Abstract
Purpose
Despite being accepted as a mainstay of treatment for hepatocellular carcinoma (HCC), technical aspects of transarterial chemoembolization (TACE) continue to vary by reporting author, leading to heterogeneity in the literature and making meaningful comparisons between treatments difficult. The goal of this survey was to report international chemoembolization practices for the treatment of HCC in an effort to understand current treatment strategies as a first step towards technique standardization.
Materials and methods
An anonymous 18-question online survey, evaluating technical aspects of their TACE practice, was distributed via email to practicing members of the five largest interventional radiology societies in Chinese and English. A total of 1160 responses were obtained from 62 countries. Responses were categorized according to region of practice and analyzed using Fisher’s exact test and chi-square test with Bonferroni correction as needed.
Results
There were significant statistical differences between regions for nearly all questions. Doxorubicin was more commonly used among respondents from North America, Europe, and South Korea than Japan and China (p = 0.0001). For single and multiple HCCs, drug-eluting bead TACE was most popular in North America and Europe (p = 0.0001), while conventional TACE was most popular in Japan, Korea, and China (p = 0.0001). CT was the most commonly used modality for follow-up among all respondents, although MR was used more commonly in North America and in academic centers (p = 0.0001).
Conclusion
This survey provides comprehensive information on and confirms the heterogeneous nature of current practice patterns in regard to TA(C)E for HCC.
Key Points
• There is a lack of information regarding current practice patterns in the area of technical considerations when performing transarterial chemoembolization.
• Type of transarterial chemoembolization utilized to treat hepatocellular carcinoma varies widely across geographical area.
• Chemotherapeutic agents and embolic agents used to perform transarterial chemoembolization for the treatment of hepatocellular carcinoma vary widely across geographical areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Locoregional therapies (LRTs) are an accepted, and frequently applied, treatment for hepatocellular carcinoma (HCC) patients. While many LRTs have been created and found efficacious, transarterial chemoembolization (TACE) is perhaps the most studied and therefore most accepted. TACE is included in HCC treatment algorithms by virtually every major liver/HCC society including the Barcelona Clinic Liver Cancer (BCLC), American Association for the Study of Liver Disease (AASLD), and European Association for the Study of the Liver (EASL) [1,2,3]. While the body of literature is extensive in regard to TACE in the treatment of HCC, the technical aspects of the procedure itself frequently vary in even basic areas such as the choice of chemotherapy or if chemotherapy is used at all.
The two groundbreaking clinical trials, which firmly established the efficacy of TACE for the treatment of HCC by showing improved overall survival as compared to best clinical care, serve to demonstrate these technical differences [4, 5]. These two studies differed in chemotherapeutic agents used, use of antibiotics, embolization endpoint, and time between treatments. This heterogeneity has persisted in the TACE literature without clear evidence to guide practitioners in the most basic aspects of the procedure.
The heterogeneity of the literature is furthered by the fact that TACE is commonly used as an umbrella term used to describe several fundamentally different procedures, including conventional TACE (cTACE), drug-eluting bead TACE (DEB-TACE), and transarterial embolization (TAE). While all three procedures involve the selective catheterization of the artery(ies) feeding the tumor, conventional TACE then involves the delivery of chemotherapeutic agent(s) mixed with an ethiodol oil, which serves to prevent immediate washout of the chemotherapy. cTACE then follows the delivery of ethiodol oil/chemotherapeutic agent(s) with particle embolization to stop blood flow as well as increase chemotherapeutic dwell time [6]. DEB-TACE differs in that chemotherapy is loaded onto beads, which then slowly release it after arterial delivery, thus combining the embolization and chemotherapeutic steps [7]. Finally, TAE is very similar to TACE, and except in TAE, no ethiodol oil or chemotherapy is used; the lesion is treated with simple particle embolization [8].
The differences in fundamental technical aspects of the procedure make comparisons across clinical trials difficult. Furthermore, the variation is a symptom of lack of evidence as to the most efficacious ways to perform the procedure. This area is in dire need of well-done randomized controlled trials to answer these fundamental questions; however, before those can be designed, it is important to understand the current state of practice. Unfortunately, there is a paucity of this type of data in the literature, which is currently limited to a single country or interventional society [9,10,11].
Therefore, this paper aims to determine the current global practice patterns of TA(C)E through a survey which was distributed to the largest interventional radiology societies around the world.
Materials and methods
A questionnaire was developed by two interventional radiologists with expertise in oncology. It was then distributed to other interventional radiologists with expertise in oncology for review and comment. Finally, a concensus18-question online survey, administered through Survey Monkey and Qualtrics, was distributed by email to members of the Cardiovascular and Interventional Radiology Society of Europe (CIRSE), the Chinese Society of Interventional Radiology (CSIR), the Japanese Society of Interventional Radiology (JSIR), the Korean Society of Interventional Radiology (KSIR), and the Society of Interventional Radiology (SIR). The survey is presented in the Appendix and was distributed in English and Chinese. Where appropriate, the responses were categorized and analyzed using Fisher’s exact test and chi-square test with Bonferroni correction as needed. Responses were categorized according to region of practice. In total, nine regions were established, including China, Japan, Korea, North America, South America, Europe, Middle East/Africa, South Asia, and Oceania and analyzed. A p value of < 0.05 was considered statistically significant.
Results
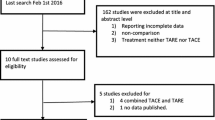
An estimated total of 15,704 surveys were distributed and 1160 responses were obtained from 62 countries, leading to a response rate of 7.4%. Fifty-eight responses were excluded because less than 90% of answers were completed. Responses by society can be found in Fig. 1 and the responses by geographical location can be found in Fig. 2. Of the completed responses, 566 (51.4%) were members of SIR, 331 (30.0%) of CIRSE, 120 (10.9%) of CSIR, 58 (5.3%) of JSIR, and 27 (2.4%) KSIR.
Response numbers by society. The number of responses is presented in parentheses following the society. CIRSE Cardiovascular and Interventional Radiology Society of Europe, CSIR Chinese Society of Interventional Radiology, JSIR Japanese Society of Interventional Radiology, KSIR Korean Society of Interventional Radiology, SIR Society of Interventional Radiology
Respondents most commonly worked at an academic practice (397/1074, 37.0%), followed by a government hospital (300/1074, 27.9%), community hospital (175/1074, 16.3%), and a secondary/tertiary referral center (202/1074, 18.8%).
There was a significant statistical difference among the cytotoxic agent(s) used, dosing of agent(s), type of procedure for single and multiple HCCs, the DEB type, amount of ethiodized oil, drug mixing method, procedural endpoint, type of embolic agent, use of additives and antibiotics, length of clinical follow-up, choice of imaging follow-up, and choice of tumor response between the regions (Table 1).
Evaluation of preferred materials and techniques
Respondents differed significantly, by region, in their preferred procedure (DEB-TACE, cTACE, etc.) for single and multiple HCCs (p < 0.0001). For single HCCs, compared with other groups, DEB-TACE was most popular in North America (318/527, 60.3%) and Europe (145/238, 60.9%) (p < 0.01), while cTACE was most popular in Japan (53/63, 84.1%), Korea (22/35, 62.8%), and China (61/131, 46.5%) (p < 0.01). For multiple HCCs, DEB-TACE remained most common in North America (243/523, 46.4%) and Europe (108/236, 45.7%) (p < 0.01), and cTACE remained most common in Japan (37/61, 60.7%), Korea (21/34, 61.7%), and China (59/111, 53.4%) (p < 0.01). TAE was the procedure of choice for 2.9% (32/1094) of practitioners.
The responses for choice of cytotoxic agent can be found in Table 2; there was a statistically significant difference in chemotherapeutic agent preferred between regions (p < 0.0001). Doxorubicin was the most popular cytotoxic agent overall (779/1084, 71.7%) and more commonly used by respondents from North America, Europe, and Korea (p < 0.01). Pirarubicin was the most commonly used cytotoxic agent in China (27/128, 21.1%) and Epirubicin in Japan (43/59, 72.9%). Use of a combination of chemotherapeutic agents is infrequent with only 2.1% (23/1084) using triple-drug therapy and 2.8% (30/1084) using double-drug therapy.
The responses for choice of cytotoxic dose determination can be found in Table 3; there was a statistically significant difference in the dose determination method between regions (p < 0.0001). A fixed dose of cytotoxin per procedure was the most common response among all groups (588/1071, 54.9%). Most respondents in this group used between 50 and 100 mg of doxorubicin. Tumor size (256/1071, 23.9%), patient body surface area (56/1071, 5.2%), liver function (58/1071, 5.4%), and patient body weight (25/1071, 2.3%) were less commonly used to determine the dose. Asian countries favor basing dose on tumor size while North America and Europe favored a fixed dose, resulting in statistically significant difference among regions (p < 0.0001).
The targeted embolic endpoint varied significantly among geographical regions (p < 0.001). The most common response was the use of a combination of flow reduction in the feeding vessel(s), complete stasis in the feeding vessel(s), and oil uptake by the tumor (311/907, 34.3%). This was followed closely by complete stasis of the feeding vessel(s) (301/907, 33.2%).
Pre- and post-procedural practices
There was a statistically significant difference in the use of antibiotics between regions (p < 0.0001). Periprocedural antibiotics were statistically more commonly used by the members in North America (462/563, 82.1%), but not as commonly used in respondents from Europe (165/313, 52.7%), Japan (31/53, 58.5%), Korea (3/19, 15.8%), or China (16/112, 14.3%) (p < 0.01).
The typical clinical follow-up was between 2 weeks and 2 months in all groups (914/1088, 84.0%). Respondents were equally likely to follow up patients between 2 weeks and 1 month (412/1088, 37.9%) and between 1 and 2 months (502/1088, 46.1%). Very few respondents followed patients up at less than 2 weeks (84/1088, 7.7%) or at greater than 2 months (90/1088, 8.3%). CT was the most commonly used modality for follow-up among all respondents (698/1090, 64.0%), but MR was statistically used more by North American respondents compared with all other groups combined (p = 0.0001).
To determine the tumor response, modified Response Evaluation Criteria in Solid Tumors (mRECIST) (658/1038, 63.3%) and RECIST (239/1038, 23.0%) criteria were most commonly utilized. mRECIST was statistically used more frequently in North America and Europe than those in the Asian Interventional Societies (p = 0.0001), and RECIST was statistically used more frequently by the Asian countries than in North America and Europe (p = 0.0001).
Effect of preference of DEB-TACE or cTACE on responses
To determine the effect of a respondents’ preference for DEB-TACE or cTACE on the other survey responses, a separate analysis was performed. The results for this analysis can be found in Table 4. The cytotoxic agent of choice for both those preferring cTACE (141/308, 45.8%) and DEB-TACE (478/506, 94.5%) was doxorubicin. However, there was a statistically significant difference between the two groups (p < 0.0001) with those preferring DEB-TACE being more likely to choose doxorubicin. There was a statistically significant difference in the dose calculation based on respondents’ preference for DEB-TACE or cTACE (p < 0.0001), with those who preferred DEB-TACE being more likely to utilize a fixed-dose calculation method. Similarly, while CT was the most common choice for follow-up imaging in both cTACE (221/304, 72.7%) and DEB-TACE (299/503, 59.4%) respondents, those who preferred cTACE were more likely to follow up with CT than those who preferred DEB-TACE (p = 0.0007).
Discussion
HCC is the fifth most common cancer worldwide and the third most common cause of cancer mortality [12, 13]. While TA(C)E is considered a palliative treatment, it is frequently used and a part of virtually every societal treatment algorithm [1,2,3]. However, some of the basic technical aspects of the procedure change with provider. These technical differences make comparison of clinical trials difficult and speak to the lack of clear evidence to guide practitioners.
This study demonstrates that there are significant regional differences in the chemotherapeutic regimen, which is preferred by interventionalists. The preference of practitioners in China to use pirarubicin may be due to an in vitro study which demonstrated that pirarubicin ethiodol oil mixture was more stable and cytotoxic to HepG2 and Hu-H7 cells than doxorubicin ethiodol oil mixture [14]. However, several studies have failed to demonstrate clear superiority of one chemotherapeutic agent to another [15,16,17], while others have demonstrated better outcomes when using a three-drug regimen as compared to a single- or two-drug regimen [18, 19]. This study found the most commonly used chemotherapeutic regimen in North America and Europe was single-agent doxorubicin. This may relate to the fact that doxorubicin is loadable onto drug-eluting beads and therefore can be used for DEB-TACE [20, 21]. This theory seems to be supported by the fact that 94.5% of respondents who preferred DEB-TACE used doxorubicin as their cytotoxic agent of choice. This study found very few practitioners use triple- or double-drug therapy (2.1% and 2.8% respectively), despite the aforementioned studies suggesting triple-drug therapy may be superior [18, 19]. Again, this may be related to a preference of some regions for DEB-TACE, where only a single drug can be loaded, to cTACE.
This study found significant differences in preference of technique between regions with the majority of North American and European practitioners preferring DEB-TACE and the majority of Japanese and Korean interventionalists preferring cTACE, while TAE was the procedure of choice for very few clinicians across all regions. One possible explanation for the preference of DEB-TACE in North America is the fact that ethiodol oil and doxorubicin powder, both critical to cTACE, have been periodically unavailable in North America due to manufacturing concerns. Another explanation may be the lack of evidence to support one technique over the other. Further analyses also revealed that respondents’ preference for DEB-TACE or cTACE significantly affected their responses to many of the other technical factors associated with TA(C)E (Table 4). This underlies that technical choices are not only significantly affected by geographical location, but also by preference of technique.
Early pathologic analysis of explanted livers, which had previously undergone either TAE or cTACE, seemed to suggest an improved complete pathologic response in the cTACE patients [22,23,24]. Further argument for the use of chemotherapy was seen when the Llovet et al trial was published. This trial was designed to compare not only cTACE and TAE to best supportive care, but each other [4]. While the trial demonstrated superior 1- and 2-year survival rates in the cTACE arm as compared to that in the TAE arm, statistical significance was not reached, possibly because trial enrollment was stopped early due to the superiority of both intervention arms to supportive care. However, in a recent trial by Brown et al comparing DEB-TACE to TAE, while OS was longer in the DEB-TACE cohort as compared to that in the TAE cohort (20.8 vs 19.6 months), this was not found to be statistically significant [8]. This study has its own limitation as the technique of embolization in both groups was heavily directed towards aggressive embolization to complete stasis. Nonetheless, the data is conflicting over the need to subject patients to chemotherapeutic agents at all. After the introduction of drug-eluting beads and the subsequent development of DEB-TACE, comparisons between cTACE and DEB-TACE have also been made; while occasional studies have found the superiority of one treatment over the other, the majority of randomized controlled trials and meta-analyses have found equivalence of these techniques [7, 25,26,27,28,29,30]. A frequent argument for DEB-TACE over cTACE is the lower serum chemotherapeutic agent exposure; however, this has not consistently translated to fewer adverse events [7, 25,26,27,28,29,30]. One of the weaknesses of these studies is they most frequently compare single chemotherapeutic agent cTACE to DEB-TACE, given some studies have found that triple therapy is superior to single therapy; the cTACE response and survival levels may be suboptimal.
Another area with significant differences across regions was the dose of chemotherapeutic drug used. North Americans and Europeans favored a fixed dose, while interventionalists in Asia tended towards dosing based on tumor size. These differences may in part be due to the preference of North Americans and Europeans to use DEB-TACE where 50 mg of doxorubicin is loaded on each vial of beads, and typically, 1–2 vials are used, whereas those in Asia tended to prefer cTACE, where dose can be more easily adjusted. This theory seems to be supported by the fact that respondents who preferred DEB-TACE were statistically more likely to use a fixed-dose calculation than those who preferred cTACE. While studies clearly identifying a clinical benefit for higher dose of chemotherapeutic agent are missing, there is some evidence that dose can play an effect on adverse events. The PERCISION V study, which compared DEB-TACE to cTACE, used a body surface area dosing for the cTACE arm resulting in most patients receiving between 100 and 150 mg of doxorubicin, a higher dose than many other studies [7]. The study found a difference in adverse events between the two arms, which was primarily driven by nearly 20% of patients developing alopecia in the cTACE arm. Alopecia is a rarely reported side effect of cTACE in other studies, and this may explain why other studies have not shown a difference in adverse events between the two techniques [28, 29].
Three prior surveys have probed the practice patterns for TA(C)E therapy or follow-up [9,10,11]. All have been relatively small and limited to a single interventional society. Gaba surveyed 268 SIR members regarding TACE [9]. Bergellini et al presented responses from 78 Italian treatment centers regarding their use of LRTs for HCC [10]. Finally, Gaba et al queried 361 SIR members about their follow-up practices following LRTs for primary and secondary malignancies of the liver [11]. While all three surveys presented interesting data on practice trends from their collective populations, they were unable to compare these trends across regions and had much smaller sample sizes than this study.
This study has several limitations. While a relatively large number of responses were obtained, the majority were from two societies (CIRSE and SIR). Questionnaires are also known to be prone to response bias, which may affect their accuracy. While the questionnaire did probe the techniques of responding practitioners, its multiple-choice format may have missed some nuances. Furthermore, it did not probe the reasons behind interventionalists’ choices. Finally, this paper does not include information about practitioners’ practice regarding other LRTs such as radioembolization or thermal ablation nor does it investigate outcomes. Due to the desire to keep the survey short and to increase response rate and the desire to probe technical choices made during the TA(C)E procedure, these topics were not breached. Despite these flaws, this provides the most comprehensive to date analysis of TA(C)E treatment practices over diverse demographic areas. The survey demonstrates that there is significant heterogeneity across even basic technical aspects of the TA(C)E procedure.
In conclusion, practitioners across diverse demographic areas differ in the way they perform TA(C)E for patients with HCC. Furthermore, the practitioners’ preference for cTACE or DEB-TACE significantly effects other procedural choices. These differences lead to difficulty in comparing studies in this field and are driven by the lack of high-level data to guide treatment teams. Further, well-done randomized controlled trials are needed to help determine the most effective technical methods to perform TA(C)E.
Abbreviations
- AASLD:
-
American Association for the Study of Liver Disease
- BCLC:
-
Barcelona Clinic Liver Cancer
- CIRSE:
-
Cardiovascular and Interventional Radiology Society of Europe
- CSIR:
-
Chinese Society of Interventional Radiology
- cTACE:
-
Conventional transarterial chemoembolization
- DEB-TACE:
-
Drug-eluting bead transarterial chemoembolization
- EASL:
-
European Association for the Study of the Liver
- HCC:
-
Hepatocellular carcinoma
- JSIR:
-
Japanese Society of Interventional Radiology
- KSIR:
-
Korean Society of Interventional Radiology
- LRTs:
-
Locoregional therapies
- mRECIST:
-
modified Response Evaluation Criteria in Solid Tumors
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- SIR:
-
Society of Interventional Radiology
- TACE:
-
Transarterial chemoembolization
- TAE:
-
Transarterial embolization
References
Forner A, Gilabert M, Bruix J, Raoul JL (2014) Treatment of intermediate-stage hepatocellular carcinoma. Nat Rev Clin Oncol 11:525–535
Heimbach J, Kulik LM, Finn R et al (2017) AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 67:358–380 https://doi.org/10.1002/hep.29086
European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Llovet JM, Real MI, Montaña X et al (2002) Arterial embolization or chemoembolization versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomized controlled trial. Lancet 359:1734–1739
Lo CM, Ngan H, Tso WK et al (2002) Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35:1164–1171
Raoul JL, Heresbach D, Bretagne JF et al (1992) Chemoembolization of hepatocellular carcinomas. A study of the biodistribution and pharmacokinetics of doxorubicin. Cancer 70:585–590
Lammer J, Malagari K, Vogl T et al (2010) Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc Interv Radiol 33:41–52
Brown KT, Do RK, Gonen M et al (2016) Randomized trial of hepatic artery embolization for hepatocellular carcinoma using doxorubicin-eluting microspheres compared with embolization with microspheres alone. J Clin Oncol 34:2046–2053
Gaba RC (2012) Chemoembolization practice patterns and technical methods among interventional radiologists: results of an online survey. AJR Am J Roentgenol 198:692–699
Bargellini I, Florio F, Golfieri R, Grosso M, Lauretti DL, Cioni R (2014) Trends in utilization of transarterial treatments for hepatocellular carcinoma: results of a survey by the Italian Society of Interventional Radiology. Cardiovasc Intervent Radiol 37:438–444
Gaba RC, Baerlocher MO, Nikolic B, Venkatesan AM, Lewandowski RJ (2015) Clinical and imaging follow-up practices after transarterial therapy for primary and secondary hepatic malignancies: results of an online survey. Acad Radiol 22:1510–1515
El-Serag HB, Rudolph KL (2007) Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 132:2557–2576
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61(2):69–90
Favoulet P, Cercueil JP, Faure P et al (2001) Increased cytotoxicity and stability of Lipiodol-pirarubicin emulsion compared to classical doxorubicin-Lipiodol: potential advantage for chemoembolization of unresectable hepatocellular carcinoma. Anticancer Drugs 12:801–806
Marelli L, Sigliano R, Triantos C et al (2007) Transarterial therapy for hepatocellular carcinoma: which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc Intervent Radiol 30:6–25
Sahara S, Kawai N, Sato M et al (2012) Prospective evaluation of transcatheter arterial chemoembolization (TACE) with multiple anticancer drugs (epirubicin, cisplatin, mitomycin c, 5-fluorouracil) compared with TACE with epirubicin for treatment of hepatocellular carcinoma. Cardiovasc Intervent Radiol 35:1363–1371
Tawanda A, Chiba T, Ooka Y et al (2015) Transarterial chemoembolization with miriplatin plus epirubicin in patients with hepatocellular carcinoma. Anticancer Res 35:549–554
Liu B, Huang JW, Li Y et al (2015) Single-agent versus combination doxorubicin-based transarterial chemoembolization in the treatment of hepatocellular carcinoma: a single-blind, randomized, phase II trial. Oncology 89:23–30
Shi M, Lu LG, Fang WQ et al (2013) Roles played by chemolipodolization and embolization in chemoembolization for hepatocellular carcinoma: single-blind, randomized trial. J Natl Cancer Inst 105:59–68
Jordan O, Denys A, De Baere T, Boulens N, Doelker E (2010) Comparative study of chemoembolization loadable beads: in vitro drug release and physical properties of DC bead and hepasphere loaded with doxorubicin and irinotecan. J Vasc Interv Radiol 21:1084–1090
Lewis AL, Gonzalez MV, Lloyd AW et al (2006) DC bead: in vitro characterization of a drug-delivery device for transarterial chemoembolization. J Vasc Interv Radiol 17:335–342
Matsui O, Kadoya M, Yoshikawa J et al (1993) Small hepatocellular carcinoma: treatment with subsegmental transcatheter arterial embolization. Radiology 188:79–83
Matsuo N, Uchida H, Nishimine K et al (1993) Segmental transcatheter hepatic artery chemoembolization with iodized oil for hepatocellular carcinoma: antitumor effect and influence on normal tissue. J Vasc Interv Radiol 4:543–549
Nakamura H, Tanaka T, Hori S et al (1983) Transcatheter embolization of hepatocellular carcinoma: assessment of efficacy in cases of resection following embolization. Radiology 147:401–405
Gao S, Yang Z, Zheng Z et al (2013) Doxorubicin-eluting bead versus conventional TACE for unresectable hepatocellular carcinoma: a meta-analysis. Hepatogastroenterology 60:813–820
Facciorusso A, Di Maso M, Muscatiello N (2016) Drug-eluting beads versus conventional chemoembolization for the treatment of unresectable hepatocellular carcinoma: a meta-analysis. Dig Liver Dis 48:571–577
Zou JH, Zhang L, Ren ZG, Ye SL (2016) Efficacy and safety of cTACE versus DEB-TACE in patients with hepatocellular carcinoma: a meta-analysis. J Dig Dis 17(8):510–517
Golfieri R, Giampalma E, Renzulli M et al (2014) Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolization for hepatocellular carcinoma. Br J Cancer 111:255–264
Sacco R, Bargellini I, Bertini M et al (2011) Conventional versus doxorubicin-eluting bead transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol 22:1545–1552
Van Malenstein H, Maleux G, Vandecaveye V et al (2011) A randomized phase II study of drug-eluting beads versus transarterial chemoembolization for unresectable hepatocellular carcinoma. Onkologie 34:368–376
Acknowledgments
The authors would like to acknowledge Dr. Yasuaki Arai, Dr. Gaojun Teng, Dr. Young Soo Do, Dr. Hyun-Ki Yoon, Dr. Daniel Brown, and Dr. Charles Ray for their feedback and comments in the preparation of the survey.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Shamar Young.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Lei Zhang kindly provided statistical advice for this manuscript.
Informed consent
Informed consent was not required because this was a survey of practicing Interventional Radiologists.
Ethical approval
Institutional Review Board approval was not required because this was a survey of practicing Interventional Radiologists.
Methodology
• Cross-sectional survey study
• Multicenter study
Appendix 1
Appendix 1
Survey Text:
Transcatheter Arterial (Chemo)embolization (TA(C)E) Survey
This short (one-page) survey should not take more than two minutes of your time. This survey was designed to obtain a general idea of the type of TA(C)E procedures that you typically perform. It is important to answer at least one answer per question, as follow up questions may drop down. Thank you very much for your participation.
-
1.
What country do you practice in?
-
a.
(Answer field blank)
-
a.
-
2.
What type of practice are you in?
-
a.
Academic
-
b.
Private practice – community hospital
-
c.
Private practice – secondary or tertiary referral center
-
d.
Government hospital
-
e.
Other (please specify)
-
i.
(Answer field blank)
-
a.
-
3.
For TA(C)E procedures at your institution, what is the common cytotoxic agent used for the treatment of hepatocellular carcinoma (HCC)?
-
a.
Doxorubicin
-
b.
Epirubicin
-
c.
Cisplatin
-
d.
Mitoxantrone
-
e.
Mitomycin C
-
f.
SMANCS
-
g.
Pirarubicin
-
h.
Nemorubicin
-
i.
Miriplatin
-
j.
Idarubicin
-
k.
Irinotecan
-
l.
Anthracycline (e.g. Doxorubicin, Epirubicin) and Mitomycin C
-
m.
Anthracycline and Cisplatin
-
n.
Anthracycline, Mitomycin C, and Cisplatin
None of the above (bland transarterial embolization (TAE))
Other (please specify)
-
a.
-
4.
For TA(C)E procedures at your institution, how is the dose of cytotoxin agent determined?
-
a.
Fixed dose (e.g. 50mg Doxorubicin for every person). Please list dose below.
-
b.
Body weight (e.g. 1mg Doxorubicin for every kg). Please list amount per kg below.
-
c.
Body surface area (e.g. 50mg/meter2). Please list amount per meter2 below.
-
d.
Tumor size
-
e.
Liver function (AFP, etc.)
-
f.
Other (please specify)
-
a.
-
5.
What is your typical procedure for a single HCC?
-
a.
Ethiodized oil TACE (cTACE)
-
b.
Drug-Eluting Beads TACE
-
c.
Bland Transarterial Embolization (TAE)
-
d.
Technique depends on the extension and location of the tumor
-
e.
Other (please specify)
-
a.
-
6.
What amount of ethiodized oil is typically used?
-
a.
Not applicable
-
b.
0-5ml
-
c.
5-7.5ml
-
d.
7.5-10ml
-
e.
>10ml
-
f.
Other
-
a.
-
7.
What is the ratio (volume:volume) of ethiodized oil to cytotoxic agent used in your procedure?
-
8.
How is the ethiodized oil mixed with the cytotoxic agent?
-
a.
Not applicable
-
b.
Pump between stop cock (to and fro) – ethiodized oil tube injected into cytotoxin tube
-
c.
Pump between stop cock (to and fro) – cytotoxin tube injected into ethiodized oil
-
d.
Pump between stop cock (to and fro) – no preference in order mixed
-
e.
Mixed with a machine
-
f.
No specific method
-
g.
Other (please specify)
-
a.
-
9.
What type of drug-eluting beads do you use?
-
a.
Not applicable
-
b.
Tandem
-
c.
Pearl
-
d.
QuadraSpheres
-
e.
LC/DC
-
f.
Other (please specify)
-
a.
-
10.
What size of drug-eluting beads do you use (please specify)?
-
a.
(Answer field blank)
-
a.
-
11.
What is your procedural endpoint?
-
a.
Administration of fixed dose
-
b.
Flow reduction in the feeding vessel(s)
-
c.
Complete stasis in the feeding vessel(s)
-
d.
Oil uptake by tumor
-
e.
A combination of B and D or C and D
-
f.
Other (please specify)
-
a.
-
12.
Are embolic agents used in your procedure?
-
a.
No
-
b.
Yes – Gelatin (specify product below)
-
c.
Yes – Non-spherical polyvinyl alcohol (specify product below)
-
d.
Yes – Spherical (specify product below)
-
a.
-
13.
What is your typical procedure for multiple HCCs?
-
a.
Ethiodized oil TACE (cTACE)
-
b.
Drug-Eluting Beads TACE
-
c.
Bland Transarterial Embolization (TAE)
-
d.
Technique depends on the extension and location of the tumor
-
e.
Other (please specify)
-
a.
-
14.
Are additives used with the primary cytotoxic agent (water-soluble contrast, solubility agents, etc.)?
-
a.
No
-
b.
Yes (please specify)
-
a.
-
15.
Do you routinely use antibiotics with TA(C)E procedures?
-
a.
No
-
b.
Yes, before
-
c.
Yes, during
-
d.
Yes, after
-
e.
A combination of the factors listed above
-
a.
-
16.
When is your typical clinical follow up for TA(C)E procedures?
-
a.
Less than 2 weeks
-
b.
2 weeks – 1 month
-
c.
>1 month - <2 months
-
d.
>2 months
-
a.
-
17.
What type of imaging follow up do you perform?
-
a.
CT (specify interval below)
-
b.
MR (specify interval below)
-
c.
Other (please specify below)
-
a.
-
18.
What criteria do you use to determine tumor response?
-
a.
European Association of the Study of Liver (EASL)
-
b.
World Health Organization (WHO)
-
c.
Response Evaluation Criteria in Solid Tumors (RECIST)
-
d.
Modified Response Evaluation Criteria in Solid Tumors (mRECIST)
-
e.
Other (please specify)
-
a.
Rights and permissions
About this article
Cite this article
Young, S., Craig, P. & Golzarian, J. Current trends in the treatment of hepatocellular carcinoma with transarterial embolization: a cross-sectional survey of techniques. Eur Radiol 29, 3287–3295 (2019). https://doi.org/10.1007/s00330-018-5782-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5782-7