Abstract
Purpose
We set out to compare outcomes in CT-guided lumbar transforaminal nerve root block patients receiving either particulate or non-particulate corticosteroids.
Materials and methods
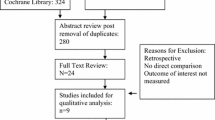
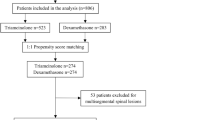
This was a retrospective comparative effectiveness outcomes study on two cohorts of lumbar radiculopathy patients. 321 received particulate and 173 non-particulate corticosteroids at CT-guided transforaminal lumbar nerve root injections. The particulate steroid was used from October 2009 until May 2014 and the non-particulate steroid was used from May 2014. Pain levels were collected at baseline using an 11-point numerical rating scale (NRS) and at 1 day, 1 week and 1 month. Overall ‘improvement’ was assessed using the Patients’ Global Impression of Change (PGIC) at these same time points (primary outcome). The proportions of patients ‘improved’ were compared between the two groups using the Chi-square test. The NRS change scores were compared using the unpaired t-test.
Results
A significantly higher proportion of patients treated with particulate steroids were improved at 1 week (43.2 % vs. 27.7 %, p = 0.001) and at 1 month (44.3 % vs. 33.1 %, p = 0.019). Patients receiving particulate steroids also had significantly higher NRS change scores at 1 week (p = 0.02) and 1 month (p = 0.007).
Conclusion
Particulate corticosteroids have significantly better outcomes than non-particulate corticosteroids.
Key Points
• Better pain relief is achieved with particulate steroids.
• Significantly more patients report overall ‘improvement’ with particulate steroids.
• Significantly more patients report ‘worsening’ at 1 week with non-particulate steroids.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar epidural transforaminal and interlaminar injections with particulate or non-particulate corticosteroids and local anaesthetics are commonly used to treat patients with symptoms of radiculopathy, but have been the focus of extensive discussions in the literature in recent years [1,2,3,4,5]. The trigger for these discussions was the warning published by the US Food and Drug Administration (FDA) in 2011 and 2014 [6, 7]. The topic of the warning was the use of particulate corticosteroids (triamcinolone acetonide) for epidural use. The reason for this particular warning was that this corticosteroid had never been authorised for epidural use by the FDA. The safety announcement in 2014, with the main statement that “injections into the epidural space may result in rare but serious adverse events, including loss of vision, stroke, paralysis and death” was based on a few cases from the FDA Adverse Event Reporting System (FAERS) and 15 references from the literature concerning complications during or after epidural corticosteroid injections. In response to the warning, the willingness to use particulate corticosteroids for epidural injections was drastically reduced and many physicians changed to non-particulate corticosteroids for the epidural injections. This included our specialised orthopaedic and rheumatological university hospital that implemented this change in May 2014. Prior to this date only particulate corticosteroids were used for the transforaminal and epidural injections of the lumbar spine.
Therefore, the purpose of this study was to compare the outcomes of patients receiving lumbar transforaminal epidural steroid injections (nerve root blocks) with particulate (triamcinolone acetonide) versus non-particulate (dexamethasone dihydrogen phosphate) steroids at 1 day, 1 week and 1 month post-injection.
Materials and methods
Patient population
In this comparative effectiveness retrospective analysis of treatment outcomes that were collected prospectively, we monitored two independent groups of patients referred to our radiology department for CT-guided transforaminal epidural therapeutic injections of the lumbar spine [8, 9]. One group (N=321) was treated with a particulate corticosteroid (i.e. 40 mg triamcinolone acetonide; Triamcort Depot, Helvepharm AG, Frauenfeld, Switzerland) and the other group (N=173) received a non-particulate corticosteroid (i.e. 4 mg dexamethasone dihydrogenphosphate; Fortecortin Inject, Merck AG, Zug, Switzerland). All patients received only one infiltration per level and side for the results of this analysis. The particulate steroid was used from October 2009 until May 2014. The non-particulate steroid was used from May 2014 after release of the safety announcement of the FDA. The patients were referred to our specialised orthopaedic/rheumatology university hospital by orthopaedic specialists, general practitioners and chiropractors. Both cohorts include consecutive lumbar transforaminal epidural injection patients registered in the radiology department outcomes database who returned follow-up outcomes postal questionnaires. Patients receiving the particulate corticosteroid preparation underwent transforaminal epidural injections between October 2009 and 8 May 2014. Patients receiving the non-particulate corticosteroid preparation underwent transforaminal epidural injections between 09 May 2014 and 31 October 2014. Before and after the injection procedure the same information was given to each patient of both groups, without any difference concerning the type of the steroid.
Informed consent was obtained before the intervention. The benefits and risks of the intervention were explained and discussed with the patients with no difference between the two cohorts.
The study was approved by the institutional review board.
Epidural injection procedure
All lumbar transforaminal epidural injections were performed as an outpatient procedure. To guarantee consistency of the procedure a standardised protocol was applied for all interventions.
A CT (64-detector row CT, Philips Brilliance; Philips Medical Systems, Best, The Netherlands or 64-detector row CT, Somatom Definition AS, Siemens Healthcare, Erlangen, Germany) was used to guide the needle route for the intervention. The initial low-dose CT acquisition was performed in a prone position at the requested nerve-root level. In this initial CT the radiologist chose the best point for the needle insertion before starting the injection procedure. After skin disinfection the subcutaneous application of local anaesthetics was performed. The needle (23-gauge 7 cm, Terumo Europe, Leuven, Belgium or 22-gauge 12.7 cm spinal needle, BD Europe, Temse, Belgium) was introduced into a transforaminal position with the needle tip near to the nerve root (Fig. 1) and 0.5 ml iopamidol (Iopamiro 200, 200 mg of iodine per millilitre; Bracco, Milan, Italy) was injected to verify a good position of the needle and a nonvascular distribution of the contrast media. Afterwards 40 mg (1 ml) of triamcinolone acetonide or 4 mg (1 ml) of dexamethasone dihydrogenphosphate were slowly injected, followed by the injection of 1 ml of 0.2 % ropivacaine (Naropin; Astra-Zeneca, Södertälje, Sweden).
Transverse CT fluoroscopy image of lumbar transforaminal epidural injection of the left L5 nerve root in 30-year-old women with left L5 radiculopathy. The procedure was performed in the prone position. (a) Dorsal approach through the left L5 foramen with a 25-gauge needle. (b) Distribution of the contrast media around the L5 nerve root after the needle was placed in the final position
Outcome measures
Pain levels of the patients were assessed while they were in the radiology department immediately prior to the lumbar transforaminal epidural intervention (baseline) using an 11-point numerical rating scale (NRS) where 0 means no pain and 10 means insufferable pain. Post-injection, in addition to the NRS pain levels, the Patients’ Global Impression of Change (PGIC) scale data was collected at 1 day, 1 week and 1 month post-injection. The PGIC is a 7-item scale that includes the responses ‘much better’, ‘better’, ‘slightly better’, ‘unchanged’, ‘slightly worse’, ‘worse’ and ‘much worse’ [10, 11]. Only the responses ‘much better’ and ‘better’ were deemed clinically relevant ‘improvement’ (primary outcome) as used in other studies [2, 10]. The responses ‘slightly worse’, ‘worse’ and ‘much worse’ were deemed as ‘worsening’ of the overall condition. ‘Worsening’ was a secondary outcome measure, as were the follow-up pain scores. Immediately before leaving the radiology department a prepaid postal questionnaire containing the 1-day, 1-week and 1-month NRS and PGIC questions was given to the patients and the patients were asked to complete the questionnaire and send it back.
Statistical analysis
The Mann-Whitney U test for non-parametric data was used for the age comparison of the two groups. The Chi-square test was used to analyse differences in sex distribution between the two cohorts.
The unpaired Student’s t-test was used to compare the NRS change scores (normally distributed data) for the two groups at 1 day, 1 week and 1 month after the injection.
For the primary outcome measure of clinically relevant ‘improvement’ at 1 day, 1 week and 1 month post-injection, the comparison between the two groups was performed with the Chi-square test. The proportion of patients reporting ‘worsening’ of their condition were also compared between the two groups using the Chi-square test at 1 day, 1 week and 1 month post-injection. P-levels lower than 0.05 were considered statistically significant.
All calculations were done with the statistical software package SPSS Statistics Version 21 (IBM, Armonk, NY, USA).
Results
Included were 321 patients in the particulate corticosteroid group and 173 patients in the non-particulate corticosteroid group. There was no significant age (p = 0.25) or sex (p = 0.93) difference between the two groups. For the particulate corticosteroid group 50.3 % of the patients were female and for the non-particulate group 51.1 % of the patients were female. The mean age for the particulate steroid cohort was 57.78 (SD = 14.83) years and for the non-particulate steroid cohort 59.40 (SD = 14.91) years. There was also no significant difference in the baseline pain scores between the two cohorts (p = 0.064). Patients receiving the particulate corticosteroid had a mean baseline NRS score of 6.02 (SD = 2.31) and the non-particulate corticosteroid patients had a mean baseline NRS score of 6.43 (SD = 2.38).
The primary outcome of ‘improvement’ found that there was no significant difference in the proportion of patients reporting ‘improvement’ at 1 day (p = 0.330). However, at both 1 week (p = 0.001) and 1 month (p = 0.019) a significantly higher proportion of patients receiving the particulate steroids reported clinically relevant ‘improvement’ (Table 1).
There was no significant difference in the proportion of patients reporting ‘worsening’ at 1 day (p = 0.197) or 1 month (p = 0.11). However, there was a significant difference at 1 week (p = 0.032), with a higher proportion of the non-particulate steroid group reporting being ‘worse’ compared to the particulate steroid group (Table 1).
For the secondary outcome of NRS change scores, there was no significant difference in the 1-day post-injection change scores (p = 0.646) between the two groups. However, significant differences in the 1-week change scores (p = 0.008) and the 1-month change scores (p = 0.021) were found (Table 2).
There were no significant adverse events for either group of patients after the transforaminal epidural injections.
Discussion
The results of this study show the superiority of particulate corticosteroids compared to non-particulate corticosteroids in providing clinically relevant ‘improvement’ for patients receiving transforaminal lumbar epidural injections at both 1 week and 1 month post-injection. Additionally, patients receiving the non-particulate corticosteroids were significantly more likely to report ‘worsening’ at 1 week post-injection. For patients receiving the particulate corticosteroids, 16 % more reported clinically relevant improvement at the 1-week time point and 10 % more patients reported improvement when treated with the particulate steroids at the 1-month time point compared to patients receiving the non-particulate steroid. These may appear to be small numbers, but for these patients the results are clinically relevant. Additionally, the results show a statistically significant difference in NRS change scores at 1 week and 1 month with those patients receiving the particulate corticosteroids having a larger amount of pain reduction. The NRS change scores for the 1-week and 1-month time points had more than a 30 % difference between the two groups, favouring the particulate steroid patients.
The replacement of the particulate steroids by non-particulate steroids in our department in May 2014 was prompted by the FDA safety announcement. In our specialised orthopaedic/rheumatological university hospital we changed the type of steroids for the epidural transforaminal nerve root blocks as well as for the epidural interlaminar injections assuming that there would be no significant difference in treatment outcomes [2]. The results of this current study support the previous research published for interlaminar injections [2], which also found that the non-particulate corticosteroids had significantly worse outcomes compared to the particulate corticosteroids, with even larger differences between the two groups for the NRS change scores compared to this current study. Knowledge about the superior outcome when using particulate steroids is important information for both the patients and the referring physicians. Indeed, some patients and especially those doctors who routinely referred their patients for these procedures complained about lack of effect or a smaller effect soon after the switch from particulate to non-particulate steroids in 2014.
There are a number of other studies in recent years that support our results.
McCormick et al. compared transforaminal epidural injections with triamcinolone versus bethamethasone in 1,568 injections in a longitudinal cohort study. They used triamcinolone in 78.8 % and betamethasone in 21.2 % of the injections. Significantly more patients who received triamcinolone had higher levels of pain relief in the short-term follow-up (1–4 weeks) [12]. Choi et al. looked at the outcomes of 262 patients with a moderate disability caused by degenerative lumbar spinal disease who received transforaminal epidural injections with triamcinolone and lidocaine. 204 of these patients had significant pain relief at the 3 months’ follow-up after the epidural injection [13]. That supports our results of significant pain relief after epidural injections with triamcinolone.
Kim and Brown reported only a trend for better pain relief with particulate steroids in their study with 30 patients who received translaminar epidural injections with either particulate or non-particulate steroids [14]. This lack of statistical significance in their study may be due to the small sample size. The work by Park et al. also supports our results. They showed better pain relief for triamcinolone acetonide in 106 patients with transforaminal epidural injections [15]. Kennedy et al. reported in their double-blind, prospective trial with 78 patients who received transforaminal epidural injections with particulate or non-particulate steroids that there was a trend for higher pain relief after injection of particulate steroids (43.2 % vs. 31.7 %) 2 weeks post-injection, and a higher number of repeat injections was necessary in the group receiving the non-particulate steroids [16].
In contrast to the studies cited above, there are also studies that do not support the results of our current study. El-Yaahchouchi et al. reported in their retrospective analysis of 3,645 transforaminal lumbar epidural injections no significant superiority for particulate or non-particulate steroids at 2 months post-injection [17, 18]. Additional studies support their results [18, 19]. The most recent study by McCormick et al. included 78 patients and found no significant difference in pain relief for the different corticosteroids. However, only a small group of 23 patients in this study received triamcinolone and as the outcome measure only the numeric rating scale was used, without analysis of overall improvement or worsening in daily life [18].
Although there are reasons to criticise the FDA warnings of April 2014, as did Manchikanti et al. [20], it is actually a fact that there are more complications/serious adverse events after lumbar spinal epidural particulate corticosteroid injections compared to non-particulate injections. The FDA warning of 2014 was based on a review of cases from the FAERS. Most of these cases were complications after cervical transforaminal injections and based on 15 references from the medical literature [7]. An incomplete review of the medical literature and the main focus on cervical injections might be a reason to question the FDA warning (10 of the 15 references in the FDA warning are about adverse events after cervical injections and one after an interlaminar thoracic injection). Overall, there are a substantial number of reported adverse events and warnings for cervical epidural injections reported in the literature [21,22,23,24,25,26], but only a few studies reported adverse events for lumbar epidural injections. Sixteen cases of spinal cord ischaemia have been reported in the literature since 2002 for lumbar epidural steroid injections with particulate steroids [27,28,29,30,31,32]. From 2002 to 2010 Wybier et al. found seven reported cases of paraplegia in the English medical literature [28]. In five of these cases prednisolone acetate was used and its high tendency to build macro-aggregates was discussed as the reason for arterial embolisation. Furthermore the correlation between prior surgery and post-interventional adverse events are discussed [28, 33, 34]. Particularly in interlaminar lumbar epidural injections there are no reported cases of serious adverse events without previous surgery. In all reported cases particulate steroids were used.
Serious adverse events are an extremely rare complication in transforaminal epidural steroid injections with particulate steroids. El-Yahchouchi et al. recently looked at 14,956 transforaminal epidural injections with either a particulate or non-particulate steroid, with the majority of injections (89 %) performed at lumbosacral segments. They found only minor adverse events such as vasovagal reaction, allergic reaction, increased pain, central steroid effects and diabetic complications but no serious adverse events [35]. Plastaras et al. reported the same results in 2015 when comparing 2,025 lumbosacral transforaminal epidural steroid injections using betamethasone or triamcinolone. Also in these cohorts there were no permanent adverse events reported [36]. This study was performed by CT guidance, which is a safe and most widespread technique. CT guidance shows the best direct access to the nerve root.
A limitation of our study is that it is a comparative effectiveness cohort study and not a randomised clinical trial with a placebo group or randomisation of patients into either a particulate or a non-particulate steroid group. However, the sample sizes were large and there were no significant differences in patient age, sex or baseline pain scores between the two groups. It is stated that cohort studies are more likely to represent everyday clinical practice compared to participants in randomised clinical trials [8, 9].
A further limitation is the lack of data on clinical information and oral medication use of the referred patients.
Another limitation could be that we did not compare the outcomes to the imaging findings. However, this was purposeful as a study by Lechmann et al., from our institution, showed that only one of six imaging findings evaluated was linked to a significant improvement and higher NRS change scores and that this single finding only affected 20 out of the 156 patients [37].
Furthermore, no outcome data were collected between the 1 week and 1 month time point, consistent with several other similar studies [37]. A longer follow-up than 1 month would also be desirable.
While the difference in NRS change scores being less than 1 point between the two groups appears to be a limitation, there is in fact at least a 30 % difference between these scores for the two different patient groups, which is clinically relevant.
Conclusion
This study showed superior treatment outcomes for patients receiving particulate corticosteroids compared to patients receiving non-particulate corticosteroids for their transforaminal epidural injections in terms of overall ‘improvement’ as well as pain reduction. Although the results are just significant for a small part of the study population, for these patients it is an improvement of life quality. Because of the results of this study as well as the fact that this hospital is not located in the USA and thus not under the jurisdiction of the FDA, we now offer patients a choice between particulate or non-particulate steroids for their lower lumbar transforaminal epidural infiltration and provide detailed oral and written information about possible serious adverse events. The majority of the patients choose the particulate steroids.
References
Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CW (2015) Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiol 44:149–155
Bensler S, Sutter R, Pfirrmann CW, Peterson CK (2016) Is there a difference in treatment outcomes between epidural injections with particulate versus non-particulate steroids? Eur Radiol
Friedly JL, Comstock BA, Turner JA et al (2014) A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med 371:11–21
Manchikanti L, Benyamin RM (2015) Key safety considerations when administering epidural steroid injections. Pain Manag 5:261–272
Manchikanti L, Kaye AD, Manchikanti K, Boswell M, Pampati V, Hirsch J (2015) Efficacy of epidural injections in the treatment of lumbar central spinal stenosis: a systematic review. Anesth Pain Med 5:e23139
Kenalog-10 F-USFaDAS, (triamcinolone taiaK-, injection. a. Available at: http://www.fda.gov/safety/medwatch/safetyinformation/ucm262876.htm. Accessed 2015 Feb 15
to FDSCFrlc, corticosteroid worbsnpae, pain. if. Available at: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM394286.pdf. Accessed 2014 Aug 31.
Tinetti ME, Studenski SA (2011) Comparative effectiveness research and patients with multiple chronic conditions. N Engl J Med 364:2478–2481
Neumann PJ (2013) Communicating and promoting comparative-effectiveness research findings. N Engl J Med 369:209–211
Bensler S, Sutter R, Pfirrmann CW, Peterson CK (2015) Long Term Outcomes from CT-guided Indirect Cervical Nerve Root Blocks and their relationship to the MRI findings--A prospective Study. Eur Radiol 25:3405–3413
Fischer D, Stewart AL, Bloch DA, Lorig K, Laurent D, Holman H (1999) Capturing the patient's view of change as a clinical outcome measure. JAMA 282:1157–1162
McCormick Z, Kennedy DJ, Garvan C et al (2015) Comparison of Pain Score Reduction Using Triamcinolone vs. Betamethasone in Transforaminal Epidural Steroid Injections for Lumbosacral Radicular Pain. Am J Phys Med Rehabil 94:1058–1064
Choi JH, Hong JY, Suh SW et al (2016) What Is the Role of Epidural Steroid Injections in Lumbar Spinal Disease with Moderate Disability? Pain Physician 19:293–298
Kim D, Brown J (2011) Efficacy and safety of lumbar epidural dexamethasone versus methylprednisolone in the treatment of lumbar radiculopathy: a comparison of soluble versus particulate steroids. Clin J Pain 27:518–522
Park CH, Lee SH, Kim BI (2010) Comparison of the effectiveness of lumbar transforaminal epidural injection with particulate and nonparticulate corticosteroids in lumbar radiating pain. Pain Med 11:1654–1658
Kennedy DJ, Plastaras C, Casey E et al (2014) Comparative effectiveness of lumbar transforaminal epidural steroid injections with particulate versus nonparticulate corticosteroids for lumbar radicular pain due to intervertebral disc herniation: a prospective, randomized, double-blind trial. Pain Med 15:548–555
El-Yahchouchi C, Geske JR, Carter RE et al (2013) The noninferiority of the nonparticulate steroid dexamethasone vs the particulate steroids betamethasone and triamcinolone in lumbar transforaminal epidural steroid injections. Pain Med 14:1650–1657
McCormick ZL, Cushman D, Marshall B, et al (2016) Pain Reduction and Repeat Injections After Transforaminal Epidural Injection With Particulate Versus Nonparticulate Steroid for the Treatment of Chronic Painful Lumbosacral Radiculopathy. PM R
Denis I, Claveau G, Filiatrault M, Fugere F, Fortin L (2015) Randomized Double-Blind Controlled Trial Comparing the Effectiveness of Lumbar Transforaminal Epidural Injections of Particulate and Nonparticulate Corticosteroids for Lumbosacral Radicular Pain. Pain Med 16:1697–1708
Manchikanti L, Candido KD, Singh V et al (2014) Epidural steroid warning controversy still dogging FDA. Pain Physician 17:E451–E474
Rozin L, Rozin R, Koehler SA et al (2003) Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol 24:351–355
Bose B (2005) Quadriparesis following cervical epidural steroid injections: case report and review of the literature. Spine J 5:558–563
Meyer HJ, Monticelli F, Kiesslich J (2005) Fatal embolism of the anterior spinal artery after local cervical analgetic infiltration. Forensic Sci Int 149:115–119
Ziai WC, Ardelt AA, Llinas RH (2006) Brainstem stroke following uncomplicated cervical epidural steroid injection. Arch Neurol 63:1643–1646
Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS (2007) Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine (Phila Pa 1976) 32:1249–1256
Hodler J, Boos N, Schubert M (2013) Must we discontinue selective cervical nerve root blocks? Report of two cases and review of the literature. Eur Spine J 22:S466–S470
Houten JK, Errico TJ (2002) Paraplegia after lumbosacral nerve root block: report of three cases. Spine J 2:70–75
Wybier M, Gaudart S, Petrover D, Houdart E, Laredo JD (2010) Paraplegia complicating selective steroid injections of the lumbar spine. Report of five cases and review of the literature. Eur Radiol 20:181–189
Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N (2009) Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med 10:1389–1394
Lyders EM, Morris PP (2009) A case of spinal cord infarction following lumbar transforaminal epidural steroid injection: MR imaging and angiographic findings. AJNR Am J Neuroradiol 30:1691–1693
Chang Chien GC, Candido KD, Knezevic NN (2012) Digital subtraction angiography does not reliably prevent paraplegia associated with lumbar transforaminal epidural steroid injection. Pain Physician 15:515–523
Makkar JK, Singh PM, Jain D, Goudra B (2016) Particulate vs Non-Particulate Steroids for Transforaminal Epidural Steroid Injections: Systematic Review and Meta-analysis of the Current Literature. Pain Physician 19:327–340
Thefenne L, Dubecq C, Zing E et al (2010) A rare case of paraplegia complicating a lumbar epidural infiltration. Ann Phys Rehabil Med 53:575–583
Lenoir T, Deloin X, Dauzac C, Rillardon L, Guigui P (2008) Paraplegia after interlaminar epidural steroid injection: a case report. Rev Chir Orthop Reparatrice Appar Mot 94:697–701
El-Yahchouchi CA, Plastaras CT, Maus TP et al (2016) Adverse Event Rates Associated with Transforaminal and Interlaminar Epidural Steroid Injections: A Multi-Institutional Study. Pain Med 17:239–249
Plastaras C, McCormick ZL, Garvan C et al (2015) Adverse events associated with fluoroscopically guided lumbosacral transforaminal epidural steroid injections. Spine J 15:2157–2165
Lechmann M, Rosskopf A, Ehrmann C, Sutter R, Pfirrmann CW, Peterson CK (2016) Relationship of specific MRI findings to treatment outcomes in patients receiving transforaminal epidural steroid injections. Skeletal Radiol 45:1677–1685
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Susanne Bensler.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Bensler, S., Sutter, R., Pfirrmann, C.W.A. et al. Particulate versus non-particulate corticosteroids for transforaminal nerve root blocks: Comparison of outcomes in 494 patients with lumbar radiculopathy. Eur Radiol 28, 946–952 (2018). https://doi.org/10.1007/s00330-017-5045-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5045-z