellular carcinoma: preliminary findings. Clin Radiol 74:814.e811–814.e817
Hayashi M, Yamamoto Y, Ibusuki M et al (2012) Evaluation of tumor stiffness by elastography is predictive for pathologic complete response to neoadjuvant chemotherapy in patients with breast cancer. Ann Surg Oncol 19:3042–3049
Levental KR, Yu H, Kass L et al (2009) Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell 139:891–906
Schrader J, Gordon-Walker TT, Aucott RL et al (2011) Matrix stiffness modulates proliferation, chemotherapeutic response, and dormancy in hepatocellular carcinoma cells. Hepatology 53:1192–1205
Dong Y, Zheng Q, Wang Z et al (2019) Higher matrix stiffness as an independent initiator triggers epithelial-mesenchymal transition and facilitates HCC metastasis. J Hematol Oncol 12:112
Finn RS, Qin S, Ikeda M et al (2020) Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 382:1894–1905
Lee MS, Ryoo BY, Hsu CH et al (2020) Atezolizumab with or without bevacizumab in unresectable hepatocellular carcinoma (GO30140): an open-label, multicentre, phase 1b study. Lancet Oncol 21:808–820
Lok AS, Sterling RK, Everhart JE et al (2010) Des-γ-carboxy prothrombin and α-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology 138:493–502
Trevisani F, D'Intino PE, Morselli-Labate AM et al (2001) Serum α-fetoprotein for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: influence of HBsAg and anti-HCV status. J Hepatol 34:570–575
Memon K, Kulik L, Lewandowski RJ et al (2012) Alpha-fetoprotein response correlates with EASL response and survival in solitary hepatocellular carcinoma treated with transarterial therapies: a subgroup analysis. J Hepatol 56:1112–1120
Riaz A, Ryu RK, Kulik LM et al (2009) Alpha-fetoprotein response after locoregional therapy for hepatocellular carcinoma: oncologic marker of radiologic response, progression, and survival. J Clin Oncol 27:5734–5742
Spreafico C, Sposito C, Vaiani M et al (2018) Development of a prognostic score to predict response to Yttrium-90 radioembolisation for hepatocellular carcinoma with portal vein invasion. J Hepatol 68:724–732
Bhutiani N, O'Brien SJ, Priddy EE et al (2020) Correlating serum alpha-fetoprotein in hepatocellular carcinoma with response to Yttrium-90 transarterial radioembolisation with glass microspheres (TheraSphere™). HPB (Oxford). https://doi.org/10.1016/j.hpb.2019.12.007
Hennedige TP, Hallinan JTPD, Leung FP et al (2016) Comparison of magnetic resonance elastography and diffusion-weighted imaging for differentiating benign and malignant liver lesions. Eur Radiol 26:398–406
Friemel J, Rechsteiner M, Frick L et al (2015) Intratumor heterogeneity in hepatocellular carcinoma. Clin Cancer Res 21:1951–1961
Acknowledgements
The authors thank the participants for their time and are grateful to the MR technologists for assistance with imaging.
Funding
This study was funded through NCI U01 CA172320.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Bachir Taouli.
Conflict of interest
The other authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
The patients reported in this study have been reported previously. There is no overlap in MR data between the studies. MR elastography data reported here has not been previously reported.
Methodology
• prospective
• Observational - longitudinal study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kennedy, P., Lewis, S., Bane, O. et al. Early effect of 90Y radioembolisation on hepatocellular carcinoma and liver parenchyma stiffness measured with MR elastography: initial experience. Eur Radiol 31, 5791–5801 (2021). https://doi.org/10.1007/s00330-020-07636-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07636-5