Abstract
Objectives
To determine resource utilisation according to age and gender-specific subgroups in two large randomized diagnostic trials.
Methods
We pooled patient-specific data from ACRIN-PA 4005 and ROMICAT II that enrolled subjects with acute chest pain at 14 US sites. Subjects were randomized between a standard work-up and a pathway utilizing cardiac computed tomography angiography (CCTA) and followed for the occurrence of acute coronary syndrome (ACS) and resource utilisation during index hospitalisation and 1-month follow-up. Study endpoints included diagnostic accuracy of CCTA for the detection of ACS as well as resource utilisation.
Results
Among 1240 patients who underwent CCTA, negative predictive value of CCTA to rule out ACS remained very high (≥99.4%). The proportion of patients undergoing additional diagnostic testing and cost increased with age for both sexes (p < 0.001), and was higher in men as compared to women older than 60 years (43.1% vs. 23.4% and $4559 ± 3382 vs. $3179 ± 2562, p < 0.01; respectively). Cost to rule out ACS was higher in men (p < 0.001) and significantly higher for patients older than 60 years ($2860–5935 in men, p < 0.001).
Conclusions
CCTA strategy in patients with acute chest pain results in varying resource utilisation according to age and gender-specific subgroups, mandating improved selection for advanced imaging.
Key Points
• In this analysis, CAD and ACS increased with age and male gender.
• CCTA in patients with acute chest pain results in varying resource utilisation.
• Significant increase of diagnostic testing and cost with age for both sexes.
• Cost to rule out ACS is higher in men and patients >60 years.
• Improved selection of subjects for cardiac CTA result in more resource-driven implementation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac computed tomography angiography (CCTA) is an alternative strategy to functional testing in patients with acute and stable chest pain and suspected coronary artery disease (CAD) [1]. There is strong evidence from large, multicentre randomized trials demonstrating that implementation of computed tomography angiography (CTA) in the diagnostic work-up of patients with acute chest pain results in shorter time to diagnosis and reduced length of hospitalisation without missed acute coronary syndrome (ACS) [1, 2]. However, these trials were not adequately powered to detect any effect of cardiac CTA on health outcomes or to demonstrate whether the observed increased rate of downstream testing. In addition, the efficiency of cardiac CTA may vary with age and gender given that differences in the usefulness of functional and anatomic testing have been reported [3].
Cost-effectiveness analysis is one way to determine clinical utility; however, an alternative is to determine efficiency based on an intention to diagnose analysis, similar to an intention to treat analysis for medical therapy [4].
To assess the efficiency and effectiveness of cardiac CTA strategy in age and gender strata, we pooled individual patient data from two large randomized comparative effectiveness trials in patients with acute chest pain.
Material and methods
Population
This study includes subjects from the two largest prospective randomized diagnostic trials that enrolled subjects who presented with acute chest pain but with inconclusive initial evaluation in the emergency department (ED) (NCT01084239; NCT00933400), the details of which have been published previously [1, 2]. In total, subjects were recruited at 14 hospitals [five [1] and nine [2] hospitals in the USA] from 2009 to 2011 [1] and from 2010 to 2012 [2]. All subjects were randomized to either a standard diagnostic strategy or a diagnostic strategy incorporating cardiac CTA for initial evaluation. Only patients that underwent CTA and were available for analysis were included. Studies were approved by local institutional review boards and were HIPAA-compliant, and all participants provided written informed consent.
Briefly, subjects were eligible if they were 30 years or older (40–74 years of age in [2]), presented to the ED with chest pain or anginal equivalent suggestive of myocardial ischaemia, and if further risk stratification for excluding acute coronary syndrome was warranted as determined by the attending physician. All subjects were at low to intermediate risk owing to a non-diagnostic electrocardiogram (ECG) and negative initial troponin test [thrombolysis in myocardial infarction (TIMI) risk score of 0 to 2 [2]] at initial presentation. Major exclusion criteria were mainly computed tomography (CT) related, including impaired renal function (>1.5 mg/dL serum creatinine), known allergy to iodinated contrast agent, clinically unstable condition or non-sinus rhythm.
Study protocol
Upon enrolment, subjects were randomized using a two-to-one [1] or one-to-one [2] strategy, which included a standard diagnostic strategy established at study sites or a strategy utilizing cardiac CTA for initial evaluation. Results of the cardiac CTA were provided to caregiving physicians in real-time and taken into account for clinical decision-making, which included early discharge of patients. All hospital tests and procedures were monitored and final diagnosis was collected. Different safety measures were applied in order to avoid unsafe discharge of patients with undetected ACS, including a second troponin test in patients who were discharged early (within 90–180 min after arrival at the ED [1]), or an early follow-up phone call within 72 h following discharge [2].
Follow-up was performed at least 4 weeks (28 days [2] or 30 days [1], respectively) after enrolment to determine patient safety outcomes. The follow-up telephone call comprised collection of information on repeat visits to the ED or hospitalisation for recurrent chest pain (including diagnostic testing, intervention and clinical events during follow-up); all potential events were verified by the collection of medical records by an independent clinical event committee.
Cardiac CT angiography and analysis
All study participants underwent cardiac CTA using at least 64-slice technology and standardised protocols according to current guidelines [5].
Results were reported according to the Society of Cardiovascular Computed Tomography guidelines, with the use of the American Heart Association coronary segment model [6]. For the analysis, the presence of stenosis was defined as a luminal narrowing of at least 50% in at least one of the 17 coronary segments. If image quality did not permit definite exclusion of the presence of a significant stenosis (because of the presence of motion artefacts, calcification or low contrast-to-noise ratio), the segment was classified as inconclusive. For clinical applicability of the analysis, inconclusive segments were counted as positives for the determination of test characteristics of cardiac CTA. Conversely, plaque was defined as being intraluminal, plaque presence was defined as presence of luminal narrowing less than 50% and no plaque was defined by the absence of any intraluminal plaque on a per patient basis.
Clinical covariates
Demographic variables were collected prospectively and presence of risk factors was established from actual measurements obtained during the hospitalisation and as defined elsewhere [1, 2]. Because age and gender are the most easily obtainable independent predictors and effect modifiers for both ACS and CAD [7,8,9], analysis was performed in age (<50, 50–60, and >60) and gender-specific strata, providing sufficient sample size in each of the age groups.
Test utilisation and costs
Resource utilisation was defined as any additional diagnostic testing (exercise treadmill testing, nuclear stress myocardial perfusion imaging, stress echocardiography or invasive coronary angiography) or coronary revascularisation (percutaneous coronary intervention or coronary artery bypass grafting (CABG)) from the index assessment in the ED to follow-up at 28 or 30 days, and it included resources used during outpatient visits, repeat visits to the ED or hospitalisation for recurrent chest pain. Costs were defined with respect to payer cost. Health care costs during the index care episode were available for ROMICAT II patients only. For these patients, costs were assessed from reports from hospital cost-accounting systems and physician billing records. Costs were adjusted to 2011 US dollars. A multiple linear regression model with total cost as outcome variable and detailed diagnostic test and intervention data as independent variables was used to estimate the costs for ACRIN-PA 4005 patients. Diagnostic cost of care included costs for functional testing and invasive coronary angiography as well as ED and observational unit costs. Total cost of care further included costs for percutaneous coronary interventions and CABG as well as hospitalisation costs. The costs regarding the intention to diagnose ACS were calculated as the following ratio: diagnostic cost of care divided by the number of ACS. Similarly, the costs regarding the intention to rule out ACS were calculated as the following ratio: diagnostic cost divided by the number of non-ACS patients. Costs are in US dollars.
Study endpoints
The primary endpoint of this analysis was diagnostic accuracy for detection of ACS during the index hospitalisation per age and gender strata. ACS was defined as myocardial infarction or objective confirmation of unstable angina (reversible ischaemia on provocative testing or coronary angiography indicating stenosis of 70% or more in a coronary artery) as verified by an independent adjudication committee [10]. Secondary endpoints included prevalence of ACS and at least 50% stenosis on CTA as well as resource utilisation and costs by age and gender strata, specifically overall costs and costs for intention to diagnose ACS.
Methods of data pooling
For data pooling, all patient-level source data from the two trials were combined by an independent statistical core. Definitions of all core variables with respect to CT findings, outcomes and risk categories were identical and no modifications were required.
Statistical analysis
All statistical analyses were performed by an independent data-coordinating centre. Continuous variables are presented as means ± standard deviations and medians with interquartile ranges. Comparisons between groups were performed with the use of an independent sample t test for continuous variables, Fisher’s exact test for categorical variables and the Wilcoxon rank-sum test for ordinal variables.
For each stratum, the prevalence of ACS and conventional measures of diagnostic accuracy [sensitivity, specificity, positive and negative predictive value (PPV and NPV, respectively), including 95% confidence intervals using the exact binominal distribution] were determined. Pretest probability of ACS was defined as the prevalence of ACS within the strata.
A two-sided P value of less than 0.05 was considered to indicate statistical significance. All analyses were performed using Stata (Version 13.1 StataCorp LP, College Station, TX, USA).
Results
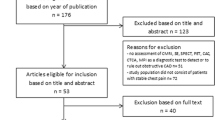
Among the 2370 patients enrolled in the two trials, all subjects randomized to the standard of care arms as well as subjects in whom no CTA findings were available were excluded from the study (n = 961 and n = 169; respectively, Fig. 1). Thus, 1240 study participants in the CTA arm formed the analysis cohort.
Baseline characteristics of the predominantly middle-aged study population (mean age 51.0 ± 8.9, 50.6% male) are provided in Table 1. There were differences between the two cohorts with respect to age, dyslipidaemia and TIMI score. After complete diagnostic evaluation, 68 patients (5.5%) had a final diagnosis of ACS: nine patients with myocardial infarction and 59 with unstable angina (0.7% and 4.8%, respectively). There were significant differences in ACS rates between men and women (p < 0.05) as well as with respect to age (p < 0.05). All subsequent analysis was stratified by age and gender.
Prevalence of findings and outcomes
Both CT findings and ACS rates varied significantly between age groups and gender. Both rates of CT-positive findings and ACS were lower in women by approximately one age category as compared to men (Table 2, Fig. 2).
There was a significant increase in the prevalence of significant stenosis and a more pronounced increase in the presence of any plaque with age for women and men (Table 2, Fig. 2). ACS rates increased with age in both women and men but were lower overall in women than in men (2.5% to 5.4%, p = 0.176 in women in the youngest vs. oldest age group, and 3.1% to 23.2%, p < 0.001 in men in the youngest vs. oldest age group).
Diagnostic accuracy of cardiac CTA
In contrast to the prevalence of findings and outcomes, there was no difference in the high NPV and sensitivity across age groups (at least 99.4%, Table 2). Also, cardiac CTA correctly identified all ACS in women older than 50 years of age (sensitivity 100%), whereas in female subjects younger than 50 years of age one of six cases of ACS was missed (sensitivity 83.3%). A total of one case of ACS was missed in men 50–60 years of age (sensitivity 96%) with none missed in the two other male age groups (Table 2). Both in women and men, the specificity and PPV decreased with age (Table 2). While sensitivity is very high across all ranges of calcium score, specificity decreases with increasing calcium score (for both men and women) (Supplementary Table 1) [12].
Resource utilisation and healthcare costs
Similar to the CT findings and outcomes, there was a significant difference in resource utilisation across age groups with highest utilisation in the oldest male age group (Tables 3 and 4, p < 0.01).
In women, the rate of subjects with additional testing increased with age (10.7% vs. 23.4% (p < 0.01) for the youngest vs. oldest female age group, respectively). Similarly, the rate of invasive coronary angiography and interventions was highest in the oldest female age group (8.1% and 4.5%, respectively). Likewise in men, the rate of subjects with additional testing increased with age (12.8% vs. 43.4% (p < 0.001) for the youngest vs. oldest male age group, respectively) with the rate of invasive coronary angiography and interventions being highest in the oldest male age group at 21.7% and 11.6%, respectively.
The increase in invasive coronary angiographies with increasing age is significant for both groups, i.e. men (p < 0.001) and women (p = 0.026). Overall 37/81 (45.7%) of coronary angiographies were followed by PCI and 5/81 (6.2%) were followed by CABG. Coronary angiographies followed in 74/231 (32.0%) of patients that had a positive CTA scan leading to 41/231 (17.8%) revascularisation (37 PCI, 4 CABG).
The mean total cost of care (US$) was 3334 ± 4538 with the diagnostic cost of care (US$) accounting for nearly 90% (2955 ± 2353) of the total. The diagnostic costs of care were significantly higher in men than in women (3242 ± 2749 vs. 2661 ± 1817; p < 0.001) and increased with age for both women and men (Tables 3 and 4, Fig. 3). However, the proportion of diagnostic costs to the total cost of care decreased with increasing age. On average the proportion was lower in men as compared with women (0.85 vs. 0.94, p < 0.001). Similarly, the prevalence of ACS and the prevalence of plaque on CT were predictive of increased costs (β: US$4407 per 1% increase in prevalence of ACS, p = 0.037, and β: US$1894 per 1% increase in prevalence of plaque on CT, p = 0.026; respectively).
Costs and prevalence of negative findings by age and gender. Relationship of the prevalence of negative finding on CT (% negative CT, absence of at least 50% stenosis) and diagnostic costs according to age groups for men (a) and women (b). Diagnostic costs are illustrated as total diagnostic costs ($$ diagnostic), costs to diagnose one ACS ($$ to diagnose ACS) and costs to rule out ACS ($$ to rule out ACS)
Key drivers of cost were coronary angiographies, which accounted for 16.8% of diagnostic cost, followed by SPECT, which accounted for 5.8% of the diagnostic cost. Much of the diagnostic costs, which are based on a multiple linear ordinary least squares regression approach, are non-specific, i.e. roughly 71% of the cost is due to ED or observational unit costs, medication costs, etc.
In an intention to rule out ACS analysis, the cost to rule out one ACS was higher in men as compared with women ($3528, 95% CI 3229–3828 vs. $2737, 95% CI 2563–2911) and increased significantly with age in women from $2585 to $3360 and in men from $2860 to $5935. Conversely, in an intention to diagnose ACS analysis, the cost to diagnose one ACS was much lower in men as compared to women ($39,918, 95% CI 31,110–48,726 vs. $95,799, 95% CI 53,811–137,788, P < 0.001) and decreased with age in women from $102,548 to $58,803 and in men from $89,242 to $19,661.
Discussion
In this pooled analysis of patient-level data from two large randomised diagnostic trials comparing a CTA strategy with standard of care in patients presenting with acute chest pain to the ED, we demonstrate that increased downstream testing and costs occur with age, these increases are more pronounced in men than in women and are associated with an increase in prevalence of CAD. When put into the perspective of an intention to rule out analysis, the costs to rule out an ACS increase with age and are higher in men compared to women. Conversely, the costs to diagnose an ACS decrease with age and are lower in men as compared to women. Hence, improved selection of patients at very low and high risk of ACS is key to improve efficiency of the management of patients presenting with suspicion of ACS.
Age and gender are well-known predictors of CAD, myocardial infarction and ACS [7,8,9]. We found that the prevalence of at least 50% stenosis on CTA is strongly associated with age in both women and men with rates of significant coronary stenosis increasing from 8.6% in women below 50 years of age to 53.6% in men over 60 years of age. This is mirrored in the increasing rates of ACS among the age and gender categories, ranging from 2.5% to 23.2%. Thus, we extend earlier evidence by Diamond and Forrester that age and gender are useful discriminators in patients with suspected CAD into the setting of acute chest pain [11–13].
It is notable that the prevalence of CT findings and ACS in women trails that in men by approximately 10 years. While our results point out the ability of CTA to exclude disease in women with a significant shortening effect on length of hospitalisation [3], they also raise caution for its application in younger women, as the sensitivity in this age category was as low as 83.3% (36–100%), still resulting in a post-test probability of disease of 0.4%. In the one false negative subject, ACS was detected after hospital admission despite the absence of coronary stenosis on CT, presumably because of transient ischaemia caused by vasospasm or thrombus, or because of endothelial dysfunction or microvascular disease particularly in women, representing a limitation of cardiac CT [14, 15]. It is important to note that in our cohort of 1240 patients, there were two patients with ACS that had no detectable coronary stenosis of at least 50%. However, both subjects had non-obstructive plaque on CCTA, which may also reflect the limitations of the arbitrary threshold of 50% for the definition of obstructive stenosis and less than 50% defined as non-obstructive plaque. However, these cases may also represent the clinical scenario of ACS occurring in subjects without coronary stenosis [16].
Three large multicentre trials have demonstrated that cardiac CT is an effective and safe alternative strategy to functional testing for evaluation of patients with acute chest pain. However, these trials also reported increased downstream resource utilisation and costs, particularly an increased number of invasive angiograms as compared to standard of care (5–12% for CTA vs. 4–8% for SOC) [1, 2, 17]. Similar observations were made in a recent meta-analysis summarising 1869 patients randomised to CTA arms and 1397 to SOC arms [18]. We expand on these prior reports by providing a pooled analysis of patient-level data from two large randomised diagnostic trials, allowing insight into the efficiency of a cardiac CTA strategy including downstream testing and costs stratified by gender and age.
We further extend earlier work on resource utilisation by using cost to rule out and cost to diagnose ACS as relative measures of cost-effectiveness, evaluating total costs from the perspective of risk to suffer an adverse outcome (ACS). These analyses suggest that resource utilisation and costs are higher in older age groups and men because of the higher prevalence of ACS. From an ED perspective, the intention to rule out analysis is the more clinically relevant measure and demonstrates that implementing CT in the work-up of patients over 60 years of age results in significantly higher costs as compared with younger patients ($2860 to $5935 in men, p < 0.001). From a diagnostic point of view, the intention to diagnose analysis indicates that resource utilisation may be more effective in higher risk populations as the prevalence of ACS increases more than the downstream testing and costs, resulting in a lower cost to diagnose ACS ratio (women: <50 years of age $102,548 vs. >60 years of age $58,803; men: <50 years of age $89,242 vs. >60 years of age $19,661). Hence, these data suggest that resources are relatively well spent according to risk of the patients with more resources being devoted to higher risk groups.
There is probably broad agreement among caregivers that not all patients currently undergoing diagnostic testing need advanced imaging, and clinical practice may simply reflect the lack of potent risk stratification tools. Recent data suggest that highly sensitive troponin assays may facilitate improved patient selection and improve resource utilisation [19]. Additionally, the low yield of catheterisation lab referrals after cardiac CTA also needs to be addressed (a maximum of 21.7% in men over 60 years of age). Forthcoming data suggest that functional information, for example, provided by CT-based determination of fractional flow reserve may serve as a gatekeeper and decrease the number of catheterisation referrals significantly [20], thereby further increasing the efficiency.
The study has several notable limitations. Our analysis is limited to the CT arms of the two mother trials. While this may have prevented a direct comparison to the standard of care in these patients, it allows for detailed analysis of CT-derived information on CAD and costs. Despite combining data from the two largest randomised diagnostic trials, the numbers of observations and outcomes in the single categories are still limited, which did not allow for performing more detailed subanalysis, e.g. with respect to smaller age categories. However, this represents the largest effort to date and serves as a basis for more detailed and focused analysis to be pursued in future trials. In addition, there was significant heterogeneity between the two source trials with respect to patient risk (Table 1) which may limit specific pooling validity. However, by combining the trials, we achieved a more generalizable patient population, also representing different SOC at two large sites. Lastly, we did not stratify our analysis by plaque composition, which was not assessed specifically in the source trials. Further research will need to specifically determine the role of plaque composition in the diagnostic work-up of these patients.
Conclusions
This patient-level pooled analysis of the cardiac CTA arms of two large randomised trials demonstrates that downstream testing, resource utilisation and costs increase with age in both men and women because of higher prevalence of positive CTA findings. Hence, besides adequate preparation and scanning, improved selection of patients is key to improving efficiency of the management of patients presenting with suspicion of ACS.
Abbreviations
- ACS:
-
Acute coronary syndrome
- CABG:
-
Coronary artery bypass graft
- CAD:
-
Coronary artery disease
- CCTA:
-
Cardiac computed tomography angiography
- CT:
-
Computed tomography
- CTA:
-
Computed tomography angiography
- ECG:
-
Electrocardiogram
- ED:
-
Emergency department
- NPV:
-
Negative predictive value
- PCI:
-
Percutaneous coronary intervention
- PPV:
-
Positive predictive value
- SD:
-
Standard deviation
- SOC:
-
Standard of care
- TIMI:
-
Thrombolysis in myocardial infarction
References
Litt HI, Gatsonis C, Snyder B et al (2012) CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med 366:1393–1403
Hoffmann U, Truong QA, Schoenfeld DA et al (2012) Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 367:299–308
Truong QA, Hayden D, Woodard PK et al (2013) Sex differences in the effectiveness of early coronary computed tomographic angiography compared with standard emergency department evaluation for acute chest pain: the rule-out myocardial infarction with Computer-Assisted Tomography (ROMICAT)-II Trial. Circulation 127:2494–2502
Gold MR, Siegel JE, Russell LB, Weinstein MC (eds) (1996) Cost-effectiveness in health and medicine. Oxford University Press, New York
Taylor AJ, Cerqueira M, Hodgson JM et al (2010) ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use criteria for cardiac computed tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Circulation 122:e525–e555
Leipsic J, Abbara S, Achenbach S et al (2014) SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 8:342–358
Morise AP, Haddad WJ, Beckner D (1997) Development and validation of a clinical score to estimate the probability of coronary artery disease in men and women presenting with suspected coronary disease. Am J Med 102:350–356
Kasser IS, Bruce RA (1969) Comparative effects of aging and coronary heart disease on submaximal and maximal exercise. Circulation 39:759–774
Ho KT, Miller TD, Hodge DO, Bailey KR, Gibbons RJ (2002) Use of a simple clinical score to predict prognosis of patients with normal or mildly abnormal resting electrocardiographic findings undergoing evaluation for coronary artery disease. Mayo Clin Proc 77:515–521
Hollander JE, Blomkalns AL, Brogan GX et al (2004) standardised reporting guidelines for studies evaluating risk stratification of emergency department patients with potential acute coronary syndromes. Ann Emerg Med 44:589–598
Diamond GA, Forrester JS (1979) Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 300:1350-1358
Chaitman BR, Rosen AD, Williams DO et al (1997) Myocardial infarction and cardiac mortality in the Bypass Angioplasty revascularisation Investigation (BARI) randomised trial. Circulation 96:2162–2170
Gibbons RJ, Chatterjee K, Daley J et al (1999) ACC/AHA/ACP-ASIM guidelines for the management of patients with chronic stable angina: executive summary and recommendations. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Chronic Stable Angina). Circulation 99:2829–2848
Kaski JC (2004) Pathophysiology and management of patients with chest pain and normal coronary arteriograms (cardiac syndrome X). Circulation 109:568–572
Bugiardini R, Bairey Merz CN (2005) Angina with "normal" coronary arteries: a changing philosophy. JAMA 293:477–484
Hoffmann U, Nagurney JT, Moselewski F et al (2006) Coronary multidetector computed tomography in the assessment of patients with acute chest pain. Circulation 114:2251–2260
Goldstein JA, Chinnaiyan KM, Abidov A et al (2011) The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 58:1414–1422
Hulten E, Pickett C, Bittencourt MS et al (2013) Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and meta-analysis of randomised, controlled trials. J Am Coll Cardiol 61:880–892
Ferencik M, Liu T, Mayrhofer T et al (2015) hs-Troponin I followed by CT angiography improves acute coronary syndrome risk stratification accuracy and work-up in acute chest pain patients: results from ROMICAT II trial. J Am Coll Cardiol Img 8:1272–1281
Douglas PS, Pontone G, Hlatky MA et al (2015) Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 36:3359–3367
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Udo Hoffmann, Department of Emergency Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
This study has received funding by:
ACRIN PA 4005 Funding: NIH, Supported by the Commonwealth of Pennsylvania Department of Health (SAP4100042725) and the American College of Radiology Imaging Network Foundation/ACR Imaging Core Lab.
ROMICAT II Funding: National Heart, Lung, and Blood Institute (U01HL092040 and U01HL092022) and the National Institutes of Health (UL1RR025758, K23HL098370, and L30HL093896, to Dr. Truong)
Additional Funding: K24HL113128 for Drs. Mayrhofer, Ferencik, Bittner, and Mr. Hallett; T32HL076136 for Dr. Janjua.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously published (Litt et al, NEJM 2012 and Hoffmann et al., NEJM 2012).
Methodology
• prospective
• randomised controlled trial
• multicentre study
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOCX 101 kb)
Rights and permissions
About this article
Cite this article
Bamberg, F., Mayrhofer, T., Ferencik, M. et al. Age- and sex-based resource utilisation and costs in patients with acute chest pain undergoing cardiac CT angiography: pooled evidence from ROMICAT II and ACRIN-PA trials. Eur Radiol 28, 851–860 (2018). https://doi.org/10.1007/s00330-017-4981-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4981-y