Abstract
Introduction
Numerous publications have studied the regional anatomy of the carpal tunnel to define a “safe zone” to reduce the risk of perioperative neurovascular complications. This zone, located between the ulnar neurovascular bundle and the median nerve, is considered to be safe mainly because of the absence of vascular structures. This study aims to assess the presence of arterioles within this area using superb microvascular imaging (SMI).
Materials and methods
The images from patients who underwent a bilateral routine wrist ultrasound with SMI, between January 28 and February 28, 2019, were retrospectively reviewed by two radiologists to evaluate the presence and location of arterioles in the safe zone. In addition, cadaveric wrists injected with intra-arterial red latex underwent dissection of the carpal tunnel.
Results
The images from 27 patients (54 wrists) were reviewed. In the safe zone, arterioles were seen superficial to the retinaculum in 36 wrists (36/54; 66.7%) and deep to the retinaculum in 21 wrists (21/54; 38.9%). The arterioles located deep to the retinaculum were more frequently found close to the median nerve (21/54; 38.9%) than to the ulnar artery (9/54; 16.7%). In five cadaveric wrists, arterioles were detected superficial to the retinaculum in 3 wrists (3/5; 60%) and deep to the retinaculum in 2 wrists (2/5; 40%).
Conclusion
Arterioles can be seen in the safe zone both superficial and deep to the flexor retinaculum. Deep to the retinaculum, they are mainly observed in the proximal aspect of the carpal tunnel and more frequently close to the median nerve.
Key Points
• Superb microvascular imaging (SMI) enables the visualization of arterioles within the “safe zone” of the carpal tunnel (visible both superficial and deep to the flexor retinaculum).
• Arterioles were more frequently observed in the proximal aspect of the carpal tunnel.
• Deep to the retinaculum, arterioles were more frequently seen in proximity to the median nerve.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome is a frequent condition that leads to 140,000 surgical procedures per year in France [1]. Surgery is, as of today, the main curative intervention for this condition. However, ultrasound-guided carpal tunnel release, via a minimally invasive approach, is a recently developed ambulatory procedure and a new technique of percutaneous interventional radiology [1, 2]. This technique could reduce the risk of iatrogenic injury by using continuous ultrasound monitoring in order to visualize the median nerve, the ulnar artery, the recurrent branch of the median nerve, the superficial palmar arch, and the palmar cutaneous branch of the median nerve [1,2,3,4,5].
Thanks to a smaller cutaneous incision, the patient’s return to daily activities seems to be faster, grip strength quicker to recover, scar-related pain reduced, and scar formation accelerated [1,2,3, 6]. A punctiform percutaneous incision is performed on the palmar face at the proximal wrist crease to introduce a hook knife under ultrasound guidance. Prior to this intervention, an ultrasound examination is useful to analyze the anatomic structures of the carpal tunnel and to locate the “safe zone” that has been described as a zone located between the ulnar neurovascular bundle and the median nerve, where a retinacular section can be performed safely [1,2,3, 6, 7] (Fig. 1). It is widely considered safe because of the absence of visible vascular or nervous structures, in ultrasound or in magnetic resonance imaging [8, 9].
Transversal cross-section of the carpal tunnel and representation of the “Safe Zone.” 1, flexor retinaculum; 2, median nerve; 3, ulnar artery; 4, flexor superficialis and profundus tendons; 5, flexor carpi ulnaris tendon; 6, common synovial sheath of the flexor tendons; 7, flexor carpi radialis tendon
However, a few anatomic studies reported that small arterial branches originating from the ulnar artery cross the carpal tunnel transversely to supply the median nerve [10,11,12], the flexor tendons sheaths, and the flexor retinaculum [12,13,14] or the skin [12].
Superb microvascular imaging (or SMI) is a novel sonographic mode (Canon Medical Systems) with a higher level of sensitivity and a high frame rate for microvasculature imaging. SMI has been reported to visualize finer details of microvessels and blood flow signals in real time and has better performance in differentiating low-speed blood flow signal from tissue motion artifacts [15, 16]. Traditional ultrasonography procedures such as color Doppler and power Doppler ultrasound seem to be less suitable to show small vessels or low-velocity blood flow because of a lower sensitivity [15, 16].
The purpose of this study was to assess the presence of arterioles within the “safe zone” using SMI and to confront the results with cadaveric dissections. The detection and localization of arterioles in this area could help in avoiding their damage during mini-invasive procedures.
Materials and methods
Patients and ultrasound technique
Between January 28 and February 28, 2019, 85 patients underwent a bilateral routine wrist ultrasound in the Musculoskeletal Imaging Department of the University Hospital of Lille (France). As part of the routine ultrasound examination of the wrist, five levels of assessment of the carpal tunnel are systematically performed in our department (Fig. 2), in line with the literature [8].
The subgroup of patients who had a complete examination protocol of the carpal tunnel with SMI acquisitions were included in this retrospective analysis. Patients with chronic conditions that can affect local vascularization such as rheumatoid arthritis or carpal tunnel syndrome were not included for this first anatomical study.
All examinations were performed on an Applio i800 ultrasound device (Canon Medical Systems).
This retrospective analysis was declared and approved by the institutional board under the number DEC19-057.
Data collection and image analysis
Ultrasound images were extracted from the PACS (IntelliSpace PACS, Philips) and analyzed retrospectively together by a junior radiologist and a senior radiologist.
The primary criterion was the presence or absence of an arteriole seen in the “safe zone” on SMI. The second criterion was the localization of this arteriole.
For each image, the “safe zone” was divided into six areas of equal spacing (Fig. 3) for a reproducible mapping of the vascularization. Three areas were located on the superficial side of the retinaculum (SA, towards the ulnar artery; SN, towards the median nerve; SM, in the middle third) and three areas on the deep side of the retinaculum (DA, towards the ulnar artery; DN, towards the median nerve; DM, in the middle third).
Subdivision of the safe zone in 6 areas of equal spacing. Three areas were located on the superficial side of the retinaculum (SA, towards the ulnar artery; SN, towards the median nerve; SM, in the middle third) and three areas on the deep side of the retinaculum (DA, towards the ulnar artery; DN, towards the median nerve; DM, in the middle third). Anatomical structures 1 to 6 refer to legends in Fig. 1
Each area was rated in consensus by the readers, to assess the presence of arterioles in SMI mode, with a binary notification of 0 (if no blood flow) or 1 (if one or more vascular spots were present). To qualify as an arteriole, a SMI signal had to be associated with a compatible pulsed Doppler (PD) spectrum (Fig. 4a, b).
Anatomical study on cadavers
Five forearms of three embalmed cadavers (two males and one female) were injected by hand pump with red latex via the brachial artery to fill arterial vessels. Macro and micro-dissections of the carpal tunnel (especially, at the safe zone level) were undertaken to search for arterial vessels. These dissections were analyzed by two musculoskeletal radiologists and one anatomist.
Results
Patients included
A total of 27 patients who underwent a bilateral routine wrist ultrasound with SMI were included, leading to the analysis of images from 54 wrists. They consisted of 11 men (11/27; 40.7%) and 16 women (16/27; 59.3%). The mean age was 40.4 years (range, 20–73).
SMI analysis of the supra-retinacular region (superficial aspect of the safe zone)
When analyzing the 3 areas of the superficial aspect of the safe zone (supra-retinacular), numerous arterioles were found in SMI, as detailed in Table 1.
The highest number of arterioles was seen on the ulnar side (area SA), with up to 36/54 wrists (66.7%) displaying arterioles in this area.
The lowest number of arterioles was detected in the proximal aspect (level 1) of the median side (area SN), with 9/54 wrists (16.7%) displaying arterioles seen in SMI in this area.
The arterioles were more frequent in the distal levels of the safe zone, with 27 to 36 wrists (50.0% to 66.7%), out of 54 displaying arterioles in level 5, whereas 9 to 23 wrists (16.7% to 42.6%) had arterioles seen in SMI in the proximal level (level 1).
Anatomical correlation (supra-retinacular region)
In anatomical pieces, arterioles were seen in the supra-retinacular region in 3 wrists (3/5; 60%). They all originated from the ulnar artery and had a medial course along the flexor retinaculum and in the adjacent soft tissues (Fig. 5).
Anatomical dissection showing the supra-retinacular region of the safe zone. The flexor retinaculum (dissected) is depicted with white arrows and the proximal and distal limits of the carpal tunnel by black broken lines. The limits of the safe zone are depicted with white broken lines and double head arrows. N, median nerve; A, ulnar artery. Note the arterioles arising from the ulnar artery and running along the flexor retinaculum, clearly visible in the safe zone
SMI analysis of the infra-retinacular region (deeper aspect of the safe zone)
When analyzing the 3 areas of the deeper aspect of the safe zone (infra-retinacular), several arterioles were visualized in SMI, as detailed in Table 2.
The highest number of arterioles was seen on the median nerve side (area DN), with up to 21/54 wrists (38.9%) displaying arterioles in this area.
The lowest number of arterioles was detected in the distal aspect of the carpal tunnel, with no arterioles seen in levels 4 and 5 (0/54; 0%).
We finally noticed that arterioles were concentrated at the proximal levels of the safe zone (Table 2; levels 1 and 2) and, within these 2 levels, the closer to the median nerve the higher the concentration of arterioles. As we move away from the median nerve, the concentration of arterioles decreases (levels 3 to 5). Indeed, 9/54 (16.7%) and 4/54 (7.4%) wrists had visible arterioles using SMI on the arterial side (area DA) of levels 1 and 2 versus 21/54 (38.5%) and 12/54 wrists (22.2%) on the median nerve side (area DN) respectively.
Anatomical correlation (infra-retinacular region)
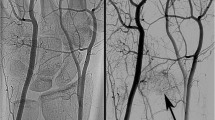
These findings were concordant with the results seen on anatomical pieces (Fig. 6a, b). Two cadaver wrists (2/5; 40%) had visible arterioles under the flexor retinaculum in the safe zone. These vessels originated from the ulnar artery and had a proximal transverse course (that was seen either just above the proximal aspect of the flexor retinaculum, or at the proximal aspect of the carpal tunnel), and then an oblique and/or longitudinal course eventually reaching the median nerve.
a Anatomical dissection showing the infra-retinacular region of the carpal tunnel. The flexor retinaculum (reclined) is depicted with white arrows and the proximal and distal limits of the carpal tunnel by black broken lines. The limits of the median nerve (N) are depicted with white broken lines. Note the arterioles (black arrows) passing through the safe zone. b Further dissection and magnification of the anatomical piece. The proximal limit of the carpal tunnel is depicted with black dotted line. The limits of the median nerve (N) are depicted with white dotted lines. Note the arterioles (black arrows) passing through the safe zone, especially running along the ulnar side of the median nerve
Discussion
Although the safe zone of the carpal tunnel has been described as a zone without any vascular structure detected on traditional imaging, our study demonstrates that arterioles can be seen within it when using superb microvascular imaging. Superficial to the flexor retinaculum, arterioles can be seen in various locations and more frequently near the ulnar artery. Arterioles were also seen deep to the flexor retinaculum, especially in the proximal levels of the carpal tunnel and more commonly close to the median nerve.
These results concur with previous anatomical descriptions regarding the fact that arterioles can cross the carpal tunnel in order to irrigate the median nerve [10,11,12], the flexor tendons sheaths [12, 13], and the flexor retinaculum, or perforate the retinaculum to supply its superficial side [12,13,14] and the skin [12]. In studies from 1988 and 1996 based upon carpal tunnel dissections of fresh cadavers, Zbrodowski et al showed that the blood supply of the flexor retinaculum comes from a superficial as well as a deep network. At the level of the carpal tunnel, the ulnar artery translates into transversal branches to constitute the main part of this superficial network. These branches can also perforate the flexor retinaculum and participate in the deep network [13, 14]. These same authors also reported that the common synovial sheath for the flexor tendons is vascularized in part by the ulnar and the radial arteries [13]. In other anatomical dissection studies, Zbrodowski et al (in 1983) and Pecket et al (in 1973) showed that the median nerve was partially supplied by the branches of the ulnar or the radial artery in the carpal tunnel [10, 11]. The precise understanding of local arterial vasculature is also crucial for procedures like the use of a synovial flap from the flexor tendon sheets to protect the median nerve from scarring [17]. Arterioles seen on SMI located on the superficial aspect of the safe zone are thus likely to play a role in the vascularization of the soft tissues, the skin, and the flexor retinaculum.
Vascular-related complications during carpal tunnel release are rare, the most frequent being hypertrophic scars and hematomas (0.9% [18] to 7.1% of complications [19]) that can even require reintervention [19]. Those were described both in endoscopic and in open surgery [20], yet not reported so far with the minimally ultrasound-guided procedure. Palmer et al analyzed the complications of the endoscopic technique and found that its most common complications are linked to vessel lacerations with ecchymosis, more frequently than ulnar or median nerve lacerations [21]. Roux et al noticed that vascular lacerations can occur with these two techniques (endoscopic and open surgery), especially when the procedure is executed with a tourniquet which hides arteries. As a consequence, vascular lacerations can create a hematoma causing adhesions and hypertrophic scar [22].
Regarding the infra-retinacular region of the Safe Zone, the arterioles observed in our study are more frequently seen towards the median nerve and often have an oblique or a longitudinal course to reach the median nerve or the flexor tendons. This orientation and proximity to the median nerve reinforce the choice of a longitudinal approach in mini-invasive techniques and suggest that, deep to the flexor retinaculum, the safest zone for arterioles does not extend as close to the median nerve as previously described. The use of ultrasound could help in detecting vessels at risk of lesion and avoid their damage during mini-invasive procedures.
The consequences of an injury of these deep arterioles have never been described. However, some of these vessels could play a role in the arterial vasculature of the median nerve as they seem to reach its epineurial region. Epineurial fibrosis, interstitial scar, and soft-tissue adhesions to the median nerve are common causes of recurrence after carpal tunnel release [23] and their precise mechanisms are yet poorly understood. Axons of the median nerve have been shown to be sensitive to ischemia in patients with carpal tunnel syndrome [24].
We cannot rule out that a perioperative injury of these small arterioles could play a role in further axonal ischemia and thus in persistent or recurrent symptoms. Further studies are needed to assess the effects of selective damage to these arterioles, and especially towards subsequent fibrosis.
As for the deeper aspect of the carpal tunnel, no arterioles were seen in SMI in the distal levels (4 and 5). Although this seems to be in agreement with previous anatomic descriptions, it is unclear however if this could also be linked to a lack of gain and/or ultrasound signal in these deep areas.
Our study has several limitations. Firstly, it was monocentric and retrospective. The interpretation of ultrasound images a posteriori can be difficult; hence, the rating phase was jointly agreed by the two readers. This strategy did not enable inter- or intra-reader agreement, but seems adequate since this study only aimed at providing a better understanding of the local anatomy and dit not aim at evaluating the intrinsic performances of SMI.
Secondly, PD was used as a reference to make sure the images displayed in SMI were arterioles. However, several images had SMI acquisitions without PD spectrum. In that case, the readers agreed not to include these images as arterioles. It is possible that this could have led to an underestimation of the number of arterioles.
Finally, the number of patients and cadavers included was limited, which can lead to variability in the observed percentages of arterioles. However, the population was consistent with the anatomical purpose of this study.
Conclusion
Although the “safe zone” of the carpal tunnel has been described as a zone without any vascular structure detected on imaging, our study demonstrates that arterioles can be seen within it using superb microvascular imaging, most of which are located above the flexor retinaculum. Arterioles can also be seen deep to the flexor retinaculum, especially in the proximal aspect of the carpal tunnel with a gradient towards the median nerve. The use of novel ultrasound techniques, such as SMI, could help in having a better description of local microvasculature and improved visualization of small arterioles, to avoid their damage during micro-invasive procedures.
This precise anatomical understanding could also lead to further prospective studies evaluating the consequences of damage to these arterioles, in terms of local complications such as bleeding, nerve ischemia, or epineurial fibrosis.
Abbreviations
- PACS:
-
Picture archiving and communication system
- PD:
-
Pulsed Doppler
- SMI:
-
Superb microvascular imaging
References
Petrover D, Richette P (2018) Treatment of carpal tunnel syndrome: from ultrasonography to ultrasound guided carpal tunnel release. Joint Bone Spine 85:545–552
Petrover D, Hakime A, Silvera J, Richette P, Nizard R (2018) Ultrasound-guided surgery for carpal tunnel syndrome: a new interventional procedure. Semin Intervent Radiol 35:248–254
Petrover D, Silvera J, De Baere T, Vigan M, Hakimé A (2017) Percutaneous ultrasound-guided carpal tunnel release: study upon clinical efficacy and safety. Cardiovasc Intervent Radiol 40:568–575
Petrover D, Bellity J, Vigan M, Nizard R, Hakime A (2017) Ultrasound imaging of the thenar motor branch of the median nerve: a cadaveric study. Eur Radiol 27:4883–4888
Seiler JG 3rd, Daruwalla JH, Payne SH, Faucher GK (2017) Normal palmar anatomy and variations that impact median nerve decompression. J Am Acad Orthop Surg 25(9):e194–e203
Nakamichi K, Tachibana S, Yamamoto S, Ida M (2010) Percutaneous carpal tunnel release compared with mini-open release using ultrasonographic guidance for both techniques. J Hand Surg Am 35:437–445
Atik TL, Smith B, Baratz ME (2001) Risk of neurovascular injury with limited-open carpal tunnel release: defining the “safe-zone”. J Hand Surg Br 26:484–487
Nakamichi K, Tachibana S (1998) Distance between the median nerve and ulnar neurovascular bundle: clinical significance with ultrasonographically assisted carpal tunnel release. J Hand Surg Am 23:870–874
Rojo-Manaute JM, Capa-Grasa A, Rodríguez-Maruri GE et al (2013) Ultra-minimally invasive sonographically guided carpal tunnel release: anatomic study of a new technique. J Ultrasound Med 32:131–142
Zbrodowski A, Buchs JB (1983) Blood supply of the median nerve in the carpal tunnel. Hand 15:310–316
Pecket P, Gloobe H, Nathan H (1973) Variations in the arteries of the median nerve. With special considerations on the ischemic factor in the carpal tunnel syndrome (CTS) Clin Orthop Relat Res 97:144–147
Omokawa S, Tanaka Y, Ryu J et al (2002) Anatomy of the ulnar artery as it relates to the transverse carpal ligament. J Hand SurgAm 27:101–104
Zbrodowski A, Gajisin S, Bednarkiewicz M (1996) The vascularization of the common synovial sheath and the tendons of the flexor muscles of the carpal tunnel. Ann Chir Main Memb Super 15:248–256
Zbrodowski A, Gajisin S (1988) The blood supply of the flexor retinaculum. J Hand Surg Br 13:35–39
Karahan AY, Arslan S, Ordahan B et al (2018) Superb microvascular imaging of the median nerve in carpal tunnel syndrome: an electrodiagnostic and ultrasonographic study. J Ultrasound Med 37(12):2855–2861
Chen J, Chen L, Wu L et al (2017) Value of superb microvascular imaging ultrasonography in the diagnosis of carpal tunnel syndrome: compared with color Doppler and power Doppler. Medicine (Baltimore) 96:e6862
Pelissier P, Alet JM, Morchikh A et al (2015) Arterial vascularization of the flexor digitorum superficialis synovial flap. An anatomical study. Chir Main 34:193–196
Mathen SJ, Nosrati NN, Merrell GA (2018) Decreased rate of complications in carpal tunnel release with hand fellowship training. J Hand Microsurg 10:26–28
Zhang D, Blazar P, Earp BE (2019) Rates of complications and secondary surgeries of mini-open carpal tunnel release. Hand (NY) 14(4):471–476
Hong JT, Lee SW, Han SH et al (2006) Anatomy of neurovascular structures around the carpal tunnel during dynamic wrist motion for endoscopic carpal tunnel release. Neurosurgery 58:ONS127–ONS133
Palmer AK, Toivonen DA (1999) Complications of endoscopic and open carpal tunnel release. J Hand Surg Am 24:561–565
Roux J-L (2004) Traitement des complications de la chirurgie du canal carpien. Chir Main 23:S178–S187
Jones NF, Ahn HC, Eo S (2012) Revision surgery for persistent and recurrent carpal tunnel syndrome and for failed carpal tunnel release. Plast Reconstr Surg 129:683–692
Han SE, Boland RA, Krishnan AV et al (2009) Ischaemic sensitivity of axons in carpal tunnel syndrome. J Peripher Nerv Syst 14:190–200
Acknowledgments
The authors would like to thank Julien ADAM, Cassandre DUVINAGE, Benjamin LEJEUNE, and Quentin SION (medical students) who contributed to the cadaveric study.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Thibaut Jacques.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sergeant, AC., Badr, S., Saab, M. et al. Carpal tunnel ultrasound: is the “safe zone” on the ulnar side of the median nerve really avascular?. Eur Radiol 30, 887–894 (2020). https://doi.org/10.1007/s00330-019-06416-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06416-0