Abstract
Objectives
We aimed to evaluate the prognostic role of cardiac magnetic resonance imaging (CMR)–based extracellular volume fraction (ECV) in patients with non-ischemic dilated cardiomyopathy (NIDCM) and compare it with late gadolinium enhancement (LGE) parameters.
Methods
This was a single-center, prospective, cohort study of 117 NIDCM patients (71 men, 51.9 ± 16.7 years) who underwent clinical 3.0-T CMR. Myocardial ECV and LGE were quantified on the left ventricular myocardium. The presence of midwall LGE was also detected. Nineteen healthy subjects served as controls. The primary end points were cardiovascular (CV) events defined by CV death, rehospitalization due to heart failure, and heart transplantation.
Results
During the follow-up period (median duration, 11.2 months; 25th–75th percentile, 7.8–21.9 months), the primary end points occurred in 19 patients (16.2%). The ECV (per 3% and 1% increase) was associated with a hazard ratio of 1.80 and 1.22 (95% confidence interval [CI], 1.48–2.20 and 1.14–1.30, respectively; p < 0.001) for the CV events. Multivariable analysis also indicated that ECV was an independent prognostic factor and had a higher prognostic value (Harrell’s c statistic, 0.88) than LGE quantification values (0.77) or midwall LGE (0.80).
Conclusion
CMR-based ECV independently predicts the clinical outcome in NIDCM patients.
Key Points
• T1-mapping–based ECV is a useful parameter of risk stratification in NIDCM
• ECV has a higher prognostic value than LGE
• Contrast-enhanced T1-mapping CMR is a feasible and safe method
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-ischemic dilated cardiomyopathy (NIDCM) is characterized by diffuse intrinsic myocardial remodeling, with reduction in left ventricular systolic function, in the absence of significant coronary artery disease [1]. Myocardial fibrosis, particularly midwall fibrosis, is a characteristic feature of NIDCM [2, 3]. Late gadolinium enhancement (LGE) on cardiac magnetic resonance imaging (CMR) is considered the standard method for detecting focal myocardial fibrosis. Midwall fibrosis, as detected by LGE, is a predictor of adverse cardiovascular (CV) outcomes [1, 4], Although LGE is a powerful imaging tool that can detect focal fibrosis patterns [5], it often fails to detect diffuse myocardial fibrosis [6, 7]. A recently developed T1-mapping sequence can be used to quantitatively characterize the myocardium. The quantification of ECV using CMR can serve as a noninvasive tool for determining diffuse myocardial pathology [6]. However, the prognostic significance of CMR-based ECV remains unclear. We aimed to examine the prognostic role of CMR-based ECV in NIDCM patients and compare this parameter with conventional LGE parameters.
Materials and methods
Study population
This was a single-center prospective, cohort study. The institutional review board approved the study, and written informed consent was obtained from each patient. A total of 447 consecutive patients who underwent T1-mapping CMR from April 1, 2012, to April 30, 2015, were eligible for the study.
Patients with 1) reduced left ventricular ejection fraction (LVEF) ≤40% on CMR without any history of significant coronary artery disease and 2) left ventricular chamber dilatation, defined as an enlarged left ventricular end-diastolic diameter on short-axis view (≥6 cm), were included. A total of 135 patients met the inclusion criteria. Of these, 18 were excluded because of recent myocarditis (n = 7), newly diagnosed significant coronary artery disease (n = 7), and incomplete data sets (n = 4), and, finally, 117 patients were analyzed. All the patients underwent clinical examination, cardiopulmonary exercise test (CPET), routine biochemical analysis including the N-terminal pro-B-type natriuretic peptide, and CMR. Nineteen healthy subjects also underwent CMR. The hematocrit (Hct) levels of the patients and healthy subjects were acquired on the day of CMR.
CMR protocol
CMR was performed using a 3.0-T scanner (Magnetom Trio Tim; Siemens AG Healthcare Sector, Erlangen, Germany), with a six-element body matrix coil and a spine matrix coil array. The localization of the heart was performed with True FISP localizers under electrocardiographic gating. T1 mapping was performed using a modified Look-Locker inversion-recovery sequence at end expiration in three short-axis planes (at the basal, mid, and apical levels). Pre-contrast T1-mapping images were acquired before the intravenous injection of the contrast agent, whereas post-contrast T1-mapping images were acquired 15 min after the injection of the contrast agent (0.2 mmol/kg gadolinium contrast agent, Gadovist; Bayer Schering Pharma AG, Berlin, Germany). LGE magnetic resonance (MR) imaging was performed 10 min after the injection of the contrast agent between the pre- and post-contrast T1-mapping sequences by using a magnitude- and phase-sensitive inversion recovery (PSIR)–prepared True FISP sequence (see the Supplemental Materials for detailed protocols). For T1-mapping imaging, we employed the nonselective inversion pulse True FISP single-shot readout sequence in the mid-diastolic phase, with the following parameters: field of view, 308 × 380 mm; acquisition matrix, 126 × 192; slice thickness, 8 mm; TR, 2.4 ms; TE, 1.0 ms; minimum inversion time, 100 ms; inversion time increment, 80 ms; flip angle, 35°; parallel acquisition technique factor, 2; number of inversions, 3. Three images were acquired after the first inversion; following a pause for three heartbeats, three images were acquired after the second inversion; subsequently, after a pause for three heartbeats, five images were acquired after the third inversion. Fully automated non-rigid motion correction was applied to register the individual TI images before inline T1 fitting was performed using a mono-exponential three-parameter fit.
CPET
A symptom-limited CPET was performed on a treadmill according to the modified Bruce ramp protocol (see the Supplemental Materials for details).
Image analysis
All MR images were analyzed using the cvi42 image analysis software (Circle Cardiovascular Imaging Inc., Calgary, AB, Canada). Two radiologists (Y.J.H. and H.J.L.), with 10 and 12 years of experience in CV image interpretation, respectively, who were blinded to the clinical data, independently analyzed all MR images, and inter-observer reproducibility was assessed.
Functional MR image analysis
Ventricular function was assessed on short-axis cine MR images according to Simpson’s method [8]. The endocardial and epicardial borders of the left ventricle (LV) and the endocardial border of the right ventricular (RV) wall were delineated manually on the end-diastolic and end-systolic images, from which the papillary muscles and trabeculations were excluded.
Quantification of native T1 and ECV
The endocardial and epicardial borders of the LV were drawn, and the RV insertion sites were delineated manually. A round region of interest (ROI) >10 mm2 that excluded the papillary muscle was also drawn manually on the LV blood cavity, and the pre- (native) and post-contrast T1 values on 16 segments of the LV (except for the apex segment) and blood cavity were measured. The myocardial ECV was calculated using the following equation [9]:
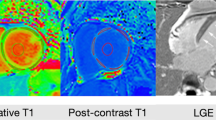
The global native T1 and ECV values of LV (mean values of the 16 segments) were recorded (Fig. 1).
Representative case of T1 mapping and late gadolinium enhancement (LGE) image analysis of the mid-left ventricle (LV) in a patient. (A and B) On pre-contrast (A) and post-contrast (B) T1-mapping images, segmental-based regions of interest (ROI) on the myocardium and a round ROI on the blood cavity were drawn to measure the native and post-T1 values of myocardium and blood cavity. (C and D) Reported global native T1 was 1227.8 ms and ECV 29.7% on native T1 (C) and ECV maps (D). (E) On the LGE image, LGE was noted on the mid-ventricular septum. (F) The extent of LGE was automatically calculated by adopting the 5-standard deviation method. The quantified LGE was 17%
Quantification of LGE
The presence of LGE was first visually determined, and the pattern was analyzed in cases where LGE was detected. In short-axis LGE images, the endocardial and epicardial borders of the LV were drawn manually and the extent of LGE (%) was automatically quantified by adopting the 5-standard deviation (SD) method [10] (Fig. 1).
Clinical outcome and follow-up duration
The primary end points of clinical outcome were CV events defined by CV death, rehospitalization due to heart failure, and heart transplantation. The follow-up duration was computed from the date of CMR examination to the last visit to the hospital or the occurrence of the first CV event.
Statistical analysis
The categorical baseline characteristics were expressed as numbers and percentages, whereas the continuous variables were expressed as means and SDs. The Shapiro-Wilk test was used to evaluate normal distributions. Statistical tests were two-sided, and p < 0.05 was considered significant. The chi square or Fisher’s exact test (if the sample size was <5) was used to compare the categorical variables, and Student’s t test was used to compare the continuous variables. With regard to survival analysis, we used the log rank test with Kaplan-Meier curves and Cox proportional hazards regression to obtain hazard ratios (HRs) and 95% confidence intervals (CIs). The proportional hazards assumptions were assessed graphically using Schoenfeld residual plots. Univariable Cox regression analysis was used to determine the association of clinical and CMR parameters, such as native T1, ECV, and LGE quantification values, with the occurrence of a composite event. Variables with a p value <0.05 on univariable analysis were included in the multivariable Cox regression analysis. The variance inflation factor (VIF) was used to assess multicollinearity for the multivariable analyses, with VIF > 10 indicating multicollinearity. The HRs for ECV were expressed in 1% and 3% increments (reflecting the 95% CI for repeated measurement, ±1.4%) [11, 12].
The predictive accuracy of the Cox regression model was evaluated by Harrell’s c statistic. The best ECV threshold for predicting the composite event was estimated via the smoothed restricted cubic spline method. This method was used to produce the flexible log HR curve vs. ECV, which facilitates the visual exploration of the relationships between ECV and the clinical outcomes. With regard to inter-observer reproducibility, the images were analyzed independently using intra-class correlation coefficients (ICCs). Statistical analyses were performed using the R statistical software version 3.2.3 (R Foundation, Vienna, Austria) and SPSS version 20 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
The final study population comprised 117 NIDCM patients (71 men, 51.9 ± 16.7 years). The clinical characteristics of the healthy subjects and the entire patient population are described in Table 1.
CMR
The CMR data of the healthy subjects and the entire patient population are also provided in Table 1.
T1-mapping data
NIDCM patients showed significantly higher global native T1 and ECV values compared with controls (p < 0.001, Table 1). Patients with clinical outcomes showed significantly higher global native T1 and ECV values as compared to patients without any CV events (p < 0.001, Table 1) (see the Supplemental Materials for the analysis of regional difference in T1-mapping parameters). The inter-observer agreements were excellent, with ICCs of 0.969 (95% CI, 0.949–0.982) for native T1 values, 0.992 (95% CI, 0.987–0.995) for post-contrast T1 values, and 0.905 (95% CI, 0.843–0.943) for ECV values.
LGE analysis
With regard to LGE, 82 (70.1%) NIDCM patients exhibited myocardial LGE, whereas 35 (29.9%) patients did not exhibit any LGE. Among the 82 patients with LGE, 63 (53.8%) exhibited LGE at the midwall and 19 (16.2%) exhibited other LGE patterns. Both the LGE (+) and LGE (−) groups showed higher native T1 and ECV values (LGE (+) group, 1328.5 ± 83.5 ms and 32.7% ± 5.5%; LGE (−) group, 1321.3 ± 105.4 ms and 30.3% ± 5.7%) as compared with the control group (p < 0.05, Table 1). Patients with CV events showed a significantly higher incidence of midwall LGE as well as higher LGE quantification values as compared to patients without CV events (p < 0.05, Table 1).
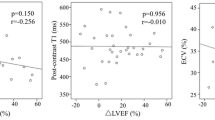
Correlations between the global ECV and other imaging and functional variables
The global ECV was well correlated with both midwall LGE (r = 0.45, p < 0.001) and LGE quantification values (r = 0.34, p < 0.001). Moreover, ECV was also significantly correlated with the clinical functional variables such as LVEF (r = −0.25, p < 0.01) and peak VO2 (r = −0.28, p = 0.03). However, the ECV values were not correlated with the left ventricular end-diastolic volume/body surface area (BSA) ratio (p = 0.26) or with the left ventricular end-systolic volume/BSA ratio (p = 0.08).
Survival analysis
During the follow-up period (median, 11.2 months; 25th–75th percentile, 7.8–21.9 months), the CV events were observed in 19 patients (16.2%), including CV death in 4, rehospitalization due to heart failure in 10, and heart transplantation in 5. Univariable Cox regression analysis indicated that, among the clinical variables, heart rate, beta-blocker medication, and peak VO2 were associated with clinical outcomes. Among the imaging parameters, LVEF and RVEF were associated with clinical outcomes (Table 2). The native T1, LGE quantification values, and the presence of midwall LGE predicted the clinical outcome, with an HR of 1.01 (95% CI, 1.00–1.01; p = 0.03), 1.04 (95% CI, 1.01–1.08; p < 0.001), and 4.89 (95% CI, 1.43–16.80; p = 0.01) (Fig. 2), respectively. A 3% increase or 1% increase in the ECV was associated with an HR of 1.80 and 1.22, respectively (95% CI, 1.48–2.20, 1.14–1.30; p < 0.001), for the CV events. Harrell’s c statistic for ECV (per 1 or 3% increase) was 0.87, which was higher than that for LGE and the other variables (0.71 for midwall LGE and 0.69 for LGE quantification values; Table 2). Even after adjusting for clinical variables, such as heart rate, peak VO2, and beta-blocker medication, and imaging parameters, including LVEF and RVEF, the multivariable Cox regression analysis indicated that increased ECV remained independently associated with adverse clinical outcomes. There was no multicollinearity between adjusted parameters in a multivariable analysis. When adjusting for clinical variables alone, ECV (3% increase) was found to be an independent prognostic factor (HR, 1.66; 95% CI, 1.26–2.18; p < 0.001), with a higher Harrell’s c statistic (0.86). Moreover, when adjusting for imaging parameters alone, ECV (3% increase) was found to be an independent prognostic factor (HR, 1.69; 95% CI, 1.34–2.14; p < 0.001), with a higher Harrell’s c statistic (0.88) than that for native T1 and LGE quantification values and midwall LGE. The native T1 values were not found to be an independent factor in multivariable analysis, whereas midwall LGE was found to be an independent predictor only after adjusting for the imaging variables. In contrast, ECV consistently showed the highest Harrell’s c statistic in all models (Table 3). The Kaplan-Meier survival curve according to the tertiles of ECV (1st tertile, 28.8; 2nd tertile, 33.8) is demonstrated in Fig. 3 (ECV 1st tertile vs. 2nd tertile; p = 0.16; 1st tertile vs. 3rd tertile; p < 0.001; 2nd tertile vs. 3rd tertile; p < 0.001). In a smoothed restricted cubic spline plot of the HR and ECV, the HR generally linearly increases as the ECV increases. In particular, with a cutoff value of 31.1% (HR = 1), the probability of adverse clinical outcomes becomes high as ECV increases, until ECV reaches a value of 42.5%. The overall association between ECV and the clinical outcome was significant (p < 0.001; Fig. 4). The higher ECV group showed poorer clinical outcome than the lower ECV group (clinical outcome rate: 3.8% vs. 26.2%; p < 0.001).
Kaplan-Meier curve according to the tertiles of the extracellular volume fraction (ECV) (1st tertile, 28.8; 2nd tertile, 33.8) and cardiovascular outcome. Patients with elevated ECV values (≥1st and 2nd tertiles) experienced significantly higher adverse clinical outcomes than patients with ECV values lower than the 3rd tertile
Smoothed restricted cubic spline plot of the hazard ratio (HR) and the extracellular volume fraction (ECV). The full line represents the logarithmic change of the HR from the ECV, and the dotted line shows its 95% confidence interval. The HR generally linearly increases as ECV increases. In particular, with a cutoff value of 31.1% (HR = 1), the probability of adverse clinical outcomes increases as ECV increases, until the ECV reaches 42.5%. The overall association between ECV and the clinical outcome was significant
Discussion
In the present study, we aimed to determine whether CMR-based ECV has an independent or incremental prognostic value in NIDCM patients. We found that global ECV independently predicts the clinical outcome and the prognostic value of ECV was higher than that of the native T1 or LGE quantification values.
Risk stratification of NIDCM patients has been challenging because they have a wide variety of clinical outcomes. Contrast-enhanced T1-mapping–based ECV may play an important role in the proper estimation of prognosis of NIDCM patients. This might be helpful for patients and clinicians in deciding the appropriate type and timing of advanced heart failure therapies such as heart transplantation and left ventricular assist devices.
CMR imaging has become a widely available diagnostic tool in visualizing myocardial scar, fibrosis, and non-ischemic cardiomyopathies [4].
LGE is a well-established gold standard method in detecting focal myocardial fibrosis, and the prognostic value of LGE in NIDCM is well known [4, 13]. In a previous study, the detection of midwall fibrosis with LGE was associated with an HR of 3.1 (95% CI, 1.1–8.5; p = 0.03). In cases of NIDCM, midwall fibrosis on CMR can serve as a predictor of the combined end point of all-cause mortality and CV hospitalization [4]. We also observed that midwall LGE and LGE quantification values have a prognostic value in NIDCM patients.
However, LGE has certain limitations in detecting diffuse myocardial remodeling. In the present study, 35 (29.9%) of 117 patients did not have detectable LGE. However, the native T1 and ECV values were significantly higher in these patients than in the control groups (p < 0.05) and were negatively correlated with the EF. These findings suggest that native T1 and ECV values can help detect and quantify diffuse myocardial changes, which cannot be detected by LGE [7, 14, 15]. T1 mapping is an emerging CMR technique that can provide a quantitative assessment of tissue characterization in NIDCM patients [16]. In NIDCM, the native T1 can quantitatively characterize diffuse myocardial abnormalities, particularly diffuse fibrosis, which is not apparent on LGE images, with a high diagnostic value (sensitivity, 100%; specificity, 96%; area under the curve, 0.99) without the need for gadolinium contrast agents [17]. ECV estimated using CMR can also identify NIDCM with a high diagnostic value (specificity, 91%; sensitivity, 62%); in fact, it has been validated in many studies as a robust marker reflecting the degree of myocardial fibrosis in NIDCM [11, 18–20].
A few recent studies have evaluated the prognostic role of T1-mapping CMR [21–24]. Kammerlander et al. [22] demonstrated that significantly higher event rates were observed in patients with higher ECV (log rank p < 0.01). In the multivariable Cox regression analysis, ECV was independently associated with the clinical outcome (p < 0.01) but was not found to be a significant factor after adjusting for clinical parameters. Puntmann et al. [23] demonstrated that native T1 was the sole independent predictor of all-cause mortality and heart failure (HR, 1.1; 95% CI, 1.06–1.15) in their large multicenter study. In previous studies, ECV was evaluated only in the mid-ventricular septum in a single slice [23] or in non-infarcted myocardium [22, 24]. We have evaluated the ECV value from all segments of the LV myocardium, and found that it demonstrated independent prognostic efficacy in consecutively enrolled NIDCM patients. Clinically important variables such as heart rate, comorbidities, CPET parameters, and various heart failure medications were analyzed in the present study. Even after adjusting for clinically important variables including heart rate, peak VO2, and beta-blocker usage, as well as imaging parameters, we found that ECV (per 1% and 3% increase) was independently associated with clinical outcomes and consistently showed the highest prognostic power among the other parameters. When a cubic spline plot of the log HR was used, we found that if the ECV was higher than 31.1%, the HR of the ECV increased according to the ECV values, until the ECV reached 42.5%. The overall association between ECV and clinical outcome was significant (p < 0.001). Moreover, myocardial ECV was significantly associated with LV dysfunction, LVEF, and peak VO2. CMR-based ECV provides an objective and standardized measure of myocardial fibrosis, and it is also a useful measure in NIDCM patients with LGE limitations. We have shown that contrast-enhanced T1-mapping CMR is a clinically feasible and effective imaging modality providing independent prognosis in NIDCM patients with a wide variety of clinical outcomes.
The present study has several potential limitations. The relatively small sample size and low event rate were the major limitations of our study. The low event rate prohibited the use of all the significant variables in the multivariable analysis; accordingly, only three variables were included. The lack of follow-up CMR, particularly in patients with reverse remodeling who have been clinically recovered, was another limitation of our study. Finally, the examined subjects included NIDCM patients with a low EF. Hence, the generalizability of the current findings to other populations is unknown. However, we evaluated the prognostic value of CMR-based ECV in consecutively enrolled homogenous NIDCM patients. The quantified ECV values were reliable because all the scans were performed with the same scanner under the same conditions, and the patients’ Hct values were acquired on the day of CMR. In addition to the imaging parameters, important clinical variables such as peak VO2 were adjusted for in the multivariable analysis. Thus, the quantification of ECV using CMR could serve as a noninvasive tool for quantifying diffuse myocardial abnormalities and risk stratification in NIDCM patients [6].
In conclusion, ECV determined by CMR is a predictor of combined CV death, rehospitalization, or heart transplantation, independent of ventricular remodeling or the clinical characteristics of NIDCM patients.
Abbreviations
- BMI:
-
body mass index
- BSA:
-
body surface area
- CI:
-
confidence interval
- CMR:
-
cardiac magnetic resonance imaging
- CPET:
-
cardiopulmonary exercise test
- CV:
-
cardiovascular
- ECV:
-
extracellular volume fraction
- EDV:
-
end-diastolic volume
- EF:
-
ejection fraction
- ESV:
-
end-systolic volume
- Hct:
-
hematocrit
- HR:
-
hazard ratio
- ICC:
-
intra-class correlation coefficient
- LGE:
-
late gadolinium enhancement
- LV:
-
left ventricle
- NIDCM:
-
non-ischemic dilated cardiomyopathy
- ROI:
-
region of interest
- RV:
-
right ventricle
- SD:
-
standard deviation
- SV:
-
stroke volume
- VIF:
-
variance inflation factor
References
Kuruvilla S, Adenaw N, Katwal AB, Lipinski MJ, Kramer CM, Salerno M (2014) Late gadolinium enhancement on cardiac magnetic resonance predicts adverse cardiovascular outcomes in nonischemic cardiomyopathy: a systematic review and meta-analysis. Circ Cardiovasc Imaging 7:250–258
Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S et al (2013) Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. Jama 309:896–908
Lehrke S, Lossnitzer D, Schob M, Steen H, Merten C, Kemmling H et al (2011) Use of cardiovascular magnetic resonance for risk stratification in chronic heart failure: prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy. Heart 97:727–732
Assomull RG, Prasad SK, Lyne J, Smith G, Burman ED, Khan M et al (2006) Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48:1977–1985
McCrohon JA, Moon JC, Prasad SK, McKenna WJ, Lorenz CH, Coats AJ et al (2003) Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation 108:54–59
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA (2011) Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 57:891–903
Ugander M, Oki AJ, Hsu LY, Kellman P, Greiser A, Aletras AH et al (2012) Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur Heart J 33:1268–1278
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Arheden H, Saeed M, Higgins CB, Gao DW, Bremerich J, Wyttenbach R et al (1999) Measurement of the distribution volume of gadopentetate dimeglumine at echo-planar MR imaging to quantify myocardial infarction: comparison with 99mTc-DTPA autoradiography in rats. Radiology 211:698–708
Bondarenko O, Beek AM, Hofman MB, Kuhl HP, Twisk JW, van Dockum WG et al (2005) Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson 7:481–485
Schelbert EB, Testa SM, Meier CG, Ceyrolles WJ, Levenson JE, Blair AJ et al (2011) Myocardial extravascular extracellular volume fraction measurement by gadolinium cardiovascular magnetic resonance in humans: slow infusion versus bolus. J Cardiovasc Magn Reson 13:16
Wong TC, Piehler K, Meier CG, Testa SM, Klock AM, Aneizi AA et al (2012) Association between extracellular matrix expansion quantified by cardiovascular magnetic resonance and short-term mortality. Circulation 126:1206–1216
Green JJ, Berger JS, Kramer CM, Salerno M (2012) Prognostic value of late gadolinium enhancement in clinical outcomes for hypertrophic cardiomyopathy. JACC Cardiovasc Imaging 5:370–377
Hong YJ, Park CH, Kim YJ, Hur J, Lee HJ, Hong SR et al (2015) Extracellular volume fraction in dilated cardiomyopathy patients without obvious late gadolinium enhancement: comparison with healthy control subjects. Int J Cardiovasc Imaging 31(Suppl 1):115–122
Bulluck H, Maestrini V, Rosmini S, Abdel-Gadir A, Treibel TA, Castelletti S et al (2015) Myocardial T1 mapping. Circ J 79:487–494
Pattanayak P, Bleumke DA (2015) Tissue characterization of the myocardium: state of the art characterization by magnetic resonance and computed tomography imaging. Radiol Clin N Am 53:413–423
Puntmann VO, Voigt T, Chen Z, Mayr M, Karim R, Rhode K et al (2013) Native T1 mapping in differentiation of normal myocardium from diffuse disease in hypertrophic and dilated cardiomyopathy. JACC Cardiovasc Imaging 6:475–484
Miller CA, Naish JH, Bishop P, Coutts G, Clark D, Zhao S et al (2013) Comprehensive validation of cardiovascular magnetic resonance techniques for the assessment of myocardial extracellular volume. Circ Cardiovasc Imaging 6:373–383
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM et al (2010) Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation 122:138–144
aus dem Siepen F, Buss SJ, Messroghli D, Andre F, Lossnitzer D, Seitz S et al (2015) T1 mapping in dilated cardiomyopathy with cardiac magnetic resonance: quantification of diffuse myocardial fibrosis and comparison with endomyocardial biopsy. Eur Heart J Cardiovasc Imaging 16:210–216
Barison A, Del Torto A, Chiappino S, Aquaro GD, Todiere G, Vergaro G et al (2015) Prognostic significance of myocardial extracellular volume fraction in nonischaemic dilated cardiomyopathy. J Cardiovasc Med (Hagerstown) 16:681–687
Kammerlander AA, Marzluf BA, Zotter-Tufaro C, Aschauer S, Duca F, Bachmann A et al (2016) T1 Mapping by CMR Imaging: From Histological Validation to Clinical Implication. JACC Cardiovasc Imaging 9:14–23
Puntmann VO, Carr-White G, Jabbour A, Yu CY, Gebker R, Kelle S et al (2016) T1-mapping and outcome in nonischemic cardiomyopathy: all-cause mortality and heart failure. JACC Cardiovasc Imaging 9:40–50
Schelbert EB, Piehler KM, Zareba KM, Moon JC, Ugander M, Messroghli DR, Valeti US, Chang CC, Shroff SG, Diez J, Miller CA, Schmitt M, Kellman P, Butler J, Gheorghiade M, Wong TC (2015) Myocardial Fibrosis Quantified by Extracellular Volume Is Associated With Subsequent Hospitalization for Heart Failure, Death, or Both Across the Spectrum of Ejection Fraction and Heart Failure Stage. J Am Heart Assoc 4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yoo Jin Hong.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
This study has received funding by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (NRF-2015R1C1A1A02036645). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors have declared that no competing interests exist.
Statistics and biometry
Kyunghwa Han kindly provided statistical advice for this manuscript.
One of the authors - Kyunghwa Han (PhD, a statistician) has significant statistical expertise.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Methodology
• prospective
• prognostic study
• performed at one institution
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Youn, JC., Hong, Y.J., Lee, HJ. et al. Contrast-enhanced T1 mapping-based extracellular volume fraction independently predicts clinical outcome in patients with non-ischemic dilated cardiomyopathy: a prospective cohort study. Eur Radiol 27, 3924–3933 (2017). https://doi.org/10.1007/s00330-017-4817-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4817-9