Abstract
Objectives
To investigate patients’ perception of the radiology service when the radiologist communicates the findings to patients.
Methods
After routine MRI, patients in group 1 (n = 101) were given the opportunity to discuss the findings with the radiologist. Patients in group 2 (n = 101) left the radiology department without any personal communication. Subsequently, by means of a questionnaire designed by an expert psychologist, both groups were asked regarding their anxiety, emotional attachment to the institute and subjective assessment of competence.
Results
Overall 76 % of all patients were concerned about their imaging findings without significant difference between both groups (p = 0.179). Significantly more patients in group 1 (81%) versus group 2 (14%; p < 0.001) perceived the opportunity to discuss their imaging findings with a radiologist to be a characteristic of a good radiology consultation. A larger number of patients in group 1 experienced significantly higher bonding and only wanted in the future to be examined in the department with communication (p = 0.001) (93%/75%). Significantly more patients in group 1 regarded the radiology department they attended as being more competent (mean score 4.72/4.09, p < 0.001).
Conclusion
Direct communication of imaging findings from radiologists to patients after an MRI examination leads to increased confidence in the radiology service and higher bonding between the patient and radiologist. Radiologists who refrain from direct communication have a lower bonding to patients and are assessed to have lower competence from the patient’s point of view.
Key Points
• Communication between radiologists and patients leads to an increased bonding affinity.
• Direct communication leads to increased patient confidence in the radiology service.
• Patients perceived discussion with a radiologist of high value.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As a result of the increasing impact and availability of imaging technologies, there has been a significant increase in the number of radiological examinations and interventions performed for the screening, diagnosis and follow-up of diseases [1, 2]. The rising workload in radiology departments and the increasing reliance on imaging in clinical decision-making testify to the importance of the radiologist in clinical care and research [3]. However, over the years, radiologists have become increasingly isolated from direct patient contact. Likewise, this separation makes radiologists less aware of the potential stress and anxiety among patients and their relatives when they attend an imaging examination [4].
Within the radiology community, there is differing opinion as to whether the radiologist should be only an “imager” limited to the review, technical provision and reporting of imaging studies; or whether the radiologist should be a more patient-oriented physician, undertaking active dialogue with patients regarding their disease management [5]. According to global radiology practices, 80–90% of radiologists do not directly talk to or engage with patients before or after imaging examinations [6, 7]. Typically, issues or queries related to imaging studies are dealt with by a radiographer/technician. In an increasing drive towards quality and value-centred healthcare, it is important for radiologists to be perceived as important healthcare contributors, otherwise there is significant risk that our profession will become progressively commoditised. For this reason, the degree to which patients are aware of the substantial and decision-making role of the radiologist can help to affirm the importance of our profession amongst other sub-specialties within the healthcare system.
There is an ongoing discussion as to whether radiologists should rethink their clinical management paradigms. In addition, the term “radiologist 3.0” has emerged in the last few years encouraging a shift from the “pure imager” to the patient-oriented specialist, which encompasses the radiologist delivering meaningful and actionable reports to the referring physician, as well as the communication of radiology reports to the patients [8].
To the best of our knowledge, no study has investigated the bonding effects of direct communication between radiologists and patients, and how the patients’ bonding behaviour and anxiety can be improved through such interventions. Hence, the aim of this study was to compare patients’ stress level, bonding behaviour and perception of the radiology service depending on whether or not the radiologist reviews the findings after an imaging examination with the patient.
Material and methods
This prospective study was conducted from January 2017 to June 2017 in accordance with the Declaration of Helsinki. Written informed consent was obtained from patients, who were evaluated anonymously.
Consecutive patients who attended a magnetic resonance imaging (MRI) examination were asked to take part in the study. All patients were outpatients and independently mobile. Patients who consented to participate to the study were randomised into two groups: group 1, patients who after MRI discussed their imaging results with the radiologist; and group 2, patients who did not get the opportunity to discuss their imaging with a radiologist after MRI. The selection of the patients, whether they were attributed to group 1 or 2, was carried out under strict controlled randomisation.
All MRI studies were conducted at the same clinic under the same conditions and at the same location for both groups 1 and 2. MRI studies were carried out on a 1.5-T MRI Aera system (Siemens Healthcare, Germany). Imaging was performed by a consistent team of eight technicians. The technicians were never told in advance on which day the study would take place to minimise any potential bias effects on the patients.
Group 1: patients who met and discussed their imaging findings with a radiologist immediately after MRI (Fig. 1)
The patients in group 1 were asked to review the imaging findings with the radiologist immediately after completing routine MRI. In that discussion, the radiologist communicated the imaging findings directly to the patients and allowed them to ask questions. The duration of the interaction was recorded using a stopwatch. Following the review, the patient was given an anonymous written questionnaire to complete and return within 2 weeks.
Group 2: patients not getting the opportunity to discuss their imaging findings with a radiologist after MRI (Fig. 2)
Patients in group 2 underwent routine MRI without the opportunity to discuss their imaging with a radiologist after the examination. This is a typical scenario practised across most radiology departments worldwide. After the MRI, the patients were also asked to complete and return the identical anonymous written questionnaire within 2 weeks as for group 1.
Questionnaire
The questions in the questionnaire were developed with a team of experienced clinical psychologists (RH, 25 years of professional experience in clinical and scientific work in psychology) in accordance with international clinical guidelines and standardised questionnaires [9].
Stress level
A modified and standardised anxiety questionnaire was applied to determine how much subjective stress or anxiety patients felt during and after their MRI examinations [9]. After the questionnaires from groups 1 and 2 were evaluated, the stress and anxiety levels of patients were categorised into five categories: “ I don’t think about it”, “no stress”, “very little stress”, “medium stress” and “massive stress”.
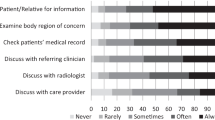
Subjective importance of direct interaction with a radiologist
The patients in both groups were asked to rate the importance of having direct interaction or an interview with a radiologist after the MRI examination by choosing one of two possible statements: (1) “A final discussion with the radiologist after an MRI examination is an important part of the medical service”. (2) “A final discussion with the radiologist is unimportant with regards to the medical service”.
Perception of competence
Patients from both groups were asked to rate how their perception of the competence of the radiology department may be interpreted using a 5-point scale, with score 1 indicating lowest competence and score 5 the highest competence. It should be noted that in group 2, without a doctor’s consultation, the answer "I cannot judge it" was given more frequently (N = 24).
Bond between patient and radiology department
We investigated the extent to which the patients were emotionally attached to the radiology department after the examination. The patients were asked to choose one of three possible responses: (1) “Based on my experience, I would no longer like to consult this radiology department and will inform my GP/referring physician”. (2) “I only want to visit this institution for future radiological investigations and will inform my GP/referring physician”. (3) “I do not mind which radiology department my GP/referring physician sends me to.”
Concerns about radiology findings
Patients in both groups were asked about the extent of their concern and anxiety about the radiology findings and the final report. Patients were able to choose one of the following answers: (1) indifferent to the result; (2) interested in the result, but not stressed; (3) yes, I worry about radiology results; and (4) I worry excessively about radiology results. There were no standardised questionnaires at this point; thus, these questions were independently formulated by our psychologist team.
Radiologist’s interaction with patients
The conversations with the patients were always conducted by the same radiologist (AG) after routine MRI for group 1. This radiologist has 17 years’ experience in general radiology and has received advanced training in active listening and communication according to Rogers and Schulz von Thun, and has obtained various dedicated certifications in communication training in the past 3 years [10, 11]. In the case of group 2 patients, the same radiologist was present but not visible to the patient. In case of need, the radiologist was available for the patient at any time, but this was never actively induced by the patient.
Statistical analysis
The answers given were analysed with SPSS version 20 (Chicago, Ill, USA). For quantitative variables, number of observations, minima, maxima, mean and standard deviations are reported. For categorical variables, the absolute (n) and relative (%) frequency is shown. Patient groups were compared with a Fisher’s exact test for categorical variables and with an exact Mann–Whitney U test for quantitative variables (except for age that was compared with an unpaired t test).
Results
Overall, 123 patients were able to discuss their MRI experience and findings with the radiologist after their examination (group 1). Of these, 22 patients were excluded from analysis because they did not return their questionnaire. Overall, we finally investigated 101 patients in group 1 (48 women; mean age 52.3 years, range 17–85).
A total of 175 patients were not given the opportunity to discuss their MRI experience and findings with the radiologist (group 2). Of these, 74 patients were subsequently excluded from further analysis because they did not return their questionnaire. We finally evaluated 101 patients in group 2 (50 women; mean age 53.1 years, range 16–86). There were no statistical differences between the two groups with regards to age (p = 0.730) and gender (p = 0.888) (Table 1).
Patients in both groups underwent a wide range of different MRI examinations (Table 2).
The results related to the completed questionnaires are presented below.
Stress level
During the MRI studies, groups 1 and 2 reported the same mean stress score with no significant difference (p = 0.496). Most patients did not experience claustrophobia or other negative symptoms. Only one patient in group 1 felt “massive stress” during the examination. These results are summarised in Table 3.
Importance of direct interaction with a radiologist
Significantly more patients in group 1 (81%) indicated that the opportunity to discuss imaging findings with a radiologist is part of a good radiology service, compared with 14% in group 2 (p < 0.001) (Table 4).
Perception of competence
Significantly more patients from group 1 (mean score 4.72) perceived high competence of the radiology department compared with group 2 (mean score 4.09) (p < 0.001) (Table 4).
Bond between patient and radiology department
Patients in group 1 showed a stronger bond to the radiology institute than patients in group 2 (p = 0.001), with a significant majority wanting only to be examined in the same department in case of future imaging studies, independent of the recommendations by the family doctor or specialist (93% in group 1 and 75% in group 2). Patients in group 2 thus showed a significantly lower bond to the radiology institute (Table 4).
Patients’ concerns about radiology findings and results
Most of the patients (76 %) were concerned about their radiology findings (answer “worrying about results” or “excessively worrying about results”). However, there was no significant difference between the two groups (p > 0.179) with regards to patients’ concern about the radiology results (Table 5).
Duration of interview after MRI examination
The duration of the discussion in group 1 averaged a mean of 3 min and 47 s (range 1–15 min).
Discussion
In this study, we showed that direct communication to discuss imaging findings between the radiologist and the patient had significant benefits by increasing emotional bonding to the department, and improving the confidence of patients in the imaging department.
Patients perceived the chance to discuss their imaging with a radiologist as a highly valuable quality feature and add-on, with 81% of patients experiencing direct communication with the radiologist stating that this was an important feature of the radiology service. Apparently the comparative group just was not aware of the benefits of radiology, as they answered positively only in 14%. Furthermore, the opportunity to talk to a radiologist directly after MRI scanning led the patients to perceive the imaging department as being more competent (mean score 4.72) compared with patients who were not offered the opportunity to discuss their scan findings with the radiologist (mean score 4.09) (p < 0.001). In addition, patients appeared to be more emotionally attached to the same radiology department after direct communication of the results by the radiologist. About 93% of patients from group 1 wanted to be imaged again exclusively in the same department, compared with only 75% in group 2 (p = 0.001). Nonetheless, a visit to the radiology department including imaging results was deemed to be a stressful experience by both groups, with no significant difference in the frequency or perception of severity of this stress.
In the current healthcare system, there is an ongoing debate about patient-oriented medicine. This alludes to personalised medicine with strong human interaction and relationship, which is also called “humanised” medicine. In addition to providing psychological support for patients, patient-oriented medicine can improve care quality and more efficient use of economic resources [12].
The main goal of a radiology report is to communicate the results of the radiology findings and interpretation to the referring physician or to the patient. The report must be accurate and easily understood. Reports should employ clear, unambiguous language [13]. In daily routine, the radiologist’s communication is limited almost exclusively to the referring physician. The patient is seldom seen and perceived by the radiologist. In recently published papers [6, 7], it was found that only 10–20% of the patients were seen by the radiologist. This means that for up to 80% of patients the radiologist is “invisible” and the patient is not aware of the importance of the role of radiologist in his care management pathway.
In the last few years, there has been an ongoing discussion as to whether the radiologist should limit its role to a “pure imager” or whether the radiologist should act as a more patient-oriented physician within the healthcare management [5, 14,15,16,17,18,19,20,21,22,23]. Intensive professional discussions about the role of the radiologist in the healthcare system of the future are ongoing. According to more recent ideas, the radiologist should take concrete steps towards a leadership role in shaping the future healthcare system. This goal is summarised in a recent publication and defined as a new concept called “Imaging 3.0” [24]. The idea of a new form of radiology organisation focusses stronger on the patient and individual needs improving service quality and professional relationship. However, to our knowledge, there are no published studies proving the potential impact of such an approach.
Recent publications have shown that patient distress about the outcomes of their radiology tests can be very high [25]. In the study by Flory and Lang it was shown that the stress associated with uncertainty of imaging diagnoses can be higher than that experienced while awaiting invasive and potentially more risky treatment [25]. Our study showed similar results, with significant stress accorded to the uncertainty of imaging results. Hence, the opportunity for radiologists to reveal imaging findings to patients directly after a radiological test can help to overcome this stress and thus help to reassure the patient.
In another recent publication, Lo Re et al. [1] reported that 54% of patients had relevant anxiety concerning the results of their radiology examination. These results are slightly lower than in our study (77%) with comparable results. However, their study [1] only evaluated oncological patients, whereas our study included both oncological and non-oncological patients. Non-oncological patients could be more concerned about radiology findings, because they have less prior experience of hospitals and radiology procedures compared with oncological patients.
The economic operation of a radiology institute is expensive and requires much effort. Many radiology institutes are suffering from an increasing workload. The general question arises whether it makes sense to assign a broad additional task to the radiologists, which in most cases will not be directly remunerated? Imaging is at present predominately the domain of radiologists, but clinicians from other specialties have begun encroaching on certain areas of medical imaging. If radiologists do not do a better job of advertising our added value, we risk further losses in our recognition as the imaging experts. This might even bear the advantage that images produced in these departments may also be reported remotely [26]. Consequently, the patients’ awareness of the radiologist’s expertise will on a long-term basis diminish replacement strategies.
Radiologists should be aware that the traditional view of the radiologist in a dark room in front of an imaging workstation and adding value to the healthcare system solely by interpreting images is rapidly becoming outdated [27]. Closing the communication loop by including the radiologist besides the referring clinician into patient interaction can significantly improve the value of radiologists in the healthcare system and patient care. There is an opportunity to address this, as machine learning and artificial intelligence promise to revolutionise the radiologists’ workflow, liberating them from the more mundane tasks and thus allowing them to focus on activities that add value. Moreover, a radiologist perceived by his patients as a unique expert could increase his value and thus classically be part of a successful marketing strategy.
Most radiologists have distanced themselves from patient communication for many years, and to address this effectively, care, empathy and sensitivity are required besides adapting the language level. The conversations can be sometimes difficult and complex. In our study, the discussion lasted an average of 3 min and 47 s. But there were also longer interactions of up to 15 min. To do this effectively, good organisation, sympathy, empathy and sensitivity are required, but communication might also be burdening especially when the patient needs basic explanations.
We are aware that this approach cannot be expected to solve all the problems of radiology and that it cannot be implemented in any institute, especially as this approach can reduce the efficiency and economics of radiology departments. It is also clear that this approach would have to be voluntary and that no radiologist can be forced if he does not want it.
There are limitations to our current study. First, the study set-up was carried out with one single radiologist (AG), who has been interested and trained in patient communication for many years. It is not certain whether other radiologists are able to emulate this model without appropriate training. Second, our study was conducted under controlled/model conditions of outpatient studies. Further investigations should be carried out to determine how this model may be implemented in other clinical conditions with emergencies and other work pressures. Third, communication with patients by the radiologist has economic cost. No economic analysis was carried out on how much of the personnel would have to be deployed in order to implement this model. The questionnaire was intentionally short to encourage patient participation.
Patients with a new diagnosis of malignant disease may be exposed to severe stress. As we have not separated between oncological and non-oncological patients, further studies may need to focus on separating the two groups.
The response rate in group 1 is higher than the response rate in group 2. We suspect that the motivation in group 1 increased because of the stronger bonding. However, it cannot be ruled out that a certain selection bias has taken place.
Conclusions
In the present study, we showed that the patients’ stress associated with the uncertainty of radiology diagnosis is very high. However, direct communication of the imaging findings by the radiologist to patients after the MR imaging study helps to improve the positive perception of competence and bonding to the radiology department. Once experienced, patients prefer to discuss their scan findings with the radiologists and perceive this as an integral part of a good radiology service. This communication concept may help to redefine our profession as an imaging physician with high relevance for patient care and thus augment the awareness and value of radiological expertise.
References
Lo Re G, De Luca R, Muscarneri F et al (2016) Relationship between anxiety level and radiological investigation. Comparison among different diagnostic imaging exams in a prospective single-center study. Radiol Med 121:763–768
Mettler FA, Bhargavan M, Faulkner K et al (2009) Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources—1950–2007. Radiology 253:520–531
Dendl LM, Teufel A, Schleder S et al (2017) Analysis of radiological case presentations and their impact on therapy and treatment concepts in internal medicine. Rofo 189:239–246
Miller LS, Shelby RA, Balmadrid MH (2016) Patient anxiety before and immediately after imaging-guided breast biopsy procedures: impact of radiologist-patient communication. J Am Coll Radiol 13:e62–e71
Berlin L (2009) Communicating results of all outpatient radiologic examinations directly to patients: the time has come. AJR Am J Roentgenol 192:571–573
Glazer GM, Ruiz-Wibbelsmann JA (2011) The invisible radiologist. Radiology 258:18–22
Margulis AR, Sostman HD (2004) Radiologist-patient contact during the performance of cross-sectional examinations. J Am Coll Radiol 1:162–163
Boland GW, Glenn L, Goldberg-Stein S et al (2017) Report of the ACR's economics committee on value-based payment models. J Am Coll Radiol 14:6–14
Spielberger CD et al (1980) State-trait anxiety inventory—Forma Y. Milano, Giunti O.S, pp 81–95
Rogers CR, Dorfman E, Nosbüsch E (1972) Client-centered therapy. Kindler Verlag, München
Schulz von Thun F (2006) Miteinander Reden. Rowohlt-Taschenbuch-Verlag, München
Sacristán J (2013) Patient-centered medicine and patient-oriented research: improving health outcomes for individual patients. BMC Med Inform Decis Mak 13:6
Kahn CE, Langlotz CP, Burnside ES et al (2009) Toward best practices in radiology reporting. Radiology 252:852–856
Levitsky DB, Frank MS, Richardson ML, Shneidman RJ (1993) How should radiologists reply when patients ask about their diagnoses? A survey of radiologists' and clinicians' preferences. AJR Am J Roentgenol 161:433–436
Pahade J, Couto C, Davis RB, Patel P, Siewert B, Rosen MP (2012) Reviewing imaging examination results with a radiologist immediately after study completion: patient preferences and assessment of feasibility in an academic department. AJR Am J Roentgenol 199:844–851
Smith JN, Gunderman RB (2010) Should we inform patients of radiology results? Radiology 255:317–321
O'Mahony N, McCarthy E, McDermott R, O'Keeffe S (2012) Who's the doctor? Patients' perceptions of the role of the breast radiologist: a lesson for all radiologists. Br J Radiol 85:e1184–e1189
Koney N, Roudenko A, Ro M, Bahl S, Kagen A (2016) Patients want to meet with imaging experts. J Am Coll Radiol 13:465–470
Cabarrus M, Naeger DM, Rybkin A, Qayyum A (2015) Patients prefer results from the ordering provider and access to their radiology reports. J Am Coll Radiol 12:556–562
European Society of Radiology (ESR) (2017) ESR concept paper on value-based radiology. Insights Imaging 8:447–454
Erdoğan N, İmamoğlu H, Görkem SB, Doğan S, Şenol S, Öztürk A (2017) Preferences of referring physicians regarding the role of radiologists as direct communicators of test results. Diagn Interv Radiol 23:81–85
Mangano MD, Rahman A, Choy G, Sahani DV, Boland GW, Gunn AJ (2014) Radiologists' role in the communication of imaging examination results to patients: perceptions and preferences of patients. AJR Am J Roentgenol 203:1034–1039
Miller P, Lightburn J, Gunderman R, Miller D (2012) Radiologists' role: the patient's perspective. Radiological Society of North America 2012 Scientific Assembly and Annual Meeting, 25–30 November 30, 2012
Norbash A, Bluth E, Lee CI (2014) Radiologist manpower considerations and Imaging 3.0: effort planning for value-based imaging. J Am Coll Radiol 11:953–958
Flory N, Lang EV (2011) Distress in the radiology waiting room. Radiology 260:166–173
European Society of Radiology (Statement) (2010) The future role of radiology in healthcare. Insights Imaging 1:2–11
Knechtges PM, Carlos RC (2007) The evolving role of radiologists within the health care system. J Am Coll Radiol 4:626–635
Acknowledgements
Deep thanks are due to Friedemann Schulz von Thun from Hamburg in Germany, who is an important scientist and teacher of psychology and communication. The education in his institute opened our minds in many aspects.
We would like to thank our medical technologists, who try to improve good communication practice doing the best possible for our patients.
We thank Nicole Graf, who has supported us as a professional statistician in the evaluations (www.graf@biostatistics.ch).
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Andreas Gutzeit.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Nicole Graf kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• prospective
• randomised controlled trial
• performed at one institution
Rights and permissions
About this article
Cite this article
Gutzeit, A., Heiland, R., Sudarski, S. et al. Direct communication between radiologists and patients following imaging examinations. Should radiologists rethink their patient care?. Eur Radiol 29, 224–231 (2019). https://doi.org/10.1007/s00330-018-5503-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5503-2