Abstract
Objectives
To evaluate percutaneous brush cytology, forceps biopsy and a tandem procedure consisting of both, in the diagnosis of malignant biliary obstruction.
Methods
A retrospective review of consecutive patients who underwent biliary brush cytology and/or forceps biopsy between 01/2010 and 09/2014 was performed. The cytology and pathology results were compared to the composite outcome (including radiological, pathological and clinical data). Cost for tandem procedure compared to brush cytology and forceps biopsy alone was calculated.
Results
A total of 232 interventions in 129 patients (70.8 ± 11.0 years) were included. Composite outcome showed malignancy in 94/129 (72.9%) patients. Sensitivity for brush cytology, forceps biopsy and tandem procedure was 40.6% (95% CI 32.6–48.7%), 42.7% (32.4–53.0%) and 55.8% (44.7–66.9%) with 100% specificity, respectively. There were 9/43 (20.9%) additional cancers diagnosed when forceps biopsy was performed in addition to brush cytology, while there were 13/43 (30.2%) more cancers diagnosed when brush cytology was performed in addition to forceps biopsy. Additional costs per additionally diagnosed malignancy if tandem approach is to be utilised in all cases was $704.96.
Conclusion
Using brush cytology and forceps biopsy in tandem improves sensitivity compared to brush cytology and forceps biopsy alone in the diagnosis of malignant biliary obstruction.
Key points
• Tandem procedure improves sensitivity compared to brush cytology and forceps biopsy.
• Brush cytology may help to overcome “crush artefacts” from forceps biopsy.
• The cost per diagnosed malignancy may warrant tandem procedure in all patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous transhepatic biliary drainage (PTBD) is a commonly performed procedure in the diagnosis and treatment of biliary obstruction [1, 2]. First described in 1980 [3], percutaneous transhepatic biliary duct access was used to obtain both cytological and tissue specimens for pathologic diagnosis of the cause of biliary obstruction.
The reported yield of brush cytology and forceps biopsy in the literature varies between 26% and 92% [4,5,6,7,8,9]. Additionally, diagnostic yield of brush cytology and forceps biopsy differs between different locations and tumour entities and additional value of repeated biopsies has been reported. A tandem procedure consisting of both methods could potentially reduce variability and increase diagnostic yield and has been reported to improve diagnostic yield in endoscopic guided biopsies [10]. Furthermore, it may be beneficial compared to performing two separate procedures in cases of an initial negative biopsy owing to the already established access. There are only two studies that evaluate performing both procedures in tandem percutaneously; however, these studies used different techniques that are not routinely used: a smear from the forceps biopsy to obtain cytology instead of independent cytological sampling [6] and a choledochoscopic approach instead of fluoroscopy to obtain samples [7].
A potential downside of the tandem procedure is increased cost associated with performing two tests instead of one. The cost for brush cytology and forceps biopsy is reported to be similar [5]; however, additional diagnostic yield of tandem procedure versus each procedure alone should be demonstrated.
The purpose of our study is to investigate the diagnostic yield and costs associated with tandem procedure consisting of brush cytology and forceps biopsy as compared to each one separately.
Methods
Patients
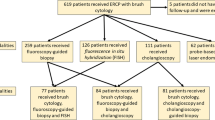
A retrospective search in the interventional radiology (IR) database was performed in this institutional review board approved, Health Insurance Portability and Accountability Act compliant study with waiver of informed consent. All patients who underwent a procedure with the brush cytology device (Cellebrity Cytology Brush Set, Boston Scientific, Marlborough, MA, USA), a procedure with the forceps tissue biopsy device (Radial Jaw Forceps, Boston Scientific, Marlborough, MA, USA) or both at the same time (tandem procedure) under fluoroscopic guidance in a single tertiary academic hospital between January 2010 and September 2014 were included in the study. Patients who underwent a procedure for causes other than suspected malignant biliary obstruction were excluded from the study (Fig. 1).
Procedure
All patients were referred to IR after a failed attempt at endoscopic retrograde access or directly referred to IR because of unfavourable anatomy for an endoscopic approach (e.g. due to hepatico-jejunostomy). The indications for percutaneous biliary procedure were biliary obstruction and a suspected malignancy lesion on cross-sectional imaging. Indication for the type of biliary sampling procedure was based on operator preference as no evidence-based literature was available at that time. All PTBD procedures in our tertiary academic centre are performed by one of the IR fellows under direct supervision of an attending interventional radiologist. After establishing percutaneous access to the biliary system and then to the enteric system, sampling was performed via coaxial technique through a support sheath placed just beyond the area of stricture/mass. By institutional protocol, brush cytology is performed initially, followed by the forceps biopsy. The brush and forceps device were then advanced through the sheath and the sampling device was unsheathed to obtain tissue samples exactly at the level of obstruction. The devices were then retracted within the sheath and removed. Two to three tissue samples (either brush cytology or forceps biopsy or both) were obtained in every procedure.
The brush cytology samples were sent in methanol/water solution (Thin Prep Cytolyt solution, Hologic Inc, Marlborough, MA), and the forceps biopsy specimens were placed in a cup with formalin for transport to pathology.
Data analysis
Data analysis was performed by an IR attending (Olga R. Brook), an IR fellow (Raphael Yoo) and a radiology research fellow (Johannes Boos) with 14, 7 and 3 years of experience in radiology. The following parameters were evaluated: age, gender, biopsy location, type of biopsy performed, indication for biopsy and final diagnosis. Biopsy location was classified as intrahepatic right or left biliary system, biliary confluence, common bile duct, ampulla and bowel/hepaticojejunal (HJ) anastomosis. The cytopathology result was considered positive for malignancy when reported as positive and/or suspected malignancy, and negative when reported as negative, atypical and/or insufficient tissue. Further analysis was performed for all cases with benign causes of biliary obstruction and for cases where the biopsy yielded insufficient tissue, including a “crush artefact” which represents “crushed” material due to the force used during forceps biopsy causing the inability to reach a histopathological diagnosis.
The reference standard was a composite of the current pathology result and pathology result from follow-up procedures within a year after the procedure. For overall sensitivity analysis of the different procedures, all procedures that were performed as part of a tandem procedure were assigned to either brush or forceps biopsy. Therefore, brush cytology from a solitary brush cytology procedure (n = 100) and brush cytology performed as part of a tandem procedure (n = 110) were pooled together (n = 210) for this analysis. Forceps biopsies from solitary forceps procedures (n = 22) were pooled with forceps biopsies from tandem procedures (n = 110, overall n = 132).
Patients who underwent tandem procedure and were diagnosed with cancer by composite outcome were further analysed. All intervention reports, reports of follow-up procedures and clinical patient notes within 1 week after the initial intervention were reviewed for complications such as bleeding, clogging of the biliary drainage, transfer to intensive care unit and death.
Cost analysis
The price of equipment was assessed using information provided by the vendor. Cytology and pathology costs for the brush cytology and the forceps biopsy were assessed using the Medicare reimbursement rates. Overall costs were extrapolated and cost per additional malignancy diagnosis and percent of increased detection rate when using the tandem method compared to both other methods alone was calculated. The formula used was [(cost tandem – cost other method)/(cancer detection rate tandem – cancer detection rate other method)] [11].
Statistical analysis
Data is given as mean ± standard deviation or as median ± interquartile range with 95% confidence intervals (95% CI). Sensitivity of brush cytology and forceps biopsy was compared using the method reported by Bland and Butland [12]. The McNemar test was used to compare brush cytology and forceps biopsy in patients with malignancy that underwent both procedures in tandem. Cohen’s kappa statistics was used to assess agreement between brush cytology and forceps biopsy. The level of statistical significance was set at alpha < 0.05.
Results
Subjects
A total of 232 interventions (129 patients, 61 women, 68 men, age 70.8 ± 11.0 years, range 39–94 years) were included in the study; 210 brush cytology procedures (Fig. 2), 132 forceps biopsies (Fig. 3) and 110 tandem biopsies were included in the study (Fig. 1). Of 232 interventions, 85 (36.6%) were performed at the time of the initial biliary drainage placement and 147/232 (63.4%) were performed at a later time point. Composite outcome showed malignancy in 94/129 patients (72.9%) and another cause for the biliary obstruction in 35/129 (27.1%) patients (Appendix Tables 1 and 2). Rate of malignancy was 143/210 (68.1%) for brush cytology, 89/132 (67.4%) for forceps biopsy and 77/110 (70%) for tandem procedure.
Diagnostic accuracy
Sensitivity to detect malignancy was 58/143 (40.6%, 95% CI 32.6–48.7%) for brush cytology, 38/89 (42.7%, 95% CI 32.4–53.0%) for forceps biopsy and 43/77 (55.8%, 95% CI 44.7–66.9%) for tandem procedure. Sensitivity for benign and malignant causes of biliary obstruction was 76/210 (36.2%, 95% CI 29.7–42.7%) for brush cytology, 64/132 (48.5%, 95% CI 40.0–57.0%) for forceps biopsy and 59/110 (53.6%, 95% CI 44.3–62.9%) for the tandem approach. Sensitivity was comparable between brush cytology only procedure and brush cytology as part of the tandem procedure (24/65, 36.9% vs. 27/77, 44.2%, p = 0.38) and higher for forceps biopsy only procedure compared with forceps as part of the tandem procedure (8/12, 66.6% vs. 27/77, 35.0%, p = 0.04, 95% CI of the difference −2.3% to 57.3%). Specificity was 100% for all methods. Agreement between brush cytology and forceps biopsy in cancer patients was moderate (0.43, 95% CI 0.23–0.63) [13]. Negative predictive value was highest for tandem approach (33/67, 49.3%, 95% CI 37.3–61.3%) compared to brush cytology (72/152, 44.1%, 95% CI 36.2–52.0%) and forceps biopsy (42/94, 45.7%, 95% CI 35.6–55.8%). The tandem approach provided the highest sensitivity for all locations except for the biliary confluence (Table 1) and for all types of malignancy (Tables 2 and 3). Tandem biopsy led to an increased malignancy detection rate of 9/43 (20.9%, 95% CI 11.4–35.2%) compared to brush cytology alone and 13/43 (30.2%, 95% CI 18.6–45.1%) compared to forceps biopsy alone. There was no significant difference regarding the additional value over either method during the tandem procedure (p = 0.52, odds ratio 1.44, 95% CI odds ratio 0.62–3.38).
Complications of the procedure
There were no complications immediately related to the procedure in any of the patients. In 73/232 (32%) of the cases, a biliary intervention was performed within 1 week after the index procedure. In 9/232 (3.9%) cases the drainage catheter was occluded during the follow-up procedure, 4/9 times after brush cytology only and 5/9 times after the tandem procedure. In all nine cases sampling was performed at the time of placement of a percutaneous biliary drainage. Other re-interventions were performed for leakage around the drainage (6/232, 2.6%), re-evaluation of the biliary system for insufficient biliary drainage as detected clinically by lack of decrease in total bilirubin or persistently elevated liver function tests (36/232, 15.5%), stent placement or removal (18/232, 7.8%) and attempts to internalize the drainage (4/232, 1.7%). Analysis revealed no case with tract seeding due to the intervention. One 87-year-old male patient with pancreatic cancer and widespread peritoneal metastatic disease was referred to the intensive care unit after the procedure because of hypotension. The patient died after 5 days; however, autopsy revealed no bleeding and no coherence to the procedure.
Insufficient material for pathological diagnosis
Insufficient material to enable pathological diagnosis was found in 20/342 of all procedures (5.8%; 1/20, 5% in brush cytology, 19/20, 95% in forceps biopsy). Composite outcome analysis revealed malignancies in 14/20 of these cases (70%, 95% CI 51.2–88.2%). In 11 out of 20 cases (58%, 95% CI 34.2–74.2%, all forceps biopsy), the reason for the inability to make the diagnosis was a “crush artefact”. In three out of 11 (27%, 95% CI 1–53.6%) cases with crush artefact in the forceps biopsy, brush cytology enabled diagnosis of malignancy.
Repeated procedures
Initial biopsy was negative in 38/129, 29.5% of the patients (brush cytology n = 23, forceps biopsy n = 2, tandem procedure n = 13). All 38 patients underwent at least one additional biopsy (96 follow-up interventions, median 1, range 1–10).
In 22/38 patients (57.9%), composite outcome revealed a malignancy (cholangiocarcinoma n = 17, pancreatic carcinoma n = 2, hepatocellular carcinoma n = 1, adenocarcinoma with oncocytic features n = 1, melanoma metastasis n = 1). In these 22 patients, 54 follow-up procedures were performed which enabled diagnosis in 15/22 patients (68%; 25/54 procedures, 46%). Diagnosis was achieved at the second procedure in 9/22 (40.9%, 95% CI 20.4–61.4%) patients, at third procedure in 1/22 (4.6%, 95% CI 0–13.4%) patients, at fourth procedure in 4/22 (18.2%, 95% CI 2.1–34.3%) patients and at ninth procedure in 1/22 (4.6%, 95% CI 0–13.4%) cases. The initial procedure was repeated in 36/54 (66.7%, brush cytology n = 29, tandem n = 7), whereas a different procedure was performed in 18/54 cases (33.3%, brush cytology n = 2, forceps biopsy n = 2, tandem procedure n = 14). In cases with repeated procedure of the same modality, diagnosis was achieved in 10/29 (34.5%) cases with brush cytology and 4/7 (57.1%) of cases with tandem procedure. In cases with a different follow-up procedure, diagnosis was achieved in six cases with tandem after brush cytology, two cases with brush cytology after tandem and one case with forceps after brush cytology, forceps after tandem procedure and tandem after forceps procedure, respectively.
Cost analysis
Equipment price at the time of the study was $11.50 for a cytology brush set and $44.00 for a forceps biopsy kit. Medicare reimbursement rates for cytological and pathological analysis for biliary brush cytology and forceps biopsy were $80.85 and $81.74 in 2016, respectively. Therefore, overall cost for a single brush cytology was $92.35, for a single forceps biopsy was $125.74 and for a single tandem procedure was $218.09 (Table 4).
If the tandem approach was used for all patients, then cost per detection of one additional malignancy compared to brush cytology alone would be $827.24, and compared to forceps biopsy alone it would be $704.96.
Discussion
We have found improved sensitivity for percutaneous transbiliary diagnosis of malignant biliary obstruction by performing brush cytology and forceps biopsy in tandem as compared to performing each procedure alone. Compared to brush cytology and forceps biopsy alone, the tandem approach enabled additional diagnosis of 21% and 30% of malignancies, respectively.
In our study the sensitivity was highest for the tandem approach and we have found only moderate agreement between brush cytology and forceps biopsy with a kappa value of 0.43, which indicates that using both methods in tandem is preferable. The sensitivity of brush cytology of 41% and forceps biopsy of 43% found in this study is within the range of values reported in the literature from 26% to 75% [4,5,6,7, 14] for brush cytology and 30% to 92% for forceps biopsy [4,5,6,7,8,9]. The increase in sensitivity between sampling with either procedure and the tandem approach is most likely the result of sampling error. Although forceps biopsy leads to a larger sample, the site of malignancy could be missed because of lack of direct visualization, as it is difficult to differentiate between cancer and secondary inflammatory changes in fluoroscopy. Of note, we found a higher sensitivity for the forceps biopsy alone procedure compared with forceps as part of the tandem procedure; however, only a small number of stand-alone forceps biopsies in patients with malignancy were available.
Our results regarding the superiority of the tandem approach are in contrast with two previous studies which reported no additional value of the combination of brush cytology and forceps biopsy [4, 6]. Nevertheless, comparison of prior studies to our results is limited. Rossi et al. [4] used forceps under choledochoscopic instead of fluoroscopic guidance and only investigated 22 tandem procedures. Tapping et al. [6] agitated the forceps device in cytological solution after the biopsy instead of performing an independent brush cytology.
In contrast, Savader et al. [5] performed multiple biopsies using either brush cytology, forceps under choledochoscopic guidance and forceps under fluoroscopic guidance and found 17% of the initially negative malignancies to be detected using another biopsy technique during re-intervention. They do not report which technique was used initially and at re-intervention which limits comparison with our results. Of note, the complementary nature of core biopsy and cytology has also been reported in the sampling of pulmonary nodules [15, 16].
A recent study reported a true positive rate for diagnosis by forceps biopsy of 88% [17], considerably higher than in our study. However it is hard to make true comparison between the study by Li et al. and our study, as a number of important descriptors are missing in their methods, such as size of forceps biopsy and location of biliary obstruction.
We found a similar sensitivity for detection of cholangiocarcinoma by fluoroscopic guided brush cytology (38%) and forceps biopsy (35%) alone, whereas it was considerably higher for the tandem approach (58%). Previous studies reported a wide range of sensitivities of 0–87% for brush cytology and 0–94% for fluoroscopic guided forceps biopsy [4,5,6]. Additionally, we found brush cytology as a part of the tandem procedure to be helpful in the diagnosis of cholangiocarcinoma which is in contrast to the study by Savader et al. who reported a sensitivity of 0% in 21 cases and discussed that brush cytology may not be useful in the diagnosis of cholangiocarcinoma because of the fibrotic nature of the malignancy [5]. Of note, the location with highest sensitivity by tandem approach (66%) in this study was the common bile duct site which is in accordance with previously reported results [6].
The forceps biopsy technique is known to have a limitation in the form of “crush artefact” [18] which describes destruction of tissue as a result of the force generated using the forceps biopsy. In our study, “crush artefact” led to non-diagnostic biopsy material in 9% of the procedures, of which 91% had a malignancy at the composite outcome. Of these cases, 30% could be diagnosed by brush cytology which is performed without putting force on the tissue and may help to overcome this limitation.
We found additional costs of $705 per detected malignancy when using the tandem approach. Considering the average reported medical cost per patient with pancreatic cancer ($49,000 to $135,000) [19], the additional cost of the tandem approach seems negligible. Of note, our results indicate that repeated biopsy is successful in 44% of the cases. It could be more efficient to perform an initial biopsy and only in negative cases add a second procedure; however, compared to costs of the biopsy kits, the costs for an additional procedure seem to be much higher and performing the tandem approach in the initial procedure seems reasonable. Although not evaluated in this study, there may be a positive effect on patient outcome due to earlier diagnosis of malignancy which warrants further studies.
Our study has a number of limitations. While previous studies have reported percutaneous brush cytology or forceps biopsy to be performed for all patients with suspected malignant biliary obstruction [6], in our hospital endoscopic retrograde cholangio-pancreatography (ERCP) is the initial method of choice in these patients. This may be a selection bias leading to lower values of sensitivity. Additionally, although a large number of interventions were included in our study, the patient population was heterogeneous with different types of malignancy, tumour locations and tumour sizes which may limit generalisability of our findings to other institutions.
Reimbursement rates for brush cytology and forceps biopsy may vary between regions and practices which limits generalisability of our cost analysis. We did not include additional costs for medical personnel and the additional procedure time in our cost analysis as the additional time for brush cytology during the procedure is relatively short. We did not analyse the additional costs of added procedures in cases of non-diagnostic procedures including additional hospital stays or costs from delayed diagnosis of malignancies. Biliary drainage placement often leads to inflammatory changes which can be difficult to distinguish from malignancy. We accounted for this by not counting atypical results as positive cases. Lastly, interventional procedures were performed by different interventional radiologists and pathological diagnosis was performed by different pathologists. We did not analyse the impact of the performing physicians and their level of expertise regarding procedure accuracy; however, all procedures were performed by one interventional fellow under supervision of an interventional staff radiologist.
In conclusion, fluoroscopically guided brush cytology and forceps biopsy procedures performed in tandem provide improved sensitivity compared to brush cytology and forceps biopsy alone in the percutaneous diagnosis of malignant biliary obstruction. The cost per additional diagnosed malignancy may warrant tandem procedure in all patients with suspected malignant biliary obstruction.
Abbreviations
- PTBD:
-
Percutaneous Transhepatic Biliary Drainage
- IR:
-
Interventional Radiology
- HJ:
-
Hepaticojenunal
References
Pereiras RV, Rheingold OJ, Huston D et al (1978) Relief of malignant obstructive jaundice by percutaneous insertion of a permanent prosthesis in the biliary tree. Ann Intern Med 89:583–589
Mori K, Misumi A, Sugiyama M, Okabe M, Matsuoka T (1977) Percutaneous transhepatic bile drainage. Ann Surg 185:111–115
Elyaderani MK, Gabriele OF (1980) Brush and forceps biopsy of biliary ducts via percutaneous transhepatic catheterization. Radiology 135:777–778
Rossi M, Cantisani V, Salvatori FM et al (2004) Histologic assessment of biliary obstruction with different percutaneous endoluminal techniques. BMC Med Imaging 4:3
Savader SJ, Prescott CA, Lund GB, Osterman FA (1996) Intraductal biliary biopsy: comparison of three techniques. J Vasc Interv Radiol JVIR 7:743–750
Tapping CR, Byass OR, Cast JEI (2012) Cytological sampling versus forceps biopsy during percutaneous transhepatic biliary drainage and analysis of factors predicting success. Cardiovasc Intervent Radiol 35:883–889
Rossi M, Lemos A, Bonaiuti P et al (1997) Instrumental diagnosis of obstructive jaundice: brushing versus biopsy. Radiol Med (Torino) 93:230–235
Jung G-S, Huh J-D, Lee SU, Han BH, Chang H-K, Cho YD (2002) Bile duct: analysis of percutaneous transluminal forceps biopsy in 130 patients suspected of having malignant biliary obstruction. Radiology 224:725–730
Li T-F, Ren K-W, Han X-W et al (2014) Percutaneous transhepatic cholangiobiopsy to determine the pathological cause of anastomotic stenosis after cholangiojejunostomy for malignant obstructive jaundice. Clin Radiol 69:13–17
Kitajima Y, Ohara H, Nakazawa T et al (2007) Usefulness of transpapillary bile duct brushing cytology and forceps biopsy for improved diagnosis in patients with biliary strictures. J Gastroenterol Hepatol 22:1615–1620
Owens D (1998) Interpretation of cost-effectiveness analyses. J Gen Intern Med 13:716–717
Bland JM, Butland BK. Comparing proportions in overlapping samples. https://www-users.york.ac.uk/~mb55/overlap.pdf. Accessed 1 Jan 2017
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Xing G-S, Geng J-C, Han X-W, Dai J-H, Wu C-Y (2005) Endobiliary brush cytology during percutaneous transhepatic cholangiodrainage in patients with obstructive jaundice. Hepatobiliary Pancreat Dis Int HBPD INT 4:98–103
Yamagami T, Iida S, Kato T, Tanaka O, Nishimura T (2003) Combining fine-needle aspiration and core biopsy under CT fluoroscopy guidance: a better way to treat patients with lung nodules? Am J Roentgenol 180:811–815
Kiranantawat N, Petranovic M, Digumarthy S et al (2015) Clinical role and accuracy of CT-guided percutaneous needle biopsy of cavitary pulmonary lesions. 29 November–4 December 2015, Chicago IL.; archive.rsna.org/2015/15047606.html. Accessed 31 Jan 2016
Li Z, Li T-F, Ren J-Z et al (2016) Value of percutaneous transhepatic cholangiobiopsy for pathologic diagnosis of obstructive jaundice: analysis of 826 cases. Acta Radiol 58:3–9
Song K, Toweill D, Rulyak SJ, Lee SD (2011) Novel jumbo biopsy forceps for surveillance of inflammatory bowel disease: a comparative retrospective assessment. Gastroenterol Res Pract 2011:671659
O’Neill CB, Atoria CL, O’Reilly EM, LaFemina J, Henman MC, Elkin EB (2012) Costs and trends in pancreatic cancer treatment. Cancer 118:5132–5139
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Olga R. Brook.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
One of the authors has significant statistical expertise (Alexander Brook).
Ethical approval
Institutional review board approval was obtained.
Informed consent
Written informed consent was waived by the institutional review board.
Study subjects or cohorts overlap
None of the study subjects or cohorts have been previously reported.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix Table 1
(DOCX 13 kb)
Appendix Table 2
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Boos, J., Yoo, R.J., Steinkeler, J. et al. Fluoroscopic percutaneous brush cytology, forceps biopsy and both in tandem for diagnosis of malignant biliary obstruction. Eur Radiol 28, 522–529 (2018). https://doi.org/10.1007/s00330-017-4987-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4987-5