Abstract
Purpose
To investigate whether monitoring with ultrasound and MR imaging before, during and after neoadjuvant chemotherapy (NAC) can predict axillary response in breast cancer patients.
Materials and methods
A total of 131 breast cancer patients with clinically positive axillary lymph node (LN) who underwent NAC and subsequent surgery were enrolled. They had ultrasound and 3.0 T-MR examinations before, during and after NAC. After reviewing ultrasound and MR images, axillary LN features and tumour size (T size) were noted. According to LN status after surgery, imaging features and their diagnostic performances were analysed.
Results
Of the 131 patients, 60 (45.8%) had positive LNs after surgery. Pre-NAC T size at ultrasound and MR was different in positive LN status after surgery (p < 0.01). There were significant differences in mid- and post-NAC number, cortical thickness (CxT), T size and T size reduction at ultrasound and mid- and post-NAC CxT, hilum, T size and T size reduction, and post-NAC ratio of diameter at MR (p < 0.03). On multivariate analysis, pre-NAC MR T size (OR, 1.03), mid-NAC ultrasound T size (OR, 1.05) and CxT (OR, 1.53), and post-NAC MR T size (OR, 1.06) and CxT (OR, 1.64) were independently associated with positive LN (p < 0.004). Combined mid-NAC ultrasound T size and CxT showed the best diagnostic performance with AUC of 0.760.
Conclusion
Monitoring ultrasound and MR axillary LNs and T size can be useful to predict axillary response to NAC in breast cancer patients.
Key Points
• Monitoring morphologic features of LNs is useful to predict axillary response.
• Monitoring tumour size by imaging is useful to predict axillary response.
• The axillary ultrasound during NAC showed the highest diagnostic performance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemotherapy (NAC) has been widely used for large or locally advanced breast cancers, allowing breast-conserving surgery by reducing cancer size, and treatment response after NAC is known to offer prognostic information [1, 2]. For patients with breast cancer undergoing NAC, axillary lymph node (LN) status is crucial to determine axillary management and has been reported to be associated with disease-free survival [3,4,5].
Currently, axillary LN dissection (ALND) is regarded as a standard-of-care management for clinically positive LNs in breast cancer patients. However, it requires a major surgery for the axilla and can cause long-term morbidity, including lymphedema or paraesthesia [6]. To overcome this, sentinel LN biopsy (SLNB) is used as an effective method in node-negative breast cancer patients with much less complication. Regarding axillary management after NAC, two prospective observational trials—the Alliance Z1071 and SENTINA trials—were conducted to evaluate the feasibility of SLNB for the negatively converted LN group after NAC in initially node-positive breast cancer patients and reported 12.6% and 14.2% of false-negative rates, respectively, which were above the accepted cut-off value of 10% [7, 8]. Interestingly, axillary ultrasound (US) after NAC was found to reduce false-negative rates to 4~9.8% [9, 10]. In this context, axillary imaging for predicting axillary pCR becomes very important for surgeons to decide axillary management after NAC.
As breast imaging is routinely performed for monitoring response to NAC, US and MR imaging are also used for monitoring axillary response in clinical practice. Previous studies reported that the sensitivity and specificity of axillary imaging after NAC are 50–70% and 58–77% for US and 57–72% and 54–72% for MR [11,12,13,14]. To the best of our knowledge, however, specific US or MR imaging features associated with axillary pCR by sequential monitoring of axillary response to NAC—before, during and after NAC—were not investigated. In particular, monitoring axillary response during NAC could be beneficial to identify responders to reduce overtreatment and non-responders to be directed to change ineffective treatment or to earlier surgical intervention [15]. Therefore, we performed the current study to investigate whether monitoring with US and MR imaging can predict axillary response in breast cancer patients before, during and after NAC.
Materials and methods
Study population
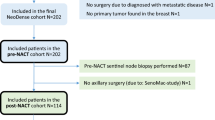
After approval of the institutional review board, the requirement of informed consent was waived. We retrospectively identified 1382 breast cancer patients who underwent surgery of the breast and axilla in our institution from January 2014 to October 2017. Of them, 172 patients received NAC and obtained US and MR imaging before, during and after NAC. The US and MR monitoring during NAC was performed after 3~4 cycles of NAC. Among them, we excluded 41 patients because of the following: (a) images were obtained in a 1.5-T MR system (n = 3), (b) MR imaging was not obtained at our hospital (n = 2), (c) axillary regions were insufficiently included on MR imaging (n = 12) and (d) axillary LNs did not show any suspicious feature, including cortical thickening more than 3 mm, round or irregular shape, or loss of fatty hilum at presentation (n = 24) [16]. We finally enrolled 131 women (mean age, 48 ± 10 years; range, 26–75 years) who demonstrated clinically positive LNs by US or MR imaging (cortical thickening more than 3 mm, round or irregular shape, or loss of fatty hilum) [16]. Of them, representative LNs of 88 patients were confirmed malignant by fine-needle aspiration biopsy.
The NAC regimen administered to all patients was according to the standard protocols of our institution, including adriamycin with docetaxel, adriamycin with cyclophosphamide, adriamycin with cyclophosphamide plus docetaxel or human epidermal growth factor receptor 2 (HER2)/neu monoclonal antibody-based chemotherapy. After NAC, all patients underwent breast-conserving surgery or mastectomy. Axillary LNs were surgically removed by SLNB (n = 22), ALND (n = 34) and both (n = 75). The results of SLNB were accepted if at least three SLNs were removed.
US technique
US examinations were performed before, during and after NAC for breast cancer and axilla by one of six radiologists with 6 to 20 years of experience in breast imaging. All patients were assessed with real-time US using a 5–12-MHz linear-array transducer (iU22; Philips Medical Systems) or a 4–15-MHz linear-array transducer (SuperSonic Imagine).
MR imaging technique
MR examinations were performed using a 3.0-T system (Achieva; Philips Medical Systems and Discovery MR750; General Electric Medical Systems) with a dedicated, four-channel breast coil. The baseline protocol consisted of turbo spin-echo T1/T2-weighted sequences and T2-weighted spin-echo series with fat suppression (repetition time/echo time ms, 5506/70; matrix, 564 × 261; field of view, 20–34 cm; sliced thickness, 3 mm). Dynamic contrast-enhanced MR examination was undergone with one pre-contrast and five post-contrast series using a fat-suppressed T1-weighted gradient echo sequence (repetition time/echo time ms, 5/2.5; matrix, 340 × 274; flip angle, 12°; field of view, 34 cm; sliced thickness, 2 mm). Gadobutrol (Gadovist, Bayer Healthcare) was injected with a dose of 0.1 mmol/kg using an automated injector (Nemoto; Nemoto Kyorindo) at a rate of 2 mL/s, followed by a 20-mL saline flush.
Image interpretation
US and MR images of the index breast cancer and axillary LN obtained before, during and after NAC were retrospectively reviewed by two radiologists in consensus. For the index breast cancer, the tumour size was determined by the largest dimension of it. For the axillary LNs with suspicious features, their number was counted. If the axillary LNs were identified two or more, the index LN was determined as the LN with the most suspicious feature which exhibits the largest cortical thickness [17]. Imaging features of the index LN were assessed as follows: longitudinal diameter, ratio of short/long diameter, cortical thickness, shape (oval, round or irregular) and hilum (normal-appearing, no or displaced hilum). Invisible LNs at US and MR during and after NAC were not included in the analysis.
Histopathologic assessment
The histologic result was assessed by one pathologist with 30 years’ experience in breast pathologic evaluation. The histologic type was assessed from histopathologic reports of US-guided core biopsies before NAC. The expression of oestrogen receptor (ER), progesterone receptor (PR) and HER2 was evaluated by the standard avidin-biotin complex immunohistochemical (IHC) staining method [17, 18]. ER and PR positivity were assessed by the Allred score, which rates the proportion of positive cells (on a 0–5 scale) and the staining intensity (on a 0–3 scale). Tumours were considered ER or PR positive if the Allred score exceeded 3. Tumours with 3+ score at IHC examination were defined as HER2 positive. If HER2 status was equivocal (2+ score) at IHC examination, gene amplification using fluorescence in situ hybridisation analysis or silver in situ hybridisation analysis was performed to determine HER2 status.
After surgery, the excised LNs were fixed in formalin, embedded in paraffin, and stained with haematoxylins and eosin. They were routinely sectioned to 2–3-mm thickness and examined. Each node was classified according to the staging system of the American Joint Committee on Cancer, and we defined benign and isolated tumour cells (≤ 0.2 mm) as axillary pCR and micro- (> 0.2–2.0 mm) and macrometastasis (> 2.0 mm) as axillary non-pCR. For the index breast cancer, pCR was defined as the absence of any invasive cancer with or without ductal carcinoma in situ.
Data and statistical analysis
Univariate analysis was performed for US and MR features of axillary LNs and the tumour size before (pre-NAC), during (mid-NAC) and after NAC (post-NAC) according to the response of axillary LN to NAC, by using independent t test for continuous variables and the chi-square or Fisher’s exact test for categorical variables. Multiple logistic regression analysis using the backward elimination method was performed for identifying independently associated features with axillary non-pCR. Receiver operator characteristic curve analysis was performed to assess the diagnostic performance of US and MR imaging features. Sensitivity, specificity, positive predictive value, negative predictive value (NPV), accuracy and the area under the receiver operating characteristic curve (AUC) were obtained at the cut-off value yielding the largest Yuden index and compared using generalized estimating equations and the DeLong method. Statistical analyses were performed using SAS ver. 9.2 (SAS Institute Inc.) with a value of p < 0.05 considered to be significant.
Results
Patients’ characteristics
Among 131 patients who underwent SLNB in 22 (16.8%) and ALND in 109 (83.2%), 71 (54.2%) achieved axillary pCR. Patients’ characteristics according to axillary response are listed in Table 1. For clinical characteristics, the non-pCR group showed a higher proportion of initial clinical stage III (58%, p = 0.048), NAC regimen of adriamycin with docetaxel (22%, p = 0.021) and the operation method of mastectomy (68%, p = 0.002) or ALND (95%, p < 0.0001) than the pCR group. For histopathologic characteristics, the non-pCR group showed a higher proportion of ER positivity (65%, p = 0.0002), hormone-positive cancer subtype (65%, p = 0.0009) and tumour non-pCR (87%, p < 0.0001) than the pCR group. The pCR group showed a higher rate of PR negativity (79%, p = 0.002). Age and tumour histologic type showed no significant difference between the two groups.
Univariate and multivariate analyses
For the univariate analysis of US features (Table 2), only larger tumour size was associated with axillary non-pCR before NAC (45 mm vs. 33 mm, p = 0.004). During NAC, larger tumour size (29 mm vs. 17 mm, p < 0.0001), reduction in tumour size (51% vs. 34%, p = 0.0002), larger number of LNs (2.2 vs. 1.6, p = 0.033) and thicker cortex of LNs (5.3 mm vs. 2.9 mm, p < 0.0001) were associated with axillary non-pCR. After NAC, larger tumour size (22 mm vs. 12 mm, p = 0.0001), larger number of LNs (1.7 vs. 1.0, p = 0.003) and thicker cortex of LNs (3.9 mm vs. 2.5 mm, p = 0.002) were associated with axillary non-pCR.
For the univariate analysis of MR features (Table 3), only larger tumour size was associated with axillary non-pCR before NAC (50 mm vs. 37 mm, p = 0.002). During NAC, larger tumour size (30 mm vs. 15 mm, p < 0.0001), reduction in tumour size (59% vs. 41%, p = 0.0005), thicker cortex of LNs (6.6 mm vs. 3.7 mm, p < 0.0001) and higher proportion of abnormal hilum (30.5% vs. 12.7%, p = 0.013) were associated with axillary non-pCR. After NAC, larger tumour size (24 mm vs. 10 mm, p < 0.0001), reduction in tumour size (74% vs. 53%, p < 0.0001), larger ratio of short/long diameter of LNs (0.6 vs. 0.5, p = 0.021), thicker cortex of LNs (4.5 mm vs. 2.6 mm, p < 0.0001) and higher proportion of abnormal hilum of LNs (26% vs. 6%, p = 0.002) were associated with axillary non-pCR.
For the multivariate analysis, pre-NAC MR tumour size (odds ratio [OR], 1.03; p = 0.002), mid-NAC US tumour size (OR, 1.05; p = 0.004), mid-NAC US cortical thickness of LNs (OR, 1.53; p = 0.0002), post-NAC MR tumour size (OR, 1.06; p = 0.004) and post-NAC MR cortical thickness of LNs (OR, 1.64; p = 0.002) were independently associated with axillary non-pCR (Table 4) (Figure 1, 2).
Axillary ultrasound and MR images of a 31-year-old woman given diagnosis of ER/PR-positive/HER2-positive breast carcinoma with a fine-needle aspiration-proven metastatic lymph node in the right breast and axilla. Ultrasound image before neoadjuvant chemotherapy (a) shows a metastatic lymph node with cortical thickening of 7.7 mm and displaced hilum, which were assessed as positive findings. The lymph node shows cortical thickening of 4.7 mm and 4 mm at US during (b) and after (c) neoadjuvant chemotherapy. The MR image before neoadjuvant chemotherapy (d) shows a metastatic lymph node with cortical thickening of 9 mm and displaced hilum. The lymph node shows cortical thickening of 5 mm and 3 mm at MR during (e) and after (f) neoadjuvant chemotherapy. The final pathology after axillary lymph node dissection revealed a residual metastatic deposit of 2 mm; therefore, this was included in the axillary non-pCR group
Axillary ultrasound and MR images of a 61-year-old woman given diagnosis of ER-negative/PR-positive/HER2-negative breast carcinoma with a fine-needle aspiration-proven metastatic lymph node in the left breast and axilla. Ultrasound image before neoadjuvant chemotherapy (a) shows a metastatic lymph node with cortical thickening of 10 mm with displaced hilum, which were assessed as positive findings. The lymph node shows cortical thickening of 3.1 mm during neoadjuvant chemotherapy (b) and disappears at US after neoadjuvant chemotherapy (c). The MR image before neoadjuvant chemotherapy (d) shows a metastatic LN with cortical thickening of 15 mm with displaced hilum. The lymph node shows cortical thickening of 2.5 mm at MR during neoadjuvant chemotherapy (e) and normal appearance at MR after neoadjuvant chemotherapy (f). Axillary lymph node dissection revealed 0.05 mm metastasis on final pathology, and this was included in the axillary pCR group
Diagnostic performance for predicting axillary lymph node status
With respect to the diagnostic performance of imaging features independently associated with axillary non-pCR (Table 5), combined mid-NAC US tumour size and cortical thickness of LNs showed the highest AUC value (0.760; 95% confidence interval, 0.680–0.841) and significantly higher sensitivity and NPV than pre-NAC MR tumour size, mid-NAC US cortical thickness of LNs and post-NAC MR tumour size (p < 0.02) which showed no significant difference in the AUCs. Post-NAC MR cortical thickness of LNs had no significant difference in diagnostic performance from combined mid-NAC US tumour size and cortical thickness of LNs.
Discussion
In the present study, we identified pre-NAC MR tumour size, mid-NAC US tumour size, mid-NAC US cortical thickness of LNs, post-NAC MR tumour size and post-NAC MR cortical thickness of LNs as imaging features independently associated with axillary response (Figs. 1 and 2). Regarding the prediction of axillary response, combined mid-NAC US tumour size and cortical thickness of LNs showed the best diagnostic performance with an AUC of 0.760, a sensitivity of 81.5% and an NPV of 80.8%.
A previous study reported that a false-negative result was associated with higher pre-NAC clinical T stage [19]. Similarly, we found that pre-NAC MR tumour size was positively associated with axillary non-pCR. The explanation for the association of larger tumour size with axillary non-pCR could be that patients with higher tumour burden may have higher probability of metastatic LNs [19]. Regarding tumour response to NAC, post-NAC MR reduction in tumour size was found to be an important independent predictor in previous reports [20, 21]. Although reduction in tumour size was not independently associated in our study, mid- and post-NAC tumour size reflecting tumour response showed independent association, which could be useful in monitoring axillary response. Regarding axillary LN features, mid- and post-NAC cortical thickness were independent predictors with higher ORs, which is comparable with post-NAC studies [22, 23]. The size, shape or hilum of LN would be related to how tumour cells infiltrate within the cortex, and even when the tumour deposit is reduced by NAC and not enough to cause LN enlargement or effacement of the hilum, the cortical thickness could reflect the tumour burden within LN [22].
With respect to minimising treatment morbidity and improving cancer-related outcome, it is critical to select candidates who would benefit from SLNB and to avoid ineffective or overtreatment [15, 24]. To predict axillary response to NAC, therefore, several studies suggested prediction models using clinical, pathological or imaging features before or after NAC [12, 20, 21, 23, 25]. However, our study encompassed pre-, mid- and post-NAC US and7 MR imaging features, and identified mid-NAC US features combined tumour size with cortical thickness of LN as the best predictor of axillary response with AUC of 0.760, comparable with previous results, ranging from 0.617 to 0.788 [12, 20, 25]. It should be emphasised that our mid-NAC US features could be helpful to guide axillary management earlier than post-NAC features of previous models. Tumour size and cortical thickness of LN as measured values can provide objective and quantitative data for the prediction of axillary response. Moreover, axillary US has advantages of wide availability, low cost, lack of contrast administration and short acquisition time over MR imaging, which can be easily accepted as mid-NAC evaluation. Further investigation is needed to validate the mid-US features for the clinical outcome and cost-benefit analysis.
We acknowledge several limitations to our study. First, this study is of a retrospective design and enrolled patients with clinically positive LNs by US or MR imaging and undergoing subsequent follow-up imaging. Fine-needle aspiration or core needle biopsy for lymph nodes showing suspicious imaging features was recommended but not mandated, and 88 of 131 (67.2%) were confirmed malignant by fine-needle aspiration biopsy. Thus, the results may have suffered from selection bias. Second, interpretation of axillary LN was based on the most suspicious finding among the axillary LNs and node-to-node evaluation could not be performed. Although we did not use special marking techniques, we assumed that the index LN with the most suspicious imaging finding represents the clinically suspicious LN. Third, the diagnostic accuracy of axillary US might be underpowered by operator dependency, which is an inherent nature of US. Lastly, the assessment of US axillary imaging was based on the captured images and real-time US evaluation of tumour size and imaging features of suspicious LNs could not be analysed, although the imaging features were assessed in consensus by two radiologists.
In conclusion, pre-NAC MR tumour size, mid-NAC US tumour size and cortical thickness of LNs, and post-NAC MR tumour size and cortical thickness of LNs were independently associated with axillary response. Combined mid-NAC US tumour size and cortical thickness of LNs can be useful to predict axillary response in breast cancer patients.
Abbreviations
- ALND:
-
Axillary lymph node dissection
- AUC:
-
The area under the receiver operating characteristic curve
- ER:
-
Oestrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- IHC:
-
Immunohistochemistry
- LN:
-
Lymph node
- NAC:
-
Neoadjuvant chemotherapy
- NPV:
-
Negative predictive value
- pCR:
-
Pathologic complete response
- PR:
-
Progesterone receptor
- SLNB:
-
Sentinel lymph node biopsy
- US:
-
Ultrasound
References
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B (2001) Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr 30:96–102
Kaufmann M, von Minckwitz G, Mamounas EP et al (2012) Recommendations from an international consensus conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol 19:1508–1516
Rouzier R, Extra JM, Klijanienko J et al (2002) Incidence and prognostic significance of complete axillary downstaging after primary chemotherapy in breast cancer patients with T1 to T3 tumors and cytologically proven axillary metastatic lymph nodes. J Clin Oncol 20:1304–1310
Hennessy BT, Hortobagyi GN, Rouzier R et al (2005) Outcome after pathologic complete eradication of cytologically proven breast cancer axillary node metastases following primary chemotherapy. J Clin Oncol 23:9304–9311
von Minckwitz G, Untch M, Blohmer JU et al (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol 30:1796–1804
Lucci A, McCall LM, Beitsch PD et al (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol 25:3657–3663
Boughey JC, Suman VJ, Mittendorf EA et al (2013) Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA 310:1455–1461
Kuehn T, Bauerfeind I, Fehm T et al (2013) Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol 14:609–618
Boughey JC, Ballman KV, Hunt KK et al (2015) Axillary ultrasound after neoadjuvant chemotherapy and its impact on sentinel lymph node surgery: results from the American College of Surgeons Oncology Group Z1071 Trial (Alliance). J Clin Oncol 33:3386–3393
Peppe A, Wilson R, Pope R, Downey K, Rusby J (2017) The use of ultrasound in the clinical re-staging of the axilla after neoadjuvant chemotherapy (NACT). Breast 35:104–108
Hieken TJ, Boughey JC, Jones KN, Shah SS, Glazebrook KN (2013) Imaging response and residual metastatic axillary lymph node disease after neoadjuvant chemotherapy for primary breast cancer. Ann Surg Oncol 20:3199–3204
You S, Kang DK, Jung YS, An YS, Jeon GS, Kim TH (2015) Evaluation of lymph node status after neoadjuvant chemotherapy in breast cancer patients: comparison of diagnostic performance of ultrasound, MRI and 18F-FDG PET/CT. Br J Radiol 88:20150143
Schipper RJ, Moossdorff M, Beets-Tan RGH, Smidt ML, Lobbes MBI (2015) Noninvasive nodal restaging in clinically node positive breast cancer patients after neoadjuvant systemic therapy: a systematic review. Eur J Radiol 84:41–47
Ha SM, Cha JH, Kim HH, Shin HJ, Chae EY, Choi WJ (2017) Diagnostic performance of breast ultrasonography and MRI in the prediction of lymph node status after neoadjuvant chemotherapy for breast cancer. Acta Radiol 58:1198–1205
Candelaria RP, Bassett RL, Symmans WF et al (2017) Performance of mid-treatment breast ultrasound and axillary ultrasound in predicting response to neoadjuvant chemotherapy by breast cancer subtype. Oncologist 22:394–401
Saffar B, Bennett M, Metcalf C, Burrows S (2015) Retrospective preoperative assessment of the axillary lymph nodes in patients with breast cancer and literature review. Clin Radiol 70:954–959
Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S (2010) American society of clinical oncology/college of american pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract 6:195–197
Wolff AC, Hammond ME, Hicks DG et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31:3997–4013
Ye BB, Zhao HM, Yu Y, Ge J, Wang X, Cao XC (2017) Accuracy of axillary ultrasound after different neoadjuvant chemotherapy cycles in breast cancer patients. Oncotarget 8:36696–36706
Kim HS, Shin MS, Kim CJ et al (2017) Improved model for predicting axillary response to neoadjuvant chemotherapy in patients with clinically node-positive breast cancer. J Breast Cancer 20:378–385
Kim R, Chang JM, Lee HB et al (2019) Predicting axillary response to neoadjuvant chemotherapy: breast MRI and US in patients with node-positive breast cancer. Radiology. https://doi.org/10.1148/radiol.2019190014:190014
Le-Petross HT, McCall LM, Hunt KK et al (2018) Axillary ultrasound identifies residual nodal disease after chemotherapy: results from the American College of Surgeons Oncology Group Z1071 Trial (Alliance). AJR Am J Roentgenol 210:669–676
Kim WH, Kim HJ, Park HY et al (2019) Axillary pathologic complete response to neoadjuvant chemotherapy in clinically node-positive breast cancer patients: a predictive model integrating the imaging characteristics of ultrasound restaging with known clinicopathologic characteristics. Ultrasound Med Biol 45:702–709
Schwartz TL, Margenthaler JA (2017) Axillary ultrasound before neoadjuvant chemotherapy for breast cancer: don’t discount the benefits yet! Ann Surg Oncol 24:618–620
Kantor O, Sipsy LM, Yao K, James TA (2018) A predictive model for axillary node pathologic complete response after neoadjuvant chemotherapy for breast cancer. Ann Surg Oncol 25:1304–1311
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Professor Ji Hyun Youk, MD, PhD, at Yonsei University College of Medicine.
Conflict of interest
The authors declare that they have no competing interests.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eun, N.L., Son, E.J., Gweon, H.M. et al. Prediction of axillary response by monitoring with ultrasound and MRI during and after neoadjuvant chemotherapy in breast cancer patients. Eur Radiol 30, 1460–1469 (2020). https://doi.org/10.1007/s00330-019-06539-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06539-4