Abstract
The 2017 Core of the computed tomography (CT)/magnetic resonance imaging (MRI) Liver Imaging Reporting and Data System (LI-RADS) provides clear definitions and concise explanations of the CT/MRI diagnostic algorithm. Nevertheless, there remain some practical and controversial issues that radiologists should be aware of when using the system. This article discusses pitfalls and problems which may be encountered when the version 2017 diagnostic algorithm is used for CT and MRI. The pitfalls include challenges in applying major features and assigning the LR-M category, as well as categorisation discrepancy between CT and MRI. The problems include imprecision of category codes, application of ancillary features, and regional practice variations in hepatocellular carcinoma (HCC) diagnosis. Potential solutions are presented along with these pitfalls and problems.
Key Points
• Although the diagnostic algorithm provides clear and detailed explanations, major feature evaluation can be subject to pitfalls and differentiation of HCC and non-HCC malignancy remains challenging.
• Ancillary features are optional and equally weighted. However, features such as hepatobiliary phase hypointensity and restricted diffusion have greater impact on HCC diagnosis than other ancillary features and may merit greater emphasis or weighting.
• LI-RADS was initially developed from a Western paradigm, which may limit its applicability in the East due to regional practice variations. In Eastern Asia, high sensitivity is prioritised over near-perfect specificity for HCC diagnosis in order to detect tumours at early stages.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Liver Imaging Reporting and Data System (LI-RADS) aims to standardise the terminology, interpretation and reporting of liver imaging in patients at risk for hepatocellular carcinoma (HCC) [1]. LI-RADS has been iteratively refined; an example is the recent clarification on target population [2]. However, practical limitations and controversies still remain in the version 2017. The article discusses pitfalls and problems of the CT/MRI diagnostic algorithm, together with potential solutions.
Pitfalls
Pitfall set 1: characterisation of major features
Arterial phase hyperenhancement (APHE)
LI-RADS defines APHE by comparing an observation with surrounding liver parenchyma, not by comparing it with unenhanced images or using subtraction imaging. The definition requires that at least part of the observation be brighter than the liver in the arterial phase; observations that are hypointense precontrast and isointense in the arterial phase are not considered to have APHE, despite enhancing more than liver. Question remains why such observations, despite the hypervascular nature, do not qualify for APHE in LI-RADS. Similarly, subtraction imaging, when combined with conventional arterial phase images, can help evaluate APHE on MRI and increase the sensitivity of HCC diagnosis [3, 4]. The use of subtraction images is especially helpful in observations with intrinsic T1 hyperintensity. We encourage LI-RADS to standardise the use of subtractions in future versions. Contrast-enhanced ultrasound may also be performed to evaluate hypervascularity in these observations.
In cases of arterial phase mistiming, APHE can manifest after the nominal late arterial phase [5]. Greater awareness of this possibility among LI-RADS users may help. Additionally, since multi-arterial phase imaging can improve the consistency with which APHE is demonstrated [6], future versions of LI-RADS could give guidance to using this emerging technique.
Finally, some large circumscribed HCCs may show iso- or hypoenhancement on the arterial phase except for intratumoural arteries [7] (Fig. 1). The presence of intratumoural arteries, being a “part” of observation, should qualify as APHE. The current definition does not make this as clear as it should. Clarification is needed.
A 48-year-old man with chronic hepatitis B and a large hepatocellular carcinoma (HCC) containing intratumoural arteries. a Axial T1-weighted three-dimensional (3D) gradient-echo unenhanced MR image reveals an 82-mm hypointense mass in the left lateral hepatic section. b The mass has scattered areas of vague hyperintensity relative to the surrounding liver in the arterial phase after gadoxetate disodium administration. Note also intratumoural arteries (arrowheads). c The arterial phase hyperenhancement (APHE) is subtle and could be missed on the source image but is obvious on the (arterial phase – pre) subtraction image. d The mass shows “washout” in the portal venous phase (PVP)
“Washout”
“Washout” is defined as non-peripheral, visually assessed temporal reduction in the degree of enhancement relative to composite liver tissue, resulting in hypoenhancement in the portal venous or delayed phases. There is debate over whether iso- or hypoenhancement in the arterial phase (i.e. no APHE) followed by hypoenhancement in the portal venous or delayed phases should be regarded as “washout”, as indicated in the current definition, because this may result in overcategorisation of some benign lesions, including dysplastic nodules, as LR-4. Another opinion is that hypoenhancement in the portal venous or delayed phases relative to the adjacent liver is an essential component, and temporal reduction in the degree of enhancement throughout dynamic phases may instead be discarded from the definition. Research is needed to examine the validity of the current definition of “washout” and inform its refinement.
Using gadoxetate disodium, LI-RADS requires that “washout” be assessed only in the portal venous phase (PVP). This is problematic because LI-RADS does not clearly define the end of the PVP with this agent. Defining the end by a fixed time after injection (2 min) when the transitional phase (TP) begins is simplistic. Research is needed to better understand and define the PVP and TP using gadoxetate disodium.
Hypointensity in the TP or hepatobiliary phase (HBP) is considered an ancillary feature as it may result from background parenchymal enhancement rather than lesional de-enhancement, not being specific enough for HCC [8]. However, studies have suggested that in combination with non-rim APHE, HBP hypointensity is highly sensitive and also specific for HCC [9, 10]. As TP hypointensity itself is more specific for HCC than HBP hypointensity alone [9], the combination of non-rim APHE and TP hypointensity might be even more specific for HCC. Further research is needed to determine if TP or HBP hypointensity can be elevated to major features in the context of small lesions with non-rim APHE, especially after excluding haemangioma and intrahepatic cholangiocarcinoma (ICC).
Enhancing “capsule”
Enhancing “capsule” is a smooth enhancing rim around an observation on the portal venous, delayed or transitional phases which is clearly thicker or more conspicuous than the background liver parenchymal fibrosis. This definition is problematic on gadoxetate-enhanced MRI because the enhancing “capsule” can be masked by background parenchymal enhancement. The phenomenon reduces the sensitivity of gadoxetate-enhanced MRI for detecting enhancing “capsule” compared to extracellular agent (ECA)-enhanced MRI or CT. However, the analogous feature on gadoxetate-enhanced MRI—a smooth hypointense rim in the HBP (i.e. non-enhancing “capsule”)—can improve the sensitivity of HCC diagnosis without reducing specificity [11]. We encourage research to examine the diagnostic performance of HBP hypointense rim relative to that of enhancing “capsule” on gadoxetate-enhanced MRI.
Recognising that LI-RADS is constrained by a desire for congruency with Organ Procurement and Transplantation Network (OPTN) policy, which incorporates enhancing “capsule” in its classification system, there is a concern whether enhancing “capsule” should be retained as a major feature. The main reason for retaining enhancing “capsule” as a major feature is that it contributes to the diagnosis of HCC when “washout” is not discernible, especially in 1- to 2-cm-sized observations with APHE [12]. Other considerations suggest its removal, however [13]. For example, the imaging feature may not represent a true tumour capsule and is less specific for HCC than pathological capsule [14]. Moreover, the feature is relatively infrequent and usually accompanies other major features that permit the diagnosis of HCC anyway [15]. The validity of this latter point needs to be confirmed, however, as it was made prior to the recognition that enhancing “capsule” may create the perception of “washout” [16]. Research is needed to compare the diagnostic performance characteristics of LI-RADS categorisation using versus not using enhancing “capsule” as a major feature.
Threshold growth
Threshold growth (TG), currently a major feature in LI-RADS and OPTN system, represents tumour growth itself, which favours the diagnosis of malignancy over benignity, but per se is not diagnostic of HCC [17]. Moreover, TG cannot be applied in the diagnosis of HCC when previous CT or MRI examinations are unavailable. Finally, TG affects LI-RADS categorisation in only a small proportion of observations [18]. Therefore, contention exists as to whether TG can act as a major criterion for HCC diagnosis. More evidence is needed to validate TG as a major feature.
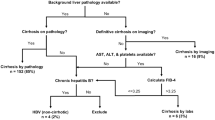
Pitfall set 2: categorisation of LR-M
LR-M is a category for probably or definitely malignant observations which are not specific for HCC. As stated in LI-RADS, the differential diagnosis of LR-M includes ICC, hepato-cholangiocarcinoma (H-ChC), metastasis, and HCC with atypical imaging features. Thus, users should be aware that in the context of high HCC prevalence, LR-M does not exclude HCC [14, 19, 20]. Interestingly, HCCs which are categorised LR-M may imply worse outcomes than HCCs meeting LR-5 criteria [21] (Fig. 2), suggesting that LR-M features may have prognostic value even for lesions proven to be HCC at biopsy or surgery.
HCC with the LR-M features in a 60-year-old man with chronic hepatitis B. a The axial T1-weighted 3D gradient-echo unenhanced MR image shows a 24-mm hypointense nodule in the hepatic segment VII. b The nodule exhibits a targetoid appearance and rim APHE after gadoxetate disodium administration. c On the PVP, the nodule shows “washout” and an enhancing “capsule.” d On the hepatobiliary phase (HBP), a subtle targetoid appearance is also demonstrated with slightly more pronounced hypointensity in the periphery of the nodule compared to the centre (arrowheads). As demonstrated in this case, LR-M does not exclude HCC
Meanwhile, it is inevitable that some non-HCC malignancies will be incorrectly categorised LR-5 or LR-4 [14, 20, 22, 23] (Fig. 3). In a retrospective analysis, more than half of 61 H-ChCs satisfied the LR-5 criteria for observations 2 cm or larger when LR-M criteria were not considered [24]. The false categorisation was reduced to 6.6% after consideration of ancillary features of version 2014 favouring non-HCC malignancy, suggesting that LR-M features can help differentiate H-ChC from HCC. Nevertheless, since H-ChCs contain HCC components, perfect differentiation from “pure” HCCs is not possible with current imaging technology. In cirrhotic patients, moreover, some small ICCs show non-rim APHE and non-peripheral “washout” and are indistinguishable from HCC based on major features alone. Unfortunately, these small ICCs may lack LR-M features in the HBP or on diffusion-weighted imaging [23]. Further study is needed to identify new imaging features that help discriminate non-HCC malignancy from HCC in order to reduce the rate of miscategorisation and subsequent overtreatment in deceased donor transplantation candidates.
Intrahepatic cholangiocarcinoma (ICC) satisfying the LR-5 criteria in a 77-year-old woman with chronic hepatitis B. a The axial CT image shows a 29-mm nodule in the anterior surface of the hepatic segment III with APHE. The nodule shows partial “washout” on the (b) portal venous and (c) delayed phases. d The axial T1-weighted 3D gradient-echo MR image shows a hypointense nodule before contrast enhancement. The nodule depicts (e) APHE and (f) partial PVP “washout” after gadoxetate disodium administration. g On HBP, the nodule is hypointense to the surrounding liver. As illustrated in this case, some ICCs meet LR-5 criteria
Additionally, an extrahepatic primary malignancy can develop hypervascular metastasis to the liver in patients with cirrhosis or chronic hepatitis B. Such metastases may also be inappropriately categorised LR-4 or LR-5 (Fig. 4). Further research is needed to determine the frequency with which hypervascular metastases occur in the LI-RADS diagnostic population as well as the frequency with which these lesions result in diagnostic errors using current LI-RADS criteria.
Metastasis from thymoma satisfying the LR-5 criteria in a 55-year-old man with chronic hepatitis B. a The axial T1-weighted 3D gradient-echo unenhanced MR image shows an 86-mm hypointense mass in the right hemiliver. After gadoterate meglumine administration, the mass depicts hypervascularity on the (b) arterial phase image and (c) subtraction image. d On the PVP, the nodule shows “washout” and an enhancing “capsule”. As illustrated by this case, hypervascular metastasis from an extrahepatic malignancy can satisfy LR-5 criteria, although this is believed to occur only rarely
A final limitation is that LR-M category rarely includes benign entities [14]. For example, sclerosing haemangiomas may manifest rim APHE and be categorised LR-M. The categorisation of benign lesions as LR-M can be problematic in terms of overtreatment when these lesions undergo surgical resection without preoperative biopsy confirmation. The ability to differentiate probably malignant from definitely malignant LR-M observations is an unmet need in these cases.
Pitfall set 3: CT-MRI categorisation discrepancy
For simplicity, LI-RADS uses the same basic diagnostic algorithm for CT and MRI, but studies have demonstrated that the LI-RADS categorisation can differ between CT and MRI in 36-77% of observations [25,26,27]. For example, the frequency of enhancing “capsule” among HCCs was higher in ECA-enhanced MRI than CT (44% vs 17%), leading to a significant increase in the number of 1- to 2-cm-sized LR-5 observations in MRI [12]. In another study, discordance rates between CT and ECA-enhanced MRI were moderate to high for APHE (57%), “washout” (21%) and enhancing “capsule” (43%); in the discordant cases, these features were demonstrated only in ECA-enhanced MRI, leading to higher category assignments [26]. Discordance also occurs between CT and gadoxetate-enhanced MRI with rates of 7% for APHE, 22% for “washout”, and 33% for enhancing “capsule” [22]; in this study, APHE and enhancing “capsule” were discerned more frequently on gadoxetate-enhanced MRI, while “washout” was seen more frequently on CT.
Similarly, many ancillary features are applicable only to MRI and others only to gadoxetate-enhanced MRI. For example, features of mild to moderate T2 hyperintensity, restricted diffusion, and HBP hypointensity lead to higher category assignment on gadoxetate-enhanced MRI than CT which is incapable of assessing these features [28]. Similarly, early HCC is categorised LR-4 more frequently on gadoxetate-enhanced MRI than on CT because of HBP hypointensity [29], and more frequently on ECA-enhanced MRI than on CT because of intratumoural fat [25]. Meanwhile, marked T2 hyperintensity permits appropriate downgrading to LR-1 or LR-2 of haemangiomas with atypical enhancement profiles [25] (Fig. 5). Conversely, MRI detects benign but potentially confusing vascular pseudolesions more often than CT [25]. Most of these are categorised LR-2 or LR-3 by MRI but, being imperceptible, uncategorised by CT.
Ancillary feature rendering a benign diagnosis in a 41-year-old man with chronic hepatitis B and non-alcoholic steatohepatitis. The axial T1-weighted 3D gradient-echo gadoxetate-enhanced MR images reveal a 20-mm nodule in the hepatic segment III with atypically persistent hyperenhancement throughout the (a) arterial and (b) portal venous phases. c On HBP, the nodule is hypointense to the liver parenchyma. d The signal intensity of the nodule on the heavily T2-weighted image (echo time, 150 ms) is markedly brighter than non-iron-overloaded spleen and close to the brightness of the cerebrospinal fluid (arrowhead), suggesting a diagnosis of haemangioma
Some of these discrepancies may be unavoidable, reflecting inherent differences in the modalities’ capabilities. Therefore, some authors suggest combined usage of both modalities under certain circumstances [22, 27]. Further consensus on the choice of modality may be necessary in LI-RADS. In addition, it may be useful to assess the value of ancillary features—which are present mainly on MRI [30]—and if they are really useful.
An additional concern is that contrast administration protocol is less standardised in CT than in MRI. In patients with liver cirrhosis, contrast injection rate and contrast administration dose need to be adjusted in order to yield optimal liver enhancement on CT [31]. Thus, covering the aspect in the LI-RADS technical recommendations may help decrease the discrepancy between major feature evaluation by CT and MRI.
Problems to be solved
Problem 1: imprecision of category codes
The actual probabilities of HCC associated with LR-3 and LR-4 are not yet well known. Studies suggested that 69-90% of LR-4 observations are HCC [20, 32], but this has not been verified extensively. Interestingly, observations categorised LR-4 based on major features have a higher HCC probability than those upgraded from LR-3 by HBP hypointensity [32], suggesting that categorisation “pathway” may affect HCC probability. A different study found that 69% of version 2013.1 LR-3 observations discovered initially on surveillance US are HCC [19], but these nodules would be categorised LR-4 using version 2017. Another study showed that 40% of version 2014 LR-3 observations undetected by surveillance US are HCC [20].
The LR-3, LR-4, and LR-5 categories are heterogeneous, each assignable by several different combinations of features. Contributing to the heterogeneity is that categories may be adjusted by ancillary features and tie-breaking rules. Thus, each category comprises a large and diverse set of observations, each with its own unique categorisation “pathway.” LI-RADS facilitates the diagnosis of high risk borderline lesions, especially with gadoxetate-enhanced MRI [29]. However, the clinical significance of these lesions, mostly categorised LR-3 or LR-4, is still uncertain. Large multicentre studies are needed to define the HCC probability and/or the natural history of common categorisation pathways, especially for LR-3 and LR-4. Such data may eventually permit the assignment of granular probabilities of HCC, which would facilitate application of individualised management strategies and decrease overdiagnosis and overtreatment of borderline lesions.
A related challenge is that reader variability in the characterisation of major and ancillary features can introduce variability in assigning LI-RADS categories. As expected, agreement for assigning LR-2, LR-3 and LR-4 categories is lower than that for assigning LR-1 and LR-5 categories [33]. Meanwhile, assigning LR-M category does not seem to be critically discrepant among readers [30]. A few studies have shown that the inter-reader agreement can be improved in LI-RADS. As diameter measurement tends to be consistent among readers [12, 26, 33, 34], some investigators have proposed a modified algorithm whereby size is the initial node in the decision tree [34].
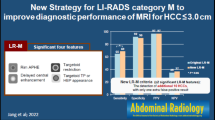
Problem 2: application of ancillary features
LI-RADS currently includes many ancillary features, although the quality of evidence supporting these features tends to be low. Some ancillary features are rarely used and do not differ in frequency between HCC and non-HCC malignancy [14]. To reduce the perceived complexity of LI-RADS, ancillary features have been made optional. However, this solution is suboptimal as some ancillary features do play important roles in diagnosis. For example, HBP hypointensity and restricted diffusion are strong indicators of malignancy [22]. We anticipate that HBP hypointensity and restricted diffusion could be elevated to major features with appropriate combination of other features, based on emerging data [9, 10]. Hierarchical weighting and/or removal of less contributory features may also be beneficial.
Problem 3: regional practice variations
Risk factors and incidence of HCC vary geographically, resulting in different diagnostic and management strategies across the world. For example, whereas hepatitis C virus infection is the most important risk factor in Europe, Japan and North America, hepatitis B virus infection is a major risk factor in the Asia-Pacific region [35,36,37]. This is important because many patients with HCC due to chronic hepatitis B have no or well-compensated cirrhosis and can be offered curative resection if the cancer is detected in early stages. Thus, in Eastern Asia, where the incidence of HCC is highest [36], early detection of HCC is critical, and high sensitivity for HCC diagnosis is valued even at the expense of an “acceptable” decrease in specificity [13]. By comparison, transplantation is the only curative treatment for patients with HCC developing in the cirrhotic liver. Since deceased donor liver transplantation is the main source of organ procurement in the West, high specificity for HCC diagnosis is needed to ensure appropriate organ allocation [38]. For this reason, LR-5 category has been designed in LI-RADS to provide a near-perfect specificity for HCC. However, such high specificity may not be as necessary in living donor transplant candidates in Asian countries [39].
Ideally, future versions will consider regional differences in HCC diagnosis and management. For regionally tailored LI-RADS, one proposal is to divide LR-M into LR-4M (probably malignant but not specific for HCC) and LR-5M (definitely malignant but not specific for HCC) [40]. Particularly in Eastern Asia, the most important preoperative goal is to identify definitely malignant lesions (i.e. LR-5 or LR-5M), which also applies to other regional practices in terms of overdiagnosis and overtreatment.
Conclusions
Despite the clear definitions and detailed explanations, there remain some practical and controversial issues regarding the CT/MRI diagnostic algorithm of LI-RADS. Assessment of major features may be subject to several pitfalls, which indicates the need for continuing refinement of the current system. Refinements are also needed to better discriminate non-HCC malignancy from HCC and to manage the category discrepancy between CT and MRI. Suggestion on granular HCC probability according to categorisation pathway may enable individually tailored management. Some ancillary features merit greater emphasis or weighting. We anticipate that LI-RADS will evolve to integrate regional practice variations and enhance the global influence.
Abbreviations
- APHE:
-
Arterial phase hyperenhancement
- ECA:
-
Extracellular contrast agent
- HBP:
-
Hepatobiliary phase
- HCC:
-
Hepatocellular carcinoma
- H-ChC:
-
Hepato-cholangiocarcinoma
- ICC:
-
Intrahepatic cholangiocarcinoma
- LI-RADS:
-
Liver Imaging Reporting and Data System
- PVP:
-
Portal venous phase
- TG:
-
Treshold growth
- TP:
-
Transitional phase
References
American College of Radiology (2017) Liver imaging reporting and data system version 2017. Available via https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/CT-MRI-LI-RADS-v2017. Accessed 6 Jun 2018
Tang A, Hallouch O, Chernyak V, Kamaya A, Sirlin CB (2018) Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol (NY) 43:13–25
Choi SH, Kim SY, Lee SS et al (2017) Subtraction images of gadoxetic acid–enhanced MRI: effect on the diagnostic performance for focal hepatic lesions in patients at risk for hepatocellular carcinoma. AJR Am J Roentgenol 209:584–591
An C, Park MS, Kim D et al (2013) Added value of subtraction imaging in detecting arterial enhancement in small (<3 cm) hepatic nodules on dynamic contrast-enhanced MRI in patients at high risk of hepatocellular carcinoma. Eur Radiol 23:924–930
Jo PC, Jang HJ, Burns PN, Burak KW, Kim TK, Wilson SR (2017) Integration of contrast-enhanced US into a multimodality approach to imaging of nodules in a cirrhotic liver: how I do it. Radiology 282:317–331
Ikram NS, Yee J, Weinstein S et al (2017) Multiple arterial phase MRI of arterial hypervascular hepatic lesions: improved arterial phase capture and lesion enhancement. Abdom Radiol (NY) 42:870–876
Lee JH, Lee JM, Kim SJ et al (2012) Enhancement patterns of hepatocellular carcinomas on multiphasic multidetector row CT: comparison with pathological differentiation. Br J Radiol 85:e573–e583
Joo I, Lee JM, Lee DH, Jeon JH, Han JK, Choi BI (2015) Noninvasive diagnosis of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: can hypointensity on the hepatobiliary phase be used as an alternative to washout? Eur Radiol 25:2859–2868
Choi SH, Byun JH, Lim YS et al (2016) Diagnostic criteria for hepatocellular carcinoma ≤3 cm with hepatocyte-specific contrast-enhanced magnetic resonance imaging. J Hepatol 64:1099–1107
Renzulli M, Biselli M, Brocchi S et al (2018) New hallmark of hepatocellular carcinoma, early hepatocellular carcinoma and high-grade dysplastic nodules on Gd-EOB-DTPA MRI in patients with cirrhosis: a new diagnostic algorithm. Gut. https://doi.org/10.1136/gutjnl-2017-315384
An C, Rhee H, Han K et al (2017) Added value of smooth hypointense rim in the hepatobiliary phase of gadoxetic acid-enhanced MRI in identifying tumour capsule and diagnosing hepatocellular carcinoma. Eur Radiol 27:2610–2618
Ehman EC, Behr SC, Umetsu SE et al (2016) Rate of observation and inter-observer agreement for LI-RADS major features at CT and MRI in 184 pathology proven hepatocellular carcinomas. Abdom Radiol (NY) 41:963–969
Korean Society of Abdominal Radiology (2017) Diagnosis of hepatocellular carcinoma with gadoxetic acid-enhanced MRI: 2016 consensus recommendations of the Korean Society of Abdominal Radiology. Korean J Radiol 18:427–443
Fraum TJ, Tsai R, Rohe E et al (2018) Differentiation of hepatocellular carcinoma from other hepatic malignancies in patients at risk: diagnostic performance of the Liver Imaging Reporting and Data System version 2014. Radiology 286:158–172
Rimola J, Forner A, Tremosini S et al (2012) Non-invasive diagnosis of hepatocellular carcinoma ≤2 cm in cirrhosis. Diagnostic accuracy assessing fat, capsule and signal intensity at dynamic MRI. J Hepatol 56:1317–1323
Sofue K, Sirlin CB, Allen BC, Nelson RC, Berg CL, Bashir MR (2016) How reader perception of capsule affects interpretation of washout in hypervascular liver nodules in patients at risk for hepatocellular carcinoma. J Magn Reson Imaging 43:1337–1345
Tang A, Bashir MR, Corwin MT et al (2018) Evidence supporting LI-RADS major features for CT- and MR imaging-based diagnosis of hepatocellular carcinoma: a systematic review. Radiology 286:29–48
Chernyak V, Kobi M, Flusberg M, Fruitman KC, Sirlin CB (2017) Effect of threshold growth as a major feature on LI-RADS categorization. Abdom Radiol (NY) 42:2089–2100
Darnell A, Forner A, Rimola J et al (2015) Liver Imaging Reporting and Data System with MR imaging: evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology 275:698–707
Kim YY, An C, Kim S, Kim MJ (2018) Diagnostic accuracy of prospective application of the Liver Imaging Reporting and Data System (LI-RADS) in gadoxetate-enhanced MRI. Eur Radiol 28:2038–2046
An C, Park S, Chung YE et al (2017) Curative resection of single primary hepatic malignancy: Liver Imaging Reporting and Data System category LR-M portends a worse prognosis. AJR Am J Roentgenol 209:576–583
Cha DI, Jang KM, Kim SH, Kang TW, Song KD (2017) Liver Imaging Reporting and Data System on CT and gadoxetic acid-enhanced MRI with diffusion-weighted imaging. Eur Radiol 27:4394–4405
Joo I, Lee JM, Lee SM, Lee JS, Park JY, Han JK (2016) Diagnostic accuracy of liver imaging reporting and data system (LI-RADS) v2014 for intrahepatic mass-forming cholangiocarcinomas in patients with chronic liver disease on gadoxetic acid-enhanced MRI. J Magn Reson Imaging 44:1330–1338
Potretzke TA, Tan BR, Doyle MB, Brunt EM, Heiken JP, Fowler KJ (2016) Imaging features of biphenotypic primary liver carcinoma (hepatocholangiocarcinoma) and the potential to mimic hepatocellular carcinoma: LI-RADS analysis of CT and MRI features in 61 cases. AJR Am J Roentgenol 207:25–31
Corwin MT, Fananapazir G, Jin M, Lamba R, Bashir MR (2016) Differences in Liver Imaging and Reporting Data System categorization between MRI and CT. AJR Am J Roentgenol 206:307–312
Zhang YD, Zhu FP, Xu X et al (2016) Liver Imaging Reporting and Data System: substantial discordance between CT and MR for imaging classification of hepatic nodules. Acad Radiol 23:344–352
Basha MAA, AlAzzazy MZ, Ahmed AF et al (2018) Does a combined CT and MRI protocol enhance the diagnostic efficacy of LI-RADS in the categorization of hepatic observations? A prospective comparative study. Eur Radiol 28:2592–2603
Joo I, Lee JM, Lee DH, Ahn SJ, Lee ES, Han JK (2017) Liver imaging reporting and data system v2014 categorization of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: comparison with multiphasic multidetector computed tomography. J Magn Reson Imaging 45:731–740
Kim BR, Lee JM, Lee DH et al (2017) Diagnostic performance of gadoxetic acid-enhanced liver MR imaging versus multidetector CT in the detection of dysplastic nodules and early hepatocellular carcinoma. Radiology 285:134–146
Fowler KJ, Tang A, Santillan C et al (2018) Interreader reliability of LI-RADS version 2014 algorithm and imaging features for diagnosis of hepatocellular carcinoma: a large international multireader study. Radiology 286:173–185
Eddy K, Costa AF (2017) Assessment of cirrhotic liver enhancement with multiphasic computed tomography using a faster injection rate, late arterial phase, and weight-based contrast dosing. Can Assoc Radiol J 68:371–378
Choi SH, Byun JH, Kim SY et al (2016) Liver Imaging Reporting and Data System v2014 with gadoxetate disodium-enhanced magnetic resonance imaging: validation of LI-RADS category 4 and 5 criteria. Investig Radiol 51:483–490
Davenport MS, Khalatbari S, Liu PS et al (2014) Repeatability of diagnostic features and scoring systems for hepatocellular carcinoma by using MR imaging. Radiology 272:132–142
Becker AS, Barth BK, Marquez PH et al (2017) Increased interreader agreement in diagnosis of hepatocellular carcinoma using an adapted LI-RADS algorithm. Eur J Radiol 86:33–40
European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Ferlay J SI, Ervik M, Dikshit R et al (2012) Cancer incidence and mortality worldwide: IARC CancerBase No. 11. International Agency for Research on Cancer. Available via http://globocan.iarc.fr. Accessed 6 Aug 2017.
Zhu RX, Seto WK, Lai CL, Yuen MF (2016) Epidemiology of hepatocellular carcinoma in the Asia-Pacific region. Gut Liver 10:332–339
Tang A, Fowler KJ, Chernyak V, Chapman WC, Sirlin CB (2018) LI-RADS and transplantation for hepatocellular carcinoma. Abdom Radiol (NY) 43:193–202
Chen CL, Kabiling CS, Concejero AM (2013) Why does living donor liver transplantation flourish in Asia? Nat Rev Gastroenterol Hepatol 10:746–751
Kim YY, An C, Kim MJ (2018) Letter to the editor. Abdom Radiol (NY) 43:237–238
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jin-Young Choi in Department of Radiology, Severance Hospital, Research Institute of Radiological Science, Yonsei University College of Medicine.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required because this review article does not include analysis of patient data.
Ethical approval
Institutional Review Board approval was not required because this review article does not include analysis of patient data.
Rights and permissions
About this article
Cite this article
Kim, YY., Choi, JY., Sirlin, C.B. et al. Pitfalls and problems to be solved in the diagnostic CT/MRI Liver Imaging Reporting and Data System (LI-RADS). Eur Radiol 29, 1124–1132 (2019). https://doi.org/10.1007/s00330-018-5641-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5641-6