Abstract
Objective
To investigate the safety profile of percutaneous cryoablation of renal tumours < 7 cm, utilising data extracted from an international multicentre registry.
Materials and methods
A retrospective review of all immediate and delayed complications from a multicentre database was performed and was categorised according to the Clavien-Dindo classification. Statistical analysis was performed for both overall complications (all Clavien-Dindo) and major complications (Clavien-Dindo 3 to 5). The following criteria were identified as potential predictive factors for complications: centre number, modality of image guidance, tumour size (≤ 4 cm vs. > 4 cm), number of tumours treated in the same session (1 vs. > 1) and tumour histology.
Results
A total of 713 renal tumours underwent ablation in 647 individual sessions. In 596 of the cases, one tumour was treated; in the remaining 51 cases, several tumours were treated per session. Mean lesion size was 2.8 cm. Fifty-four complications (Clavien-Dindo 1 to 5) occurred as a result of the 647 procedures, corresponding to an overall complication rate of 8.3%. The most frequent complication was bleeding (3.2%), with 9 cases (1.4%) requiring subsequent treatment. The rate of major complication was 3.4%. The only statistically significant prognostic factor for a major complication was a tumour size > 4 cm.
Conclusion
Percutaneous renal cryoablation is associated with a low rate of complications. Tumours measuring more than 4 cm are associated with a higher risk of major complications.
Key Points
• Percutaneous kidney cryoablation has a low rate of complications.
• Bleeding is the most frequent complication.
• A tumour size superior to 4 cm is a predictive factor of major complication.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous kidney ablation is gaining popularity in the treatment of early-stage renal cancer, with mid-term oncological outcomes challenging those of surgery [1,2,3]. Among the various available modalities, cryoablation has gained wide acceptance with respect to renal tumour ablation [4]. The modality offers specific advantages over radiofrequency ablation (RFA), such as real-time monitoring of the ablation zone (thanks to the visualisation of the iceball), large volume of treatment (thanks to the simultaneous activation of several applicators) and urothelium preservation, which are particularly well adapted to manage complex renal tumours [5, 6]. The safety profile of cryoablation is also excellent, even in the setting of early experience of the operator where the expected significant complication rates are roughly 8% in the literature, with bleeding reported as the most frequent adverse event [7,8,9].
EuRECA (European Registry for Renal Cryoablation) is a European multicentre registry, which aims to document and collect short-, mid- and long-term oncological outcomes of both laparoscopic and percutaneous cryoablation procedures [10]. Prior to the introduction of a prospective database in 2016, four participating centres individually collected their retrospective data on all kidney tumours treated with percutaneous cryoablation from 2007 to 2013 (depending on the centre) to July 2016. The purpose of this study is to establish the rate and type of complications following percutaneous cryoablation of kidney tumours documented in the retrospective data collection.
Material and methods
This is a multicentre retrospective study. All patients gave informed consent for the procedure. Institutional review board was waived due to the retrospective design of the present study.
Cryoablation procedures
Across all four centres, the indication for percutaneous cryoablation was decided upon after a multidisciplinary meeting. In most cases, cryoablation was offered as an alternative to patients deemed unfit for surgery, or in the setting of a specific clinical scenario (chronic renal failure, single kidney, genetic disease). After patient consent, all procedures were performed under general anaesthesia by interventional radiologists (centres 1, 2, 3, 4) and a urologist trained in image-guided interventional techniques (centre 2), utilising argon-based cryoablation devices and cryo-probes (BTG-Galil). Depending on the centre, imaging modalities included computed tomography (CT), cone-beam CT (CBCT) or magnetic resonance imaging (MRI) guidance. Due to its limitation to monitor the positioning of multiple probes in the kidney and the poor visualisation of the whole iceball, no patients were treated with stand-alone ultrasound guidance. The number of probes utilised was determined by the treating physician in order to cover the entire lesion and maintain a safety margin of 5 mm with the iceball [11]. As per literature and manufacturer recommendation, cryoablation was performed with a dual-freeze protocol across all centres [12, 13]. All procedures were performed on an inpatient basis with a minimum hospital stay of at least one-night post-procedure.
Retrospective database
Each centre retrospectively recorded their data and outcomes into the database, which contained the following 13 variables: gender, age, single kidney, size of the tumour(s), tumour histology, history of previous renal cancer with description of treatment modality, number of tumours treated in one session, image guidance modality, use of hydro- or CO2 dissection, perioperative complications (up to 24 h after treatment), post-operative complications (without limitations in time), primary technical success and oncological status at last available follow-up. Although some of the data from this retrospective database have been previously published in the context of a single centre experience, this is the first encompassing a multicentre analysis [7, 14]. Data from all four institutions was then gathered by a referring physician from centre 2 and additional statistical analysis was performed by centre 1.
Data collection and analysis
Immediate and delayed complications were extracted from the database and classified according to the Clavien-Dindo classification [15]. Variables that were not available universally for all centres were excluded from statistical analysis. Hence, the following criteria were available from all four institutions and analysed as predictive factors for complications: centre number, modality of image guidance, size of tumour (≤ 4 cm vs. >4 cm, i.e. T1a vs. T1b), number of tumours treated in the same session (1 vs. > 1) and tumour histology. Statistical analysis was performed for both overall complications (Clavien-Dindo 1 to 5) and major complications (Clavien-Dindo 3 to 5). Descriptive statistics and statistical analysis were computed using SAS software version 9.4. Statistical significance was set with a p < 0.05.
Results
Tumours and procedures
A total of 713 renal tumours were ablated in 647 sessions. The number of treated tumours per intervention were one tumour only in 596 procedures (92.1%), two tumours in 39 procedures (6%), three in 9 procedures (1.4%) and four in 3 procedures (0.5%). The mean tumour size was 2.8 cm (range 0.8–6.7). There were 609 tumours (84%) which measured 4 cm or less, and 104 tumours (16%) measuring more than 4 cm. Histopathology included 486 renal cell carcinomas (RCC), with clear cell being the most frequent subtype (53%). A definite subtype was not available for 140 of the 486 biopsy-proven RCC tumours (28.8%). A certain diagnosis of benignity was found in 74 tumours (10.4%). Histology was not available for 18.4% of the 713 tumours. Details of histopathological results are presented in Table 1. Per-procedural modality of image guidance was found to be CT for 507 procedures (78%), cone-beam CT for 80 procedures (12.5%) and MRI-guidance for 60 procedures (9.5%). Repartition of the centres and modality of image guidance per centre are reported in Table 2.
Complications
Overall complications
A total of 54 complications (graded Clavien-Dindo 1 to 5) occurred during the 647 procedures, which correspond to an overall complication rate of 8.3%. Tumours measuring 4 cm or less had an overall complication rate of 7.3%, while tumours exhibiting a size superior to 4 cm had a rate of 9.8% (no statistically significant difference between the two groups was identified; p > 0.05).
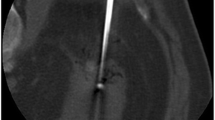
Overall, the most frequent complication was bleeding with 21 cases (3.2%). Of these, a total of 9 cases (1.4%) required subsequent treatment (transfusion in 4 cases, ureteral stenting in 3 cases and embolisation in 2 cases). Among all other complications, pneumothorax was the most frequent and occurred in 15 cases (2.2%), with 9 cases requiring chest tube insertion. There was a single case of colonic fistula formation (Fig. 1), and three injuries of the pyelo-ureteral junction requiring ureteral stenting. Regarding overall complications, univariate analysis did not reveal a statistically significant predictive factor for complication among the five tested variables. Detailed statistics for overall complications are presented in Table 3.
Colonic fistula following percutaneous cryoablation of a kidney RCC. a Per-procedure axial CT scan shows that the iceball encompasses part of the colon (arrow) despite extensive hydro-dissection (black asterisks) and carbodissection (white asterisk). b 3-week follow-up coronal T2-weighted MRI demonstrates a fistula (arrow) between the colon (black asterisk) and the cryoscar (white asterisk). The fistulous track heeled with antibiotic medications and did not require surgery (Clavien-Dindo 2)
Major complications
Twenty-two complications (3.4%) graded Clavien-Dindo 3 or more occurred during the 647 procedures, including 5 complications graded 4 or more (0.8%), with 2 post-operative deaths (0.3%). The two deaths were caused by a massive lung aspiration in one case and massive right-sided myocardial infarction in the other case, both in the recovery room immediately after the procedure. Details of major complications are presented in Table 4. For major complications, univariate analysis revealed a significant higher risk of complications for tumours measuring more than 4 cm (p < 0.05). Detailed statistics for major complications are presented in Table 5.
Discussion
Results from this retrospective multicentre database analysis confirmed the excellent safety profile of percutaneous cryoablation when treating tumours measuring less than 7 cm. The rate of major complication (Clavien-Dindo 3 or more) in this study was less than 5%, which is on par with and in some cases better than other reported outcomes in the literature. In 2014, Schmit et al reported a major complication rate (Clavien-Dindo grade 3 or more) of 7.5% in 398 cryoablation procedures [16]. The same year, Georgiades et al published a major complication rate of 6% (with a different grading system for complications) in their experience of treating 134 biopsy-proven RCC cases [11]. More recently, Breen et al reported a major complication rate (Clavien-Dindo 3 or more) of 4.9% over 473 procedures [17]. Similar to other reports, the most frequent complication in the present study was post-procedural bleeding in 3.2% of the tumours [11, 18]. However, the rate of bleeding requiring therapy was extremely low, with a transfusion rate of only 0.6% and an embolisation rate of merely 0.3%. These results are slightly more favourable than the ones presented by Kakarala et al, in which the rate of bleeding, bleeding requiring transfusion and bleeding necessitating endovascular embolisation were 3.5%, 1.5% and 0.8%, respectively (in 246 patients) [19]. The incidence of bleeding found in the present study remains higher than after RFA treatments [18, 20]. However, as already suggested in the literature, the theory of a significant risk of haemorrhage following cryoablation compared with radiofrequency ablation is probably unjustified [19]. The present study demonstrates tumour size as a factor, independent of major complications, but not of overall complications. This finding is in accordance with most publications, which report a correlation between increased tumour size and higher risk of complications [18, 19]. The rate of pneumothorax observed in the present study was rather high compared with other publications. Even though the location of the tumour was not recorded as a variable in this database, one can assume that pneumothorax might be more likely when treating upper-pole tumours. All cases of pneumothoraxes occurred in the CT guidance group, which suggest that modalities offering sagittal or oblique imaging (such as MRI and CBCT) may offer a safer approach for steep sagittal trajectories [21, 22]. Increased availability to multi-slice CT with dedicated interventional software will certainly reduce the risk of pleural transgression. The rate of pyelo-ureteral injury was low, a major difference with RFA, where pyelo-ureteral injury is one of the most frequent complications [18, 20]. Visualisation of the limits of the iceball with cryoablation is a key advantage when treating tumours located in close proximity to the pyelo-ureteral junction. Of note, unintentional freezing of the ureter does still carry a risk of secondary stricture formation [23]; surgical approach or additional protection with pyelo-perfusion and/or hydro-dissection should therefore always be considered for tumours abutting a ureter [24, 25].
The results from the EuRECA database do bring additional insight on specific points. First of all, the rate of major and, in fact, overall complications did not differ between the different centres and was not influenced by the modality of image guidance, illustrating the good reproducibility of the technique. We believe that the systematic use of general anaesthesia and cross-sectional imaging ensue confidence to the treating physician of optimum safety and can potentially explain these results. Recent recommendations of the CIRSE society include general anaesthesia and cross-sectional imaging (CT or MRI) as best clinical practice, as it allows optimum treatment precision [26]. Hence, there was only a single case of bowel fistulation and two pyelo-ureteral junction injuries in the present cohort. Additionally, histology does not appear to influence the risk of complication. This is consistent with reports from the literature; for example, malignancy was not a predictive factor for complication in the paper from Azevedo et al; it was only a predictive factor on univariate analysis (but not on multivariate analysis) in the study of Kakarala et al [19, 27]. The subtype of RCC did also not influence the rate of complications in our experience, which contradicts a recent publication from Haddad et al, in which the rate of complications was less for papillary tumour subtypes compared with the more common clear cell subtype [28]. Furthermore, we found that multiple treatments in the same session (on the same kidney) were not associated with an increased risk of complication, confirming the findings by Azevedo et al in their series of 60 patients [27]. This suggests the potential benefit of cryoablation in the treatment of patients suffering from multiple synchronous renal tumours, such as those with Von Hippel Lindau disease [29].
The present study has several major limitations, which may limit its significance. Because of the late retrospective data acquisition, many potentially relevant criteria, such as tumour location, number of probes used, procedural time and duration of hospital stay, were not consistently available and hence not analysed. Moreover, some data were not available in all centres and were therefore excluded from analysis, in order to keep data as consistent and homogeneous as possible. Finally, it is possible that the rate of complications was underestimated in our study because of the retrospective collection of the data. We believe that, on the whole, this would have impacted the rate of minor complications, which are more likely to be have been under-recorded. However, the rate of delayed complications with hospital readmission in other institutions might also have been overlooked and can potentially explain the relative low rate of major complications in this study compared with other publications.
In conclusion, analysis of this retrospective database confirms the excellent safety profile of percutaneous cryoablation, with a rate of major complications less than 5%. Bleeding is the most frequent complication, but the rate of haemorrhage requiring transfusion and/or subsequent intervention remains extremely low. These encouraging results will hopefully be confirmed by the current prospective database, which will limit the bias inherent to the present study.
Abbreviations
- CBCT:
-
Cone-beam CT
- CT:
-
Computed tomography
- EuRECA:
-
European Registry for Renal Cryoablation
- MRI:
-
Magnetic resonance imaging
- RCC:
-
Renal cell carcinomas
- RFA:
-
Radiofrequency ablation
References
Uhlig J, Strauss A, Rücker G et al (2018) Partial nephrectomy versus ablative techniques for small renal masses: a systematic review and network meta-analysis. Eur Radiol. https://doi.org/10.1007/s00330-018-5660-3
Thompson RH, Atwell T, Schmit G et al (2015) Comparison of partial nephrectomy and percutaneous ablation for cT1 renal masses. Eur Urol 67(2):252–259. https://doi.org/10.1016/j.eururo.2014.07.021
Rivero JR, De La Cerda J 3rd, Wang H et al (2018) Partial nephrectomy versus thermal ablation for clinical stage T1 renal masses: systematic review and meta-analysis of more than 3,900 patients. J Vasc Interv Radiol 29(1):18–29. https://doi.org/10.1016/j.jvir.2017.08.013
Ismail M, Nielsen TK, Lagerveld B et al (2018) Renal cryoablation: multidisciplinary, collaborative and perspective approach. Cryobiology 83:90–94. https://doi.org/10.1016/j.cryobiol.2018.06.002
Patel N, King AJ, Breen DJ (2016) Percutaneous image-guided cryoablation of small renal masses. Abdom Radiol (NY) 41(4):754–766. https://doi.org/10.1007/s00261-016-0682-2
Buy X, Lang H, Garnon J, Gangi A (2011) Percutaneous ablation of renal tumors: radiofrequency ablation or cryoablation? Journal de Radiologie 92(9):774–788. https://doi.org/10.1016/j.jradio.2011.07.016
Buy X, Lang H, Garnon J, Sauleau E, Roy C, Gangi A (2013) Percutaneous renal cryoablation: prospective experience treating 120 consecutive tumors. AJR Am J Roentgenol 201(6):1353–1361. https://doi.org/10.2214/AJR.13.11084
Schmit GD, Atwell TD, Callstrom MR et al (2010) Percutaneous cryoablation of renal masses >or=3 cm: efficacy and safety in treatment of 108 patients. J Endourol 24(8):1255–1262. https://doi.org/10.1089/end.2009.0328
Georgiades CS, Rodriguez R (2014) Efficacy and safety of percutaneous cryoablation for stage 1A/B renal cell carcinoma: results of a prospective, single-arm, 5-year study. Cardiovasc Intervent Radiol 37(6):1494–1499. https://doi.org/10.1007/s00270-013-0831-8
Nielsen TK, Lagerveld BW, Keeley F et al (2017) Oncological outcomes and complication rates after laparoscopic-assisted cryoablation: a European Registry for Renal Cryoablation (EuRECA) multi-institutional study. BJU Int 119(3):390–395. https://doi.org/10.1111/bju.13615
Georgiades C, Rodriguez R, Azene E et al (2013) Determination of the nonlethal margin inside the visible “ice-ball” during percutaneous cryoablation of renal tissue. Cardiovasc Intervent Radiol 36(3):783–790. https://doi.org/10.1007/s00270-012-0470-5
Gage AA, Baust J (1998) Mechanisms of tissue injury in cryosurgery. Cryobiology 37(3):171–186
Klossner DP, Robilotto AT, Clarke DM et al (2007) Cryosurgical technique: assessment of the fundamental variables using human prostate cancer model systems. Cryobiology 55(3):189–199
Breen DJ, Bryant TJ, Abbas A et al (2013) Percutaneous cryoablation of renal tumours: outcomes from 171 tumours in 147 patients. BJU Int 112(6):758–765. https://doi.org/10.1111/bju.12122
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Schmit GD, Schenck LA, Thompson RH et al (2014) Predicting renal cryoablation complications: new risk score based on tumor size and location and patient history. Radiology 272(3):903–910. https://doi.org/10.1148/radiol.14132548
Breen DJ, King AJ, Patel N, Lockyer R, Hayes M (2018) Image-guided cryoablation for sporadic renal cell carcinoma: three- and 5-year outcomes in 220 patients with biopsy-proven renal cell carcinoma. Radiology 7:180249. https://doi.org/10.1148/radiol.2018180249
Atwell TD, Carter RE, Schmit GD et al (2012) Complications following 573 percutaneous renal radiofrequency and cryoablation procedures. J Vasc Interv Radiol 23(1):48–54. https://doi.org/10.1016/j.jvir.2011.09.008
Kakarala B, Frangakis CE, Rodriguez R, Georgiades CS (2016) Hemorrhagic complications of percutaneous cryoablation for renal tumors: results from a 7-year prospective study. Cardiovasc Intervent Radiol 39(11):1604–1610. https://doi.org/10.1007/s00270-016-1419-x
Wah TM, Irving HC, Gregory W, Cartledge J, Joyce AD, Selby PJ (2014) Radiofrequency ablation (RFA) of renal cell carcinoma (RCC): experience in 200 tumours. BJU Int 113(3):416–428. https://doi.org/10.1111/bju.12349
Braak SJ, van Melick HH, Onaca MG, van Heesewijk JP, van Strijen MJ (2012) 3D cone-beam CT guidance, a novel technique in renal biopsy--results in 41 patients with suspected renal masses. Eur Radiol 22(11):2547–2552. https://doi.org/10.1007/s00330-012-2498-y
Koch G, Garnon J, Tsoumakidou G et al (2018) Adrenal biopsy under wide-bore MR imaging guidance. J Vasc Interv Radiol 29(2):285–290. https://doi.org/10.1016/j.jvir.2017.04.023
Bagley DH, Terrill R, Javadpour N, Beazley RM (1976) Cryosurgery of the ureter in dogs. Invest Urol 14(3):241–245
West B, Keheila M, Smith JC et al (2018) Efficacy of antegrade and retrograde warm saline pyeloperfusion during renal cryoablation for ureteral preservation. Turk J Urol 44(2):142–147. https://doi.org/10.5152/tud.2017.44380
Mauri G, Nicosia L, Varano GM et al (2017) Tips and tricks for a safe and effective image-guided percutaneous renal tumour ablation. Insights Imaging 8(3):357–363. https://doi.org/10.1007/s13244-017-0555-4
Krokidis ME, Orsi F, Katsanos K, Helmberger T, Adam A (2017) CIRSE guidelines on percutaneous ablation of small renal cell carcinoma. Cardiovasc Intervent Radiol 40(2):177–191. https://doi.org/10.1007/s00270-016-1531-y
Azevedo AAP, Rahal A Junior, Falsarella PM et al (2018) Image-guided percutaneous renal cryoablation: five years experience, results and follow-up. Eur J Radiol 100:14–22. https://doi.org/10.1016/j.ejrad.2018.01.001
Haddad MM, Schmit GD, Kurup AN et al (2018) Percutaneous cryoablation of solitary, sporadic renal cell carcinoma: outcome analysis based on clear-cell versus papillary subtypes. J Vasc Interv Radiol 29(8):1122–1126. https://doi.org/10.1016/j.jvir.2018.02.029
Yang B, Autorino R, Remer EM et al (2013) Probe ablation as salvage therapy for renal tumors in von Hippel-Lindau patients: the Cleveland Clinic experience with 3 years follow-up. Urol Oncol 31(5):686–692. https://doi.org/10.1016/j.urolonc.2011.05.008
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Julien Garnon—University Hospital of Strasbourg.
Conflict of interest
Dr. Garnon is a proctor for BTG Galil and received fees for oral presentation for Medtronic and Canon. Dr. Van Strijen, Lagerweld and Breen are proctors for BTG Galil. All other authors have no conflict of interest.
Statistics and biometry
Dr. Rousseau has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was not required because of the retrospective design of the study.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in:
• Buy X, Lang H, Garnon J, Sauleau E, Roy C, Gangi A. Percutaneous renal cryoablation: prospective experience treating 120 consecutive tumors. AJR Am J Roentgenol. 2013 Dec;201(6):1353–61. https://doi.org/10.2214/AJR.13.11084.
• Breen DJ, Bryant TJ, Abbas A, Shepherd B, McGill N, Anderson JA, Lockyer RC,Hayes MC, George SL. Percutaneous cryoablation of renal tumours: outcomes from 171 tumours in 147 patients. BJU Int. 2013 Oct;112(6):758–65. https://doi.org/10.1111/bju.12122.
Methodology
• retrospective
• observational
• multicentre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garnon, J., Van Strijen, M.J., Nielsen, T.K. et al. Safety of percutaneous renal cryoablation: an international multicentre experience from the EuRECA retrospective percutaneous database. Eur Radiol 29, 6293–6299 (2019). https://doi.org/10.1007/s00330-019-06191-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06191-y