Abstract
Objectives
To investigate the effect of neoadjuvant chemotherapy (NAC) on breast tissue composition with mammographic automated volumetric measurement.
Methods
This retrospective study included 168 breast cancer patients who were treated with NAC and underwent serial mammography (pre-treatment, mid-treatment, and post-treatment) between January 2015 and October 2018. Automated volumetric measurements of the contralateral breast volume (BV), fibroglandular volume (FGV), and breast density (BD) were performed using Volpara software. BD grades were divided into 4 groups by Volpara density grade (VDG). The longitudinal changes in BV, FGV, BD, and their associated factors were evaluated.
Results
Repeated-measures analysis of variance demonstrated a significant reduction in BV, FGV, and BD over time (p < 0.001, p < 0.001, and p = 0.002, respectively). BV showed a greater reduction in the second half than in the first half (− 28.6 cm3 vs. − 15.2 cm3), BD showed a greater reduction in the first half than in the second half (− 0.8% vs. − 0.1%), and FGV steadily decreased (− 4.6 cm3 and − 3.9 cm3 in the first and second halves). On multivariable linear regression analysis, chemotherapy regimen was associated with BV change between pre- and post-treatment (p = 0.002); age (p = 0.024) and VDG (p = 0.027) were associated with FGV change; age (p = 0.037), VDG (p = 0.002), and chemotherapy regimen (p = 0.003) were associated with BD change.
Conclusions
NAC affects breast tissue composition, reflected as reductions in BV, FGV, and BD. Mammography with automated volumetric measurement can capture quantitative changes in these breast tissue parameters during NAC.
Key Points
• Neoadjuvant chemotherapy (NAC) affects breast tissue composition with different patterns of reduction in breast volume, fibroglandular volume, and breast density.
• Age, Volpara density grades, and NAC regimen were independent factors associated with breast density change between pre-treatment and post-treatment.
• Mammography with automated volumetric measurement enables identification of longitudinal changes in breast tissue composition.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemotherapy (NAC) has become a standard treatment for locally advanced breast cancer and an important treatment option even for patients with early breast cancer; its multiple advantages include downstaging of primary tumor, reducing axillary nodal burden, eliminating micrometastatic disease, and providing prognostic information through direct observation of systemic therapeutic efficacy [1]. The conventional breast imaging modalities of mammography and ultrasound are used serially over the course of treatment for loco-regional staging, assessment of tumor response, and providing information about the presence or size of residual tumor burden [2,3,4]. NAC regimens are typically combinations of cytotoxic therapeutic agents that destroy cancer cells by damaging their DNA and interfering with cell division. Intravenous administration of cytotoxic agents has systemic effects involving the contralateral breast and other organs as well as the affected (diseased) breast. It is well understood that chemotherapy induces impairment of ovarian function with subsequent hormonal suppression leading to decreased estrogen secretion [5, 6]. Although it is biologically plausible that the normal glandular tissue of the breast may be changed in composition during NAC, few magnetic resonance imaging (MRI) studies have demonstrated a reduction in contralateral breast density (BD) [7, 8].
Automated mammographic measurement of BD can be performed with commercially available Volpara software. This technology measures volumetric BD by creating a density map derived from x-ray attenuation at each pixel, converting the attenuation to an estimate of the tissue composition using a reference point that corresponds to fat [9, 10]. This technology takes into account the region of the breast that is not in direct contact with the compression paddle (i.e., curved breast edge) using their physical model. We hypothesized that this method could be used to quantify the effects of chemotherapy on contralateral breast tissue. Data on longitudinal BD, breast volume (BV), and fibroglandular volume (FGV) change over the course of NAC and the factors that determine those changes could elucidate the mechanism underlying systemic effects of NAC. Thus, we aimed to investigate the effect of NAC on the contralateral breast using mammography with automated volumetric assessment.
Materials and methods
Patients
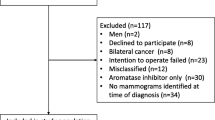
The Institutional Review Board of our institution approved this retrospective, observational study and waived the need for informed consent. The study subjects were 231 patients who were diagnosed with breast cancer and treated with NAC between January 2015 and October 2018. The imaging protocol in our institution for the assessment of tumor response to NAC included serial mammography study performed pre-treatment (baseline mammography before NAC treatment), mid-treatment (first follow-up mammography during NAC treatment), and post-treatment (second follow-up mammography after NAC treatment) (Fig. 1). The exclusion criteria were (a) lack of three serial mammograms (n = 34), (b) receipt of NAC regimens off-protocol (n = 16), (c) bilateral breast cancers (n = 9), (d) incomplete NAC because of tumor progression or adverse event (n = 3), and (e) change in NAC regimen (n = 1). Of the total patients, 168 (mean age, 48.6 ± 8.6 years [standard deviation]; range, 27–69 years) were included.
Flow diagram of the study protocol. NAC = neoadjuvant chemotherapy, MG = mammography. MGPre is the baseline mammography before NAC (pre-treatment), MGMid is the first follow-up mammography after NAC (mid-treatment), and MGpost is the second follow-up mammography after NAC/before surgery (post-treatment)
NAC mainly consisted of a taxane-based regimen with doxorubicin, cyclophosphamide, and docetaxel (ACT) based on the National Comprehensive Cancer Network (NCCN) guidelines [11]. For patients with human epidermal growth factor receptor 2 (HER2)–positive breast cancers, one of two HER2-targeted therapy regimens (trastuzumab and pertuzumab) was offered based on oncologists’ preference and economic considerations: doxorubicin, cyclophosphamide, docetaxel, and trastuzumab (ACTH); or docetaxel, carboplatin, trastuzumab, and pertuzumab (TCHP). In the ACT and ACTH groups, AC was given for the first 4 cycles and replaced with T or TH for the second 4 cycles. In the TCHP group, the combination was administered for all 6 cycles. Hence, NAC consisted of 8 cycles for the ACT and ACTH groups and 6 cycles for the TCHP group, and each cycle interval was 3 weeks. Mid-treatment mammography was performed after 4 cycles in the ACT and ACTH groups and after 3 cycles in the TCHP group.
Mammographic analysis
All images were obtained using one full-field digital mammography unit (Lorad Selenia, Hologic) with standard craniocaudal and mediolateral oblique views for each breast. Volpara commercial software (version 1.5.1, Volpara Health Technology) was used for fully automated volumetric analysis (Fig. 2). Volpara calculates BV, FGV, and BD automatically per breast (by averaging the craniocaudal and mediolateral oblique values). Volpara algorithm uses relative (as opposed to absolute) physics modeling and was described previously [9, 12]. This method is characterized as using a reference level as a calibration object that corresponds to entirely fatty tissue (usually near the chest wall) to find the thickness of dense tissue at each pixel estimated by the x-ray attenuation of that pixel. FGV is determined by integration of thickness of dense tissue over the image, while the BV is determined by multiplying the area of the breast by the recorded breast thickness. BD is the percentage ratio of the FGV and BV and ranges from 0 to 40%. Density grades were divided into 4 groups by Volpara density grade (VDG). The threshold for grades A, B, C, and D was 0.0–4.5%, 4.5–7.5%, 7.5–15.5%, and ≥ 15.5% (in percent dense volume), respectively.
A 42-year-old woman with right breast cancer. A screenshot of volumetric measurement for mammographic density using the Volpara software (a) Contralateral normal mammogram before neoadjuvant chemotherapy (b, pre-treatment), at the first follow-up (c, mid-treatment) and the second follow-up (d, post-treatment) after neoadjuvant chemotherapy. The percentage mammographic density decreased by 5.1% from 14.4 to 9.3% at the first follow-up, further decreased by 2.1% from 9.3 to 7.2% at the second follow-up
Data and statistical analysis
The clinical data included age at cancer diagnosis, menopausal status, body mass index (BMI), American College of Radiology (ACR) breast density categories, VDG, clinical TNM stage, chemotherapy regimen, HER2-targeted therapy, chemotherapy duration, and mammographic interval. The following histopathological information was obtained: histological type and grade; estrogen receptor (ER), progesterone receptor (PR), and HER2 status; and pathological complete response (pCR). Tumors expressing ER and/or PR were defined as hormone receptor (HR)–positive. A HER2 score of 0 or 1 was considered HER2-negative, a value of 3 was considered HER2-positive, and a value of 2 was considered equivocal. For equivocal cases, silver-enhanced in situ hybridization was performed, and those with a HER2/CEP17 ratio of ≥ 2 or a HER2/CEP17 ratio of < 2 and an average HER2 copy number of ≥ 6 were considered HER2-positive.
Changes in BV, FGV, and BD were analyzed using repeated-measures analysis of variance (RM-ANOVA) with the Bonferroni post hoc test. The mean changes in BV, FGV, and BD between mammograms were compared using paired t test. The percentage change was calculated as the change in the mean BV, FGV, and BD divided (normalized) by the value at baseline or mid-treatment. The mean changes and mean percentage changes in BV, FGV, and BD were compared among subgroups using the independent t test for two subgroups and analysis of variance (ANOVA) among three or more subgroups. Univariable and multivariable linear regression analyses were performed to identify the factors affecting the change in BV, FGV, and BD between pre- and post-treatment. For analyses, continuous variables (age, BMI, and chemotherapy duration) were categorized into binary groups according to their median values. Variables which were significantly associated (p < 0.05) in the univariable analysis were entered into the multivariable model. All statistical analyses were performed with the statistical software MedCalc version 17.1. All p values of less than 0.05 were considered statistically significant.
Results
Patient characteristics
Of the 168 enrolled patients, 112 (66.7%) patients received a regimen of ACT, 28 patients (16.7%) received a regimen of ACTH, and 28 patients (16.7%) received a regimen of TCHP (Table 1). HER2-targeted therapy was used in 56 patients (33.3%). The mean age was 48.6 years (range, 27–69 years) among all patients, 47.8 years (range, 27–69 years) in the ACT group, 52.1 (range years, 37–69 years) in the ACTH group, and 47.9 years (range, 30–66 years) in the TCHP group. The mean duration of chemotherapy was 4.7 months (range, 3.4 to 5.8 months). The mean interval of mammography between pre- and mid-treatment was 2.8 months (range, 1.6 to 4.2 months) and that of mammography between mid- and post-treatment was 2.6 months (range, 1.0 to 3.9 months). The mean BV, FGV, and BD at pre-treatment mammography were 551.2 cm3 (range, 73.8 to 2630.6 cm3), 67.7 cm3 (range, 12.4 to 189.4 cm3), and 15.0% (range, 3.6 to 39.1%), respectively.
Serial changes in BV, FGV, and BD
One way RM-ANOVA demonstrated a significant reduction in BV, FGV, and BD in the overall treatment population (p < 0.001, p < 0.001, and p = 0.002, respectively; Table 2) and in patients receiving an ACT regimen (p = 0.002, p < 0.001, and p < 0.001, respectively). For patients receiving an ACTH regimen, however, there were no significant changes in BV, FGV, and BD (all p > 0.05). Patients receiving a TCHP regimen showed a significant reduction in BV and increase in BD (p < 0.001 and p = 0.010, respectively) but not in FGV (p = 0.157). Regarding the percentage change, there were significant differences according to the chemotherapy regimen in BV (p < 0.001) and BD (p < 0.001). FGV also demonstrated differences according to the chemotherapy regimen; however, the differences did not reach statistical significance (p = 0.158).
The pattern of change over the course of NAC was different among the 3 parameters. For BV, a greater reduction occurred in the second half of the treatment period (between mid- and post-treatment, − 28.6 cm3) than in the first half (between pre- and mid-treatment, − 15.2 cm3); post hoc RM-ANOVA revealed a significant reduction between mid- and post-treatment periods (p < 0.001), whereas it showed only a reduction of borderline significance between pre- and mid-treatment periods (p = 0.083). FGV decreased rather steadily; the amount of reduction was similar and statistically significant in both the first and second halves (− 4.6 cm3 and − 3.9 cm3, respectively; p = 0.002 and p < 0.001). For BD, a greater reduction was found in the first half (− 0.8%) than in the second half of the treatment course (− 0.1%); post hoc tests revealed a significant decrease between pre- and mid-treatment (p = 0.001), whereas it showed no significant difference between mid- and post-treatment (p = 1.00). The mean changes in BV and FGV between pre- and post-treatment were − 43.8 cm3 (range, − 544.7 to 307.1 cm3) and − 8.5 cm3 (range, − 81.2 to 83.5 cm3), while the mean change in BD was − 0.9% (range, − 13.6 to 9.2%) (Tables S1–2).
Regarding change in VDG, 24 patients (14.5%) showed decreased VDG at post-treatment mammograms when compared with the findings at pre-treatment mammograms, where most of the patients (n = 128, 76.2%) had stable VDG and 16 (9.5%) had increased VDG (Table S3). Regarding the change in ACR density categories, most of the patients (n = 166, 98.8%) had stable ACR categories during NAC, whereas one patient had decreased ACR categories and another had increased ACR categories at mid- or post-treatment mammograms, when compared with the findings at pre-treatment mammograms.
Factors affecting changes in BV, FGV, and BD
In the univariable linear regression analysis of the change in BV between the pre- and post-treatment periods (Table 3), BMI (p = 0.023), ACR breast density categories (p = 0.001), VDG (p = 0.018), and chemotherapy regimen (p = 0.004) were significantly correlated and entered into the multivariable model, except for ACR breast density categories due to multicollinearity with VDG. Multivariable regression analysis identified only chemotherapy regimen (p = 0.002) as an independent factor associated with the BV change; the mean reduction in BV was greater in patients receiving the TCHP regimen (− 112.9 cm3) than in those receiving the ACT or ACTH regimen (− 30.0 cm3, p < 0.001).
In the univariable regression analysis of the change in FGV between the pre- and post-treatment periods (Table 4), age (p < 0.001), menopausal status (p < 0.001), VDG (p < 0.001), HER2-targeted therapy (p = 0.035), and HER2 status (p = 0.035) were significantly correlated and entered into the multivariable model, except for menopausal status and HER2 status due to multicollinearity with age and HER2-targeted therapy, respectively. Multivariable regression analysis showed that age (p = 0.024) and VDG (p = 0.027) were independent factors associated with the FGV change. Mean reduction in FGV was greater in patients with younger age (≤ 48 years, − 13.6 cm3) and higher VDG (C or D, − 10.2 cm3) than in those with older age (> 48 years, − 2.9 cm3) and lower VDG (A or B, − 0.7 cm3; p < 0.001 and p = 0.009, respectively).
In the univariable regression analysis of the change in BD between the pre- and post-treatment periods (Table 5), age (p < 0.001), menopausal status (p = 0.001), VDG (p < 0.001), chemotherapy regimen (p < 0.001), HER2-targeted therapy (p = 0.002), hormonal receptor status (p = 0.031), HER2 status (p = 0.002), and pCR (p = 0.006) were significantly correlated and entered into the multivariable model, except for menopausal status and HER2 status due to multicollinearity with age and HER2-targeted therapy, respectively. Multivariable regression analysis showed that age (p = 0.037), VDG (p = 0.002), and chemotherapy regimen (p = 0.003) were independent factors associated with the BD change. Mean reduction in BD was greater in patients with younger age (≤ 48 years, − 2.0%), higher VDG (C or D, − 1.2%), and ACT or ACTH regimen (− 1.4%) than in those with older age (> 48 years, 0.3%), lower VDG (A or B, 0.6%), and TCHP regimen (1.6%), respectively (p < 0.001, p = 0.016, and p < 0.001, respectively).
Discussion
Temporal change in breast tissue composition associated with hormonal replacement therapy or tamoxifen treatment, as a risk factor for breast cancer development or a surrogate marker for treatment response, has been extensively investigated. However, the effects of chemotherapy on breast tissue composition have rarely been reported [13,14,15,16,17]. In this longitudinal study, using mammography and automated volumetric measurement, we observed a significant reduction in 3 parameters of breast tissue composition (BV, FGV, and BD) during NAC. Mean reduction in BD between pre- and post-treatment was 0.9% overall and 1.6% in patients receiving an ACT regimen; this amount of change is slightly lower than that observed in the previous MRI study involving only the ACT regimen (1.8% reduction). Also noteworthy is the varied pattern of change among the 3 parameters over the course of NAC. BV showed a greater reduction in the second half of the NAC treatment period (between mid- and post-treatment) than in the first half (between pre- and mid-treatment). In contrast, FGV decreased steadily throughout the treatment period. Hence, BD (defined as FGV divided by BV) showed a greater reduction in the first half of the treatment period than in the second half. This pattern of temporal change in multiple breast tissue composition parameters indicates a possible mechanism of BD change in the early treatment period. In addition, our study findings suggest that the effect of NAC on glandular tissue is steady over the course of treatment. A larger reduction in BV in the second half is possibly due to weight loss associated with treatment-induced gastrointestinal symptoms or toxicity [18]; however, there was a lack of weight information at each mammographic examination in our study. In a previous study, the authors found that 9 out of 44 patients had a false increase in BD which originated from BV loss [8]. Therefore, our study findings suggest that change in BD should be interpreted carefully in light of other breast tissue composition variables, especially BV, because the non-dense area is easily changeable by body weight change longitudinally [19].
Dissimilar patterns of change of BV, FGV, and BD suggest that the effect of NAC (cytotoxicity or ovarian suppression) on glandular and fatty tissue may occur in different ways. Histological change due to chemotherapy might explain the reduction in the breast tissue composition parameters. In a previous study, lobular atrophy was found in 65% of patients who received NAC, indicating that chemotherapy may more selectively affect terminal duct lobular units corresponding to mammographically dense areas (epithelium and stroma) than fatty tissue [20, 21]. These explanations seem to be related to our finding that VDG was a factor affecting changes in FGV and BD; patients with VDG C and D showed greater reduction in FGV and BD than patients with VDG A and B. Also, similar findings had been reported that higher baseline BD was a strong predictor of greater BD reduction in tamoxifen-treated patient [15, 22, 23].
Our findings suggest that the effects on breast tissue may vary according to the type of chemotherapeutic agent. The pattern and magnitude of change in BV, FGV, and BD varied depending on the NAC regimen or administration of HER2-targeted therapy, which were independent factors for BV, FGV, and BD. In our study, greater reductions in FGV and BD occurred in patients receiving ACT regimens than in those receiving ACTH or TCHP regimens, suggesting that ACT regimens without any targeted therapy might induce more ovarian suppression. Patients receiving a TCHP regimen had a greater BV reduction than those receiving an AC or ACTH regimen; this effect pattern suggests that non-glandular (fatty) tissue was possibly reduced by the TCHP regimen. This is potentially attributable to the effect of dual inhibition of HER2 overexpression with trastuzumab and pertuzumab, which may hinder fatty acid biogenesis. Studies have revealed a bi-directional connection between HER2 and fatty acid synthase (FAS), a major lipogenic enzyme; HER2 overexpression stimulates the FAS promoter and mediates increased endogenous fatty synthesis and HER2-mediated induction of FAS is suppressible by trastuzumab and pertuzumab [24, 25]. However, future studies are needed to confirm this postulation.
Although the breast tissue composition was changed by chemotherapy, the magnitude of the changes was small, especially for BD. Thus, quantitative measurement is needed. It is usually performed with mammography and semi-automated thresholding method that is still subjective and area-based (not volumetric). MRI is considered the gold standard for density measurement; however, MRI-based methods are time- and labor-intensive, and segmentation techniques, usually with fuzzy c-means, also have limitations, especially for patients with fatty breasts, due to the low contrast between fibroglandular and fatty tissue [26]. Furthermore, MRI is still not universally utilized because of high cost, need for administration of contrast agents, and patient factors (e.g., claustrophobia and pacemaker implantation). Our findings suggest that Volpara, a fully automated volumetric measurement tool, may enable mammographic detection of small changes in breast tissue composition. However, intrinsic problems such as technical variations in mammography (position and compression) remain. The type of mammography unit can affect the BD measurement; for example, digital radiography (DR) usually has greater contrast resolution and provides a sharper image compared with computed radiography (CR) [27]. One strength of our study is that the same mammography unit was used for all patients, minimizing the risk of variation introduced by different types of mammography unit.
Our study may have the below-mentioned clinical implications; however, further studies are needed. Breast tissue composition or its change may be used as a surrogate marker for predicting contralateral second breast cancer. Mammographic density is considered an independent risk factor, and its change is known to be associated with cancer risk. In the International Breast Cancer Intervention Study (IBIS) trial, women who experienced a 10% or greater reduction in mammographic density during tamoxifen chemoprevention had a 63% decline in breast cancer risk [15]. Studies on adjuvant therapy also found that women who have a greater density reduction after tamoxifen treatment show lower rates of cancer recurrence or mortality when compared with the finding in women with a stable density [22, 28]. Thus, patients with less reduction in BD or FGV during NAC treatment have the potential risk of contralateral breast cancer and active surveillance may be needed for these patients. Moreover, considering the fact that the need of supplementary imaging increases in women with dense breasts, variability in breast tissue composition and its change according to different chemotherapy regimens may impact clinicians’ strategies for the surveillance of breast cancer survivors at increased risk.
We acknowledge several limitations of our study. First, this was a retrospective observational study in a clinical setting involving NAC regimens that included multiple chemotherapeutic agents in combination; thus, we could not identify the effects of each agent. The NAC setting in our study appears to have caused selection bias toward a higher proportion of patients with dense breasts, as Asian women tend to have denser breasts when compared with the findings in the Western women. In addition, patients with advanced breast cancers who undergo NAC may have denser breasts when compared with the finding in patients who undergo surgery without NAC, because advanced breast cancers are often correlated with symptom-detected cancers or interval cancers (masked in dense breasts). This selection bias might have overestimated the reduction in BD, considering the finding that higher baseline BD was a predictor of greater BD reduction in previous studies and this study [15, 16, 22, 23]. Second, we did not obtain menstrual cycle or body weight information, and mammographic examination was performed at predetermined intervals based on the chemotherapy. Thus, the effect of menstrual cycle or weight change on breast tissue composition was not examined. Finally, the change in BD during NAC was significant but relatively small when compared with the findings in MRI studies. This is an inherent limitation in mammography acquisition that involves technical factors such as variability in compression and positioning.
In conclusion, NAC affects breast tissue composition, causing a significant reduction in BV, FGV, and BD. Mammography with automated volumetric measurement can be used to capture quantitative changes in breast tissue composition during NAC.
Abbreviations
- ACR:
-
American College of Radiology
- ACT:
-
Doxorubicin, cyclophosphamide, and docetaxel
- ACTH:
-
Doxorubicin, cyclophosphamide, docetaxel, and trastuzumab
- ANOVA:
-
Analysis of variance
- BD:
-
Breast density
- BMI:
-
Body mass index
- BV:
-
Breast volume
- CR:
-
Computed radiography
- DR:
-
Digital radiography
- ER:
-
Estrogen receptor
- FAS:
-
Fatty acid synthase
- FGV:
-
Fibroglandular volume
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hormone receptor
- IBIS:
-
International Breast Cancer Intervention Study
- MRI:
-
Magnetic resonance imaging
- NAC:
-
Neoadjuvant chemotherapy
- NCCN:
-
National Comprehensive Cancer Network
- pCR:
-
Pathologic complete response
- PR:
-
Progesterone receptor
- RM-ANOVA:
-
Repeated-measures analysis of variance
- TCHP:
-
Docetaxel, carboplatin, trastuzumab, and pertuzumab
- VDG:
-
Volpara density grade
References
Fisher B, Bryant J, Wolmark N et al (1998) Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 16:2672–2685
Fowler AM, Mankoff DA, Joe BN (2017) Imaging neoadjuvant therapy response in breast cancer. Radiology 285:358–375
Helvie MA, Joynt LK, Cody RL, Pierce LJ, Adler DD, Merajver SD (1996) Locally advanced breast carcinoma: accuracy of mammography versus clinical examination in the prediction of residual disease after chemotherapy. Radiology 198:327–332
Rauch GM, Adrada BE, Kuerer HM, van la Parra RF, Leung JW, Yang WT (2017) Multimodality imaging for evaluating response to neoadjuvant chemotherapy in breast cancer. AJR Am J Roentgenol 208:290–299
Fornier MN, Modi S, Panageas KS, Norton L, Hudis C (2005) Incidence of chemotherapy-induced, long-term amenorrhea in patients with breast carcinoma age 40 years and younger after adjuvant anthracycline and taxane. Cancer 104:1575–1579
Poikonen P, Saarto T, Elomaa I, Joensuu H, Blomqvist C (2000) Prognostic effect of amenorrhoea and elevated serum gonadotropin levels induced by adjuvant chemotherapy in premenopausal node-positive breast cancer patients. Eur J Cancer 36:43–48
Chen JH, Nie K, Bahri S et al (2010) Decrease in breast density in the contralateral normal breast of patients receiving neoadjuvant chemotherapy: MR imaging evaluation. Radiology 255:44–52
Chen JH, Pan WF, Kao J et al (2013) Effect of taxane-based neoadjuvant chemotherapy on fibroglandular tissue volume and percent breast density in the contralateral normal breast evaluated by 3T MR. NMR Biomed 26:1705–1713
Jeffreys M, Warren R, Highnam R, Smith GD (2006) Initial experiences of using an automated volumetric measure of breast density: the standard mammogram form. Br J Radiol 79:378–382
Teo I, Whelehan P, Macaskill JE, Vinnicombe S, Munnoch DA, Evans A (2016) Volpara as a measurement tool for breast volume. J Plast Reconstr Aesthet Surg 69:581–582
Telli ML, Gradishar WJ, Ward JH (2019) NCCN guidelines updates: breast cancer. J Natl Compr Canc Netw 17:552–555
Destounis S, Johnston L, Highnam R, Arieno A, Morgan R, Chan A (2017) Using volumetric breast density to quantify the potential masking risk of mammographic density. AJR Am J Roentgenol 208:222–227
Persson I, Thurfjell E, Holmberg L (1997) Effect of estrogen and estrogen-progestin replacement regimens on mammographic breast parenchymal density. J Clin Oncol 15:3201–3207
Laya MB, Gallagher JC, Schreiman JS, Larson EB, Watson P, Weinstein L (1995) Effect of postmenopausal hormonal replacement therapy on mammographic density and parenchymal pattern. Radiology 196:433–437
Cuzick J, Warwick J, Pinney E et al (2011) Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case-control study. J Natl Cancer Inst 103:744–752
Kim WH, Cho N, Kim YS, Yi A (2018) Mammographic density changes following discontinuation of tamoxifen in premenopausal women with oestrogen receptor-positive breast cancer. Eur Radiol 28:3176–3184
Li J, Humphreys K, Eriksson L, Edgren G, Czene K, Hall P (2013) Mammographic density reduction is a prognostic marker of response to adjuvant tamoxifen therapy in postmenopausal patients with breast cancer. J Clin Oncol 31:2249–2256
Boussios S, Pentheroudakis G, Katsanos K, Pavlidis N (2012) Systemic treatment-induced gastrointestinal toxicity: incidence, clinical presentation and management. Ann Gastroenterol 25:106–118
Wanders JO, Bakker MF, Veldhuis WB, Peeters PH, van Gils CH (2015) The effect of weight change on changes in breast density measures over menopause in a breast cancer screening cohort. Breast Cancer Res 17:74
Aktepe F, Kapucuoglu N, Pak I (1996) The effects of chemotherapy on breast cancer tissue in locally advanced breast cancer. Histopathology 29:63–67
Moll UM, Chumas J (1997) Morphologic effects of neoadjuvant chemotherapy in locally advanced breast cancer. Pathol Res Pract 193:187–196
Nyante SJ, Sherman ME, Pfeiffer RM et al (2015) Prognostic significance of mammographic density change after initiation of tamoxifen for ER-positive breast cancer. J Natl Cancer Inst 107
Ko KL, Shin IS, You JY, Jung SY, Ro J, Lee ES (2013) Adjuvant tamoxifen-induced mammographic breast density reduction as a predictor for recurrence in estrogen receptor-positive premenopausal breast cancer patients. Breast Cancer Res Treat 142:559–567
Kumar-Sinha C, Ignatoski KW, Lippman ME, Ethier SP, Chinnaiyan AM (2003) Transcriptome analysis of HER2 reveals a molecular connection to fatty acid synthesis. Cancer Res 63:132–139
Menendez JA, Vellon L, Mehmi I et al (2004) Inhibition of fatty acid synthase (FAS) suppresses HER2/neu (erbB-2) oncogene overexpression in cancer cells. Proc Natl Acad Sci U S A 101:10715–10720
Wu S, Weinstein SP, Conant EF, Kontos D (2013) Automated fibroglandular tissue segmentation and volumetric density estimation in breast MRI using an atlas-aided fuzzy C-means method. Med Phys 40:122302
Kim WH, Moon WK, Kim SM et al (2013) Variability of breast density assessment in short-term reimaging with digital mammography. Eur J Radiol 82:1724–1730
Sandberg ME, Li J, Hall P et al (2013) Change of mammographic density predicts the risk of contralateral breast cancer--a case-control study. Breast Cancer Res 15:R57
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2017R1D1A1B03032143).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Won Hwa Kim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 47 kb)
Rights and permissions
About this article
Cite this article
Jang, H.J., Kim, H.J., Chae, Y.S. et al. Effect of neoadjuvant chemotherapy on breast tissue composition: a longitudinal mammographic study with automated volumetric measurement. Eur Radiol 30, 4785–4794 (2020). https://doi.org/10.1007/s00330-020-06830-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06830-9