Abstract
Objects
To investigate the utility of fused high b value diffusion-weighted imaging (DWI) and T2-weighted imaging (T2WI) for evaluating depth of invasion in bladder cancer.
Methods
We included 62 patients with magnetic resonance imaging (MRI) and surgically confirmed urothelial carcinoma in the urinary bladder. An experienced genitourinary radiologist analysed the depth of invasion (T stage <2 or ≥2) using T2WI, DWI, T2WI plus DWI, and fused DWI and T2WI (fusion MRI). Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were investigated. Area under the curve (AUC) was analysed to identify T stage ≥2.
Results
The rate of patients with surgically confirmed T stage ≥2 was 41.9% (26/62). Sensitivity, specificity, PPV, NPV and accuracy were 50.0%, 55.6%, 44.8%, 60.6% and 53.2%, respectively, with T2WI; 57.7%, 77.8%, 65.2%, 71.8% and 69.4%, respectively, with DWI; 65.4%, 80.6%, 70.8%, 76.3% and 74.2%, respectively, with T2WI plus DWI and 80.8%, 77.8%, 72.4%, 84.9% and 79.0%, respectively, with fusion MRI. AUC was 0.528 with T2WI, 0.677 with DWI, 0.730 with T2WI plus DWI and 0.793 with fusion MRI for T stage ≥2.
Conclusion
Fused high b value DWI and T2WI may be a promising non-contrast MRI technique for assessing depth of invasion in bladder cancer.
Key Points
• Accuracy of fusion MRI was 79.0% for T stage ≥2 in bladder cancer.
• AUC of fusion MRI was 0.793 for T stage ≥2 in bladder cancer.
• Diagnostic performance of fusion MRI was comparable with T2WI plus DWI.
• As a non-contrast MRI technique, fusion MRI is useful for bladder cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In bladder cancer, the depth of invasion is important for planning therapeutic strategies. For a patient with non-muscle-invasive bladder cancer (T stage <2), transurethral resection of the bladder (TURB) is generally recommended for complete tumour removal [1]. When a cancer penetrates further into the muscle layer and is thus difficult to remove by TURB, radical cystectomy with urinary diversion is required [2].
Many studies have demonstrated that diffusion-weighted imaging (DWI) is a useful non-contrast magnetic resonance imaging (MRI) technique for evaluating bladder cancer [3–12]. Takeuchi et al. reported that the overall accuracy of T2-weighted imaging (T2WI) plus DWI for assessing T stage was higher than that of T2WI alone or comparable with that of T2WI plus contrast-enhanced imaging [6]. According to a previous study with 362 patients, the interpretation of T2WI plus DWI was also useful for evaluating the T stage of bladder cancer [10]. Therefore, the combination of T2WI and DWI may have potential as a non-contrast MRI interpretation method for evaluating the depth of invasion in bladder cancer.
Recently, fused high b value DWI and T2WI has shown promise for assessing the depth of invasion of gynecologic malignancies [13, 14]. Because DWI is limited by spatial resolution, fusion of DWI onto the background T2WI may facilitate depiction of the functional status of the tumour (e.g. true cancerous area) with anatomical details (e.g. involved or adjacent organs) simultaneously. In addition, the fusion technique may replace meticulous, but relatively inconvenient investigation of two different MRI sequences. However, it remains unclear whether fused high b value DWI and T2WI is a feasible technique for the evaluation of the depth of invasion in bladder cancer.
Thus, we investigated the diagnostic performance of fused high b value DWI and T2WI, as a non-contrast MRI method, in the evaluation of depth of invasion in bladder cancer.
Materials and methods
Patients
The institutional review board at our institution approved this retrospective study and the requirement for informed consent was waived. A consecutive series of 66 patients who underwent preoperative MRI with data sets available for the image fusion at the workstation and surgically proven malignancy of the bladder were identified by a search of electronic medical records. Of these patients, four were excluded because of lack of urothelial carcinoma (adenocarcinoma of the urachus, n = 3; squamous carcinoma of the bladder, n = 1). Thus, the final study group (n = 62) had preoperative MRI and surgically proven urothelial carcinoma of the bladder. The characteristics of study group are summarized in Table 1.
MRI examination
All MRI was performed in one of two 3-T MR machines (Discovery MR750 or MR750w, GE Medical Systems, Milwaukee, WI) using a phased-array body coil. To distend the bladder, urination was prohibited for at least 1 h prior to MRI examination. To suppress bowel peristalsis, 20 mg of butyl scopolamine (Buscopan; Boehringer Ingelheim, Ingelheim am Rhein, Germany) was injected intramuscularly prior to MRI.
The T2WI protocols were as follows: TR, 4000–6500; TE, 98–115; slice thickness, 6 mm; field-of-view, 240 mm; matrix, 416 × 320. The DWI protocols were as follows: TR, 3900–5000; TE, 55–59; slice thickness, 6 mm; field-of-view, 240 mm; matrix, 128 × 128; and b values, 50 and 1000 s/mm2. Both T2WI and DWI were obtained with the axial plane perpendicular to the craniocaudal axis.
Fusion of high b value DWI onto T2WI was conducted using an image processing workstation (AW, GE Medical system, Milwaukee, WI) by a third-year radiology resident (M.L.) who was not involved in the image analysis. The colour-coded signal of DWI of a b value of 1000 s/mm2 was overlaid onto T2WI. The section level and field-of-view were automatically adjusted between DWI and T2WI by the software in the workstation. The MR examination time was not prolonged for obtaining the fusion images because all the fusion process was performed at the workstation after MR examination.
Pathology examination
All patients underwent surgical treatment for pathologic confirmation and tumour removal. For 48 patients, TURB was performed by an experienced urologist (Y.D.C., more than 20 years of experience in bladder surgery). To ensure negative surgical margins and assess T stage, TURB included the removal of tumour foci with/without deep biopsy of muscles at the tumour base. The remaining 14 patients underwent cystectomy. Two experienced pathologists determined the pathologic T stage with the surgical specimens, according to the 7th edition of the AJCC cancer staging [15]. In this study, the patients were divided into two groups based on the status of muscle invasion: (a) T stage <2 and (b) T stage ≥2.
Image interpretation
A genitourinary radiologist (S.Y.P., 5 years of experience in bladder imaging) who was unaware of the pathology results analysed non-contrast MRI of the bladder. Non-contrast MRI consisted of the following four image sets analysed in order: (a) T2WI, (b) DWI, (c) T2WI plus DWI and (d) fusion MRI. The interpretation session for each image set was performed at an interval of 3 weeks.
Bladder cancer was defined as a focal nodular or polypoid lesion of intermediate signal intensity on T2WI, diffusion restriction (e.g. hyperintensity) on DWI, or reddish colour on fusion MR. On T2WI, the disruption of hypointense line of normal bladder wall by a tumour was considered as muscle invasion [16]. On DWI, the findings of a hyperintense tumour with a hypointense stalk or intact hypointensity of submucosa was indicative of non-muscle invasion, whereas extension of the hyperintense tumorous area into relatively hypointense bladder wall was considered as muscle invasion [6]. On fusion MRI, a reddish tumorous area overlapped on T2-hypointense bladder wall was considered as muscle invasion. To determine the muscle invasion by a cancer (e.g. T stage ≥2), a five-point scale was utilized: score of 1, definitely absent; score of 2, probably absent; score of 3, indeterminate; score of 4, probably present; and score of 5, definitely present. Scores of 4 or 5 were regarded as T stage ≥2. When multiple tumour foci were seen on MRI, a single lesion showing the deepest invasion was representative of T stage for a patient.
Statistical analysis
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of T2WI, DWI, T2WI plus DWI, and fusion MRI were investigated for the evaluation of depth of invasion in bladder cancer.
We analysed the area under the curve (AUC) of each T2WI, DWI, T2WI plus DWI, and fusion MRI and compared the AUCs using the receiver operating-characteristic (ROC) curve analysis with Delong’s test. The p values from multiple testing were adjusted by Benjamini–Hochberg correction.
The above statistical analyses were conducted for all patients and patients with a single lesion separately. MedCalc (version 13.0, MedCalc Software, Mariakerke, Belgium) was used for the statistical analysis. A p value less than 0.05 was considered statistically significant.
Results
Sensitivity, specificity, PPV, NPV and accuracy
The distribution of the five-point scores for T stage ≥2 is summarized in Table 2. The rate of T stage ≥2 was 41.9% (26/62) for all patients and 46.3% (19/41) for patients with a single lesion in this study.
For identification of T stage ≥2, the sensitivity, specificity, PPV, NPV and accuracy were 50.0%, 55.6%, 44.8%, 60.6% and 53.2%, respectively, with T2WI; 57.7%, 77.8%, 65.2%, 71.8% and 69.4%, respectively, with DWI; 65.4%, 80.6%, 70.8%, 76.3% and 74.2%, respectively, with T2WI plus DWI and 80.8%, 77.8%, 72.4%, 84.9% and 79.0%, respectively, with fusion MRI in all patients (Table 3).
The sensitivity, specificity, PPV, NPV and accuracy were 47.4%, 68.2%, 56.3%, 60.0% and 58.5%, respectively, with T2WI; 57.9%, 81.8%, 73.3%, 69.2% and 70.7%, respectively, with DWI; 68.4%, 86.4%, 81.3%, 76.0% and 78.1%, respectively, with T2WI plus DWI and 79.0%, 86.4%, 83.3%, 82.6% and 82.9%, respectively, with fusion MRI in patients with a single lesion.
ROC curve analysis
The AUC for the identification of T stage ≥2 was 0.528 (95% confidence interval [CI], 0.397–0.656) with T2WI, 0.677 (95% CI, 0.547–0.791) with DWI, 0.730 (95% CI, 0.602–0.835) for T2WI plus DWI and 0.793 (95% CI, 0.671–0.885) with fusion MRI for all patients (Fig. 1). The AUC for the identification of T stage ≥2 was 0.578 (95% CI, 0.414–0.730) with T2WI, 0.699 (95% CI, 0.535–0.832) with DWI, 0.774 (95% CI, 0.617–0.890) for T2WI plus DWI and 0.827 (95% CI, 0.676–0.927) with fusion MRI for patients with a single lesion.
ROC curves of non-contrast MRI techniques for assessing T stage ≥2 in bladder cancer. a AUCs of T2WI, DWI, T2WI plus DWI, or fusion MRI were 0.528, 0.677, 0.730 and 0.793 for all patients, respectively. b AUCs of T2WI, DWI, T2WI plus DWI, or fusion MRI were 0.578, 0.699, 0.774 and 0.827 for patients with a single lesion, respectively
The AUC of T2WI plus DWI or fusion MRI was significantly higher than that of T2WI for all patients or patients with a single lesion (p < 0.05) (Table 4). The AUC of DWI was higher than that of T2WI for all patients (p = 0.044), while the AUCs of DWI and T2WI were similar for patients with a single lesion (p = 0.168). There were no significant differences in AUC values among DWI, T2WI plus DWI, and fusion MRI (p > 0.05) (Figs. 2, 3, and 4).
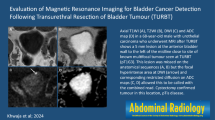
A 67-year-old man with bladder cancer. a T2WI, b DWI of b-1000 and c fusion MRI show a tumour focus, measuring 2.5 cm, in left wall of the urinary bladder (arrow). For this patient, T stage was determined to be 2 or greater on T2WI (arrowheads), while it was found to be less than 2 on DWI, T2WI plus DWI, or fusion MRI. The pathologic T stage was less than 2
A 60-year-old woman with bladder cancer. a T2WI, b DWI of b-1000 and c fusion MRI show a tumour focus, measuring 4.5 cm, in the posterior wall of the urinary bladder (arrow). For this patient, the cancerous area was located in the top of a stalk-like structure on T2WI or DWI (red dotted area), while fusion MRI additionally depicted the infiltrative area of a cancer within the bladder wall (arrowheads). Thus, T stage was determined to be less than 2 by T2WI, DWI, or T2WI plus DWI, while it was determined to be 2 or greater by fusion MRI. The pathologic T stage was 2 or greater
Discussions
In our study, fused high b value DWI and T2WI yielded good diagnostic performance (approximate accuracy of 80% and AUC of 0.8), which was slightly higher than that with the data from DWI alone or T2WI plus DWI, although the superiority of fusion MRI was not statistically significant. Those findings were consistently shown for all patients or patients with a single lesion in the bladder. This indicates that fusion MRI may have the potential to be a promising non-contrast MRI method.
In the urinary bladder, DWI can depict a focal cancerous area, where water diffusion is more restricted by the denser cellularity of the cancer. The cancerous tissues manifest as a focal area of hyperintensity on high b value DWI and low apparent diffusion coefficient (ADC) value on the ADC map [3]. With this background, it has been shown that DWI provides feasible detection [4], staging [5, 6, 10, 11], histologic grading [6, 7, 12] and assessment of therapeutic response [17, 18] for bladder cancer. Furthermore, DWI may also differentiate post-TURB inflammatory changes of the bladder wall from bladder cancer [8]. However, DWI has limited spatial resolution. To overcome this limitation, a combined analysis with T2WI and DWI may be required.
El-Assmy et al. reported that the accuracy of DWI is 63.9% for differentiating T stage <2 from T stage ≥2, while the accuracy of T2WI is just 6.1% [5]. Takeuchi et al. reported that the accuracy of T2WI plus DWI (96%) was higher than that of T2WI alone (79%) for differentiating T stage <2 from T stage ≥2 [6]. According to a study from Wu et al., the accuracy was 74–83% with T2WI, 87–92% DWI and 92–98% with T2WI plus DWI. In our study, the accuracies of T2WI, DWI and T2WI plus DWI were 53.2%, 69.4% and 74.2%, respectively. Although there is variability in accuracy, the data from previous studies and ours suggest that combined analysis of T2WI and DWI may provide the best interpretation, as a non-contrast MRI interpretation method, for assessing the muscle invasion of bladder cancer.
Technically, fusion of high b value DWI and T2WI is not complex. Dragging the retrieved DWI over T2WI at the dedicated workstation generated the fusion images in this study. The section level and field-of-view between DWI and T2WI were adjusted automatically by the dedicated software. In addition, there was no significant difference in AUC between fusion MRI and T2WI plus DWI (fusion MR, 0.793 for all patients and 0.827 for patient with a single lesion; T2WI plus DWI, 0.730 for all patients and 0.774 for patient with a single lesion; p > 0.05 between fusion MRI and T2WI plus DWI). A single interpretation of fusion MRI may replace the complex interpretation process required for conventional DWI and T2WI. Further prospective studies are required to confirm our findings.
This study had some limitations. First, a comparison between fusion MRI and dynamic contrast-enhanced (DCE) MRI was not performed. Previous studies have shown the great promise of fusion MRI for the evaluation of depth of invasion in gynecologic malignancies [13, 14]. The present results warrant further comparison studies between fusion and DCE MRI. Second, this study was performed at the patient level. The absence of a cystoscopic or pathologic tumour map precluded lesion-by-lesion analysis for patients with multiple tumour foci. Thus, we additionally analysed the diagnostic performance of non-contrast MRI techniques for patients with a single lesion to overcome the current limitation, and the data from the two groups (e.g. all patients and patients with a single lesion) consistently showed the highest AUC of the fusion MRI. Third, since a majority of the study population underwent TURB (77.4%, 48/62), the possibility of pathologic understaging exists. However, TURB included additional muscle resection at the tumour base for assessing the depth of invasion and achieving a negative tumour margin by the surgeon’s decision in this study. Furthermore, we simplified the T stage into two groups, which could minimize the misdiagnosis of T stage. Fourth, there might be possibility of misalignment between T2WI and DWI. Rigid registration was applied for fusion, and the spatial resolution between the two image sets was not identical. Bladder and bowel motion might also hamper correct image fusion. We tried to minimize it by (a) encouraging full distension of the urinary bladder before MR examination, (b) using an antispasmodic to minimize the motion of the bladder and adjacent bowels and (c) obtaining DWI right after T2WI for the distended bladder. In addition, the section level and field-of-view were automatically adjusted between T2WI and DWI by the workstation. Previous studies also reported promising data in terms of tumour staging with similar fusion methods (e.g. rigid registration or different spatial resolution between T2WI and DWI) [13, 14]. Advanced imaging and fusion techniques would improve the diagnostic accuracy. Fifth, our study was performed retrospectively. Hence, there might be the possibility of recall bias in the image interpretation of each set. To minimize this effect, an interval of 3 weeks between each interpretation set was applied. Finally, the inter-reader agreement was not investigated. Prospective, multi-institutional studies are required to validate our preliminary results.
In conclusion, fused high b value DWI and T2WI may be a promising non-contrast MRI technique for assessing depth of invasion in bladder cancer, which may help determine surgical planning.
Abbreviations
- AUC:
-
area under the curve
- CI:
-
confidence interval
- DCE:
-
dynamic contrast-enhanced
- DWI:
-
diffusion-weighted imaging
- MRI:
-
magnetic resonance imaging
- NPV:
-
negative predictive value
- PPV:
-
positive predictive value
- ROC:
-
receiver operating-characteristic
- TE:
-
echo time
- TR:
-
repetition time
- TURB:
-
transurethral resection of the bladder
- T2WI:
-
T2-weighted imaging
References
Babjuk M, Bohle A, Burger M et al (2016) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol. doi:10.1016/j.eururo.2016.05.041
World Health Organization Consensus Conference on Bladder Cancer, Hautmann RE, Abol-Enein H et al (2007) Urinary diversion. Urology 69:17–49
Matsuki M, Inada Y, Tatsugami F, Tanikake M, Narabayashi I, Katsuoka Y (2007) Diffusion-weighted MR imaging for urinary bladder carcinoma: initial results. Eur Radiol 17:201–204
Abou-El-Ghar ME, El-Assmy A, Refaie HF, El-Diasty T (2009) Bladder cancer: diagnosis with diffusion-weighted MR imaging in patients with gross hematuria. Radiology 251:415–421
El-Assmy A, Abou-El-Ghar ME, Mosbah A et al (2009) Bladder tumour staging: comparison of diffusion- and T2-weighted MR imaging. Eur Radiol 19:1575–1581
Takeuchi M, Sasaki S, Ito M et al (2009) Urinary bladder cancer: diffusion-weighted MR imaging–accuracy for diagnosing T stage and estimating histologic grade. Radiology 251:112–121
Kobayashi S, Koga F, Yoshida S et al (2011) Diagnostic performance of diffusion-weighted magnetic resonance imaging in bladder cancer: potential utility of apparent diffusion coefficient values as a biomarker to predict clinical aggressiveness. Eur Radiol 21:2178–2186
El-Assmy A, Abou-El-Ghar ME, Refaie HF, Mosbah A, El-Diasty T (2012) Diffusion-weighted magnetic resonance imaging in follow-up of superficial urinary bladder carcinoma after transurethral resection: initial experience. BJU Int 110:E622–E627
Takeuchi M, Sasaki S, Naiki T et al (2013) MR imaging of urinary bladder cancer for T-staging: a review and a pictorial essay of diffusion-weighted imaging. J Magn Reson Imaging 38:1299–1309
Wu LM, Chen XX, Xu JR et al (2013) Clinical value of T2-weighted imaging combined with diffusion-weighted imaging in preoperative T staging of urinary bladder cancer: a large-scale, multiobserver prospective study on 3.0-T MRI. Acad Radiol 20:939–946
Ohgiya Y, Suyama J, Sai S et al (2014) Preoperative T staging of urinary bladder cancer: efficacy of stalk detection and diagnostic performance of diffusion-weighted imaging at 3T. Magn Reson Med Sci 13:175–181
Zhou G, Chen X, Zhang J, Zhu J, Zong G, Wang Z (2014) Contrast-enhanced dynamic and diffusion-weighted MR imaging at 3.0T to assess aggressiveness of bladder cancer. Eur J Radiol 83:2013–2018
Park JJ, Kim CK, Park SY, Park BK (2015) Parametrial invasion in cervical cancer: fused T2-weighted imaging and high-b-value diffusion-weighted imaging with background body signal suppression at 3 T. Radiology 274:734–741
Lin G, Ng KK, Chang CJ et al (2009) Myometrial invasion in endometrial cancer: diagnostic accuracy of diffusion-weighted 3.0-T MR imaging--initial experience. Radiology 250:784–792
Edge SBBD, Compton CC, Fritz AG, Greene FL, Trotti A (eds) (2010) AJCC cancer staging manual (7th ed). Springer, New York
Verma S, Rajesh A, Prasad SR et al (2012) Urinary bladder cancer: role of MR imaging. Radiographics 32:371–387
Yoshida S, Koga F, Kawakami S et al (2010) Initial experience of diffusion-weighted magnetic resonance imaging to assess therapeutic response to induction chemoradiotherapy against muscle-invasive bladder cancer. Urology 75:387–391
Yoshida S, Koga F, Kobayashi S et al (2012) Role of diffusion-weighted magnetic resonance imaging in predicting sensitivity to chemoradiotherapy in muscle-invasive bladder cancer. Int J Radiat Oncol Biol Phys 83:e21–e27
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sung Yoon Park.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional review board approval was obtained.
Informed consent
Written informed consent was waived by the institutional review board.
Methodology
• retrospective
• cross sectional study
• performed at one institution
Rights and permissions
About this article
Cite this article
Lee, M., Shin, SJ., Oh, Y.T. et al. Non-contrast magnetic resonance imaging for bladder cancer: fused high b value diffusion-weighted imaging and T2-weighted imaging helps evaluate depth of invasion. Eur Radiol 27, 3752–3758 (2017). https://doi.org/10.1007/s00330-017-4759-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4759-2