Abstract
Purpose
To assess technical feasibility, safety, and efficacy of the liver venous deprivation (LVD) technique that combines both portal and hepatic vein embolization during the same procedure for liver preparation before major hepatectomy.
Materials and methods
Seven patients (mean age:63.6y[42-77y]) underwent trans-hepatic LVD for liver metastases (n = 2), hepatocellular carcinoma (n = 1), intrahepatic cholangiocarcinoma (n = 3) and Klatskin tumour (n = 1). Assessment of future remnant liver (FRL) volume, liver enzymes and histology was performed.
Results
Technical success was 100 %. No complication occurred before surgery. Resection was performed in 6/7 patients. CT-scan revealed hepatic congestion in the venous-deprived area (6/7 patients). A mean of 3 days (range: 1–8 days) after LVD, transaminases increased (AST: from 42 ± 24U/L to 103 ± 118U/L, ALT: from 45 ± 25U/L to 163 ± 205U/L). Twenty-three days (range: 13–30 days) after LVD, FRL increased from 28.2 % (range: 22.4–33.3 %) to 40.9 % (range: 33.6–59.3 %). During the first 7 days, venous-deprived liver volume increased (+13.4 %) probably reflecting vascular congestion, whereas it strongly decreased (-21.3 %) at 3-4 weeks. Histology (embolized lobe) revealed sinusoidal dilatation, hepatocyte necrosis and important atrophy in all patients.
Conclusion
Trans-hepatic LVD technique is feasible, well tolerated and provides fast and important hypertrophy of the FRL. This new technique needs to be further evaluated and compared to portal vein embolization.
Key Points
• Twenty-three days after LVD, FRL increased from 28.2 % (range:22.4-33.3 %) to 40.9 % (range:33.6–59.3 %)
• During the first 7 days, venous-deprived liver volume increased (+13.4 %)
• Venous-deprived liver volume strongly decreased (mean atrophy:229 cc; -21.3 %) at 3-4 weeks
• Histology of venous-deprived liver revealed sinusoidal dilatation, hepatocyte necrosis and important atrophy
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its first description by Kinoshita et al. in 1986 [1], portal vein embolization (PVE) has been widely used to generate hypertrophy of the nonembolized lobe in patients undergoing major hepatectomy in order to prevent small-for-size remnant liver resulting in post-operative liver insufficiency. Although PVE is a safe and effective procedure [2], it does not always induce sufficient hypertrophy of the future remnant liver (FRL) even after a long time [3]. Consequently, several approaches have been proposed to improve PVE: Optimization of the embolizing agent for PVE is still a matter of debate but animal [4, 5] and human [6, 7] studies have strongly suggested that permanent embolizing agents and especially cyanoacrylate (glue) was safe and induced greater liver hypertrophy than other agents. A combined technique with subsequent embolization of ipsilateral hepatic artery has also been explored. Though efficient in terms of FRL hypertrophy, it strongly increased the risk of liver abscess due to biliary ischemia [8], and thus has been abandoned. Intrahepatic biliary ablation using ethanol has also been proposed [9] but concerns have been raised to prevent damage to the bile ducts of the FRL. Hematopoeitic stem cells as an adjunct treatment to PVE has been proposed [10], but is still under investigation. Recently, surgeons developed the ALPPS (associating liver partition and portal vein ligation for staged hepatectomy) procedure and reported a very high rate of liver hypertrophy [11], thereby suggesting that a more aggressive approach on intra-hepatic liver vessels (by liver partition) resulted in better results. However, this approach for two-staged hepatectomy was recently demonstrated to dramatically increase perioperative morbidity and mortality [12].
In case of insufficient liver regeneration following PVE, some authors suggested to embolize hepatic vein(s) (HVs) [13–17]. Interestingly, the sequential right hepatic vein embolization (HVE) after right PVE demonstrated an incremental effect on the FRL, thus allowing some additional patients to be operated on. Although attractive, this approach requires two different procedures and does not spare time as compared to PVE alone.
To shorten and optimize the phase of liver preparation before surgery, we developed the so-called liver venous deprivation (LVD) technique that combines both PVE and HVE during the same procedure.
The aim of this study was to assess the feasibility, safety, and efficacy of this new technique for liver preparation before major hepatectomy.
Materials and methods
This study consisted in a retrospective analysis of our experience (two centres) with LVD technique before major hepatectomy. All patients gave their written informed consent for the procedure and our institutional review boards approved the retrospective analysis of their data.
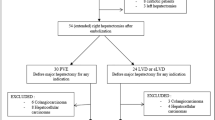
Over a 4-month period, seven non-cirrhotic consecutive patients (three women, four men; mean age: 63.6 years; range: 42–77 years) referred to our centres (University hospitals of Montpellier and Nice, France) for major hepatectomy in a context of small FRL, were included in this series (Supplemental Material 1). In each centre, the therapeutic strategy regarding these patients was discussed at our weekly tumours board meeting, including liver surgeons, oncologists, hepatologists and interventional radiologists. Tumours board meetings considered FRL as small when baseline FRL was <35 % of the total liver volume in patients with a suspicion of impaired liver function (bile duct obstruction [drained or not], multiple lines of oxaliplatin-based chemotherapy) and <30 % in the others. LVD was planned in all of these patients to increase FRL volume.
Technique (Fig. 1)
A) Portal vein embolization of right branches using a lipiodol-glue mixture through transhepatic access in a 70-year-old man referred for preparation of liver resection of colorectal metastases. Please note that a 0.018” guidewire has been inserted in the right HV after US puncture with a Chiba needle. B) Venography of the right HV through a 7 F-sheath (guidewire in the superior vena cava). C) Deployment of a 20 mm Amplatzer Vascular Plug with its distal part positioned 5–10 mm before the origin of the right HV. D) Injection through the 7 F-sheath showing that the plug is occluded but demonstrating intra-hepatic veno-venous collateral pathways (arrows) between the right and the middle HVs. E) Cautious embolization of the right HV and tract embolization using lipiodol/glue mixture
The LVD technique (combined portal vein and HV embolization) was performed under general anaesthesia. All patients received intravenous prophylactic antibiotics (amoxicillin + clavulanic acid). The right HV (and accessory right HV when present) was accessed first using a “1-stick” technique [18] with an Aprima introducer set (Cook Medical, Bloomington, IN). The distal part of the right HV was punctured under US guidance with a 15-cm-long 21-gauge Chiba introducer needle and opacified. Then a 0.018-inch Cope mandril guidewire was introduced through the needle to gain initial access and the Aprima introducer set was left in the right HV to maintain access during the PVE procedure. Then a right portal vein branch was accessed using the same technique (Aprima introducer set) under US guidance. After accommodation of a 0.035-inch guidewire in the outer sheath of the Aprima introducer, a 11 cm-long 5 F sheath (Super Arrow Flex PSI set, Teleflex medicine, Ahtlone, Ireland) was inserted into the portal venous system to secure access. A 5 F shaped catheter (Kumpe, Terumo, Tokyo, Japan) was advanced over an Advantage stiff hydrophilic 0.035” guidewire (Terumo, Tokyo, Japan) into the portal trunk where portography was performed. The PVE procedure was performed as described elsewhere [19, 20]. In both centres, embolization was conducted using a mixture of 1-4 mL of iodized oil (Lipiodol, Guerbet, Aulnay-sous-bois, France) and 1 mL of n-butyl-cyanoacrylate (Glubran II, GEM, Italy). Segment IV was not embolized. Following embolization, the sheath was pulled back while injecting the same mixture for tract embolization.
The right HV access was used to introduce a trans-hepatic 7 F Destination sheath over an Advantage 0.035” guidewire. An Amplatzer Vascular Plug II (St-Jude Medical, Plymouth, MN) of 18-22 mm was deployed with its distal part 10 mm before the junction with the inferior vena cava, to facilitate further surgical HV ligature. Injection of contrast medium was used to check for right HV occlusion by the plug, patent distal branches of the right HV and potential veno-venous collateral vessels. Then, embolization of the distal branches of the right HV, as well as collaterals (inter-hepatic vein communications when visible) was conducted using a 1:1 mixture of lipiodol:n-butyl-cyanoacrylate. During 7 F sheath removal, track embolization was performed using the same mixture. HVE and track embolization were achieved using 1-2 vials of glue.
During the two days following the procedure, pain was managed using paracetamol and/or morphine titration when necessary.
Volumetric and congestion CT assessment
Baseline computed tomography (CT) imaging data were obtained a mean of 6 days (range: 0–24 days) before the LVD procedure. All patients had follow-up imaging (Supplemental Material 2 for protocol) with at least one CT-scan during the first 15 days, and between 15–30 days after the procedure. The ratio between the FRL and the whole liver volume minus tumour volume was calculated and defined as the FRL ratio. Because we occluded veinous outflow from the right hepatic vein, we also looked at hepatic congestion. It was defined as hypoattenuation at portal venous phase on the first post-procedure CT-scan , as previously reported after venous deprivation during hepatectomy [21].
Liver enzymes
Serum liver enzymes were assessed by measuring serum aspartate aminotransferase (AST), serum alanine aminotransferase (ALT), gamma-glutamyl-transpeptidase (GGT), alkaline phosphatase (ALP), total bilirubin and prothrombin time (PT) before , after the LVD procedure (each day during hospital stay), at day 8 and the day before surgery.
Histological analysis
Liver samples of representative embolized and non-embolized lobe (when available) were performed to assess the histological changes in the resected specimen.
Liver tissues were fixed in 10 % formalin. Paraffin tissue sections were stained with hematoxylin and eosin. Reticulin fibre staining was helpful to visualize atrophy or hypertrophy of hepatocyte plates.
Additional immunostaining were also performed in the embolized and non-embolized samples: CD31 (DAKO, Clone JC70A, 1/25 dilution) to visualize capillarization of sinusoids (angiogenesis), hepatocyte paraffin 1 (DAKO, OCH1E5 clone, 1/25 dilution) as a marker for hepatocytes and Ki-67 (Ventana-Roche Ready-to-Use) using MIB-1 monoclonal antibody as a marker for hepatocyte replication.
Statistical analysis
Categorical variables were described using percentages and other variables as means and standard deviations. Given the small number of patients, comparisons of laboratory tests and liver volumes were not performed. All descriptive analyses were performed using Stata software version 11.0 (Stata corporation, College Station, TX, USA).
Results
LVD was achieved in all patients. No complication related to the procedure was observed, and especially no migration of embolic material. Mean hospital duration was 3 days (range: 2–5 days). Pain was absent (n = 2) or moderate (n = 5) and was only managed using IV paracetamol when necessary. A fever > 38°c probably related to a post-embolization syndrome (no evidence of infection) was observed in 5/7 patients and was managed using paracetamol only. On post-procedural CT-scan, successful embolization of right portal branches was obtained in all cases without non-target embolization. Right HV and accessory right HV (when present) were occluded by the amplatzer plug in all cases while preserving a 10 mm distance at their origin for surgical clamping. In two patients, the first branch of the right HV (usually draining segment VIII) was not occluded although the proximal part of the plug was placed beyond the origin of this branch (Fig. 2).
A) Baseline axial CT-scan passing through the left portal vein (future remnant liver [highlighted in blue] represents 23 % of total liver volume). B) Axial CT-scan 4 weeks after liver venous deprivation showing considerable volume increase in future remnant liver (43 % of the total liver volume). Please note the atrophy of the right liver lobe. C) Gross appearance of the liver without any vascular clamping, showing both a discolored (darker) and atrophied right lobe and a definite parenchymal enlargement of the left liver lobe
When looking at hepatic congestion on the first post-procedure CT-scan (mean: 6 days [range: 1–14 days]), heterogeneous hypoattenuating areas in the venous-deprived areas were observed in 6/7 patients (Fig. 3). This was confirmed at the beginning of the surgical procedure, during which the venous-deprived liver surface was discoloured (blue) without any vascular clamping (Fig. 3).
CT-scan (A) and surgical view (B) without any vascular clamping 13 days after liver venous deprivation in a 77-year-old woman bearing hepatocellular carcinoma (without cirrhosis). Please note the hypo-attenuated area on CT-scan (stars) and the clear demarcation and discoloration of the venous-deprived area (arrows) on the surgical view
Six of seven patients were resected a mean 23 days after LVD (range: 13–30 days), whereas one patient was not due to peritoneal carcinomatosis. R0 resection was performed in 5/6 patients (R1 in one patient). Unfortunately, the patient with the highest %FRL died 10 days after surgery from a septic shock (due to post-operative pneumonitis in a context of chronic obstructive pulmonary disease) without any liver insufficiency whereas the other ones had a mean hospital stay of 8 days (range: 4–14 days). During the 8 weeks following surgery, none of them developed liver failure or decompensation.
Liver enzymes
During the first 8 days after the LVD procedure, AST and ALT increased from 42 ± 24 U/L to 103 ± 118 U/L and from 45 ± 25 U/L to 163 ± 205 U/L, respectively, (peak observed at a mean of 3 days [range: 1-8]), whereas GGT moderately increased from 135 ± 110 U/L to 187 ± 136 U/L, ALP remained stable (from 207 ± 192 U/L to 206 ± 240 U/L) and total bilirubin moderately decreased (from 27 ± 35 μmol/L to 22 ± 16 μmol/L). During the same time, PT moderately increased from 87 ± 18 % to 91 ± 8 %. One day before surgery, AST, ALT, GGT and ALP had returned to baseline values (respectively, 40 ± 25 U/L, 41 ± 30 U/L, 140 ± 105 U/L and 210 ± 183 U/L) and total bilirubin had decreased (18 ± 15 μmol/L). At the same time point, PT was 94 ± 9 %.
Volumetric analysis (Table 1)
After a mean delay of 23 days (range: 13–30 days) after LVD, the FRL volume increased from 409 cc (range: 345–601 cc) to 624 cc (range: 510–807 cc) (Fig. 4). During the same time, total liver volume moderately increased from 1558 cc (range: 1492–1827 cc) to 1650 cc (range: 1461–2109 cc). Percentage of FRL strongly increased from 28.2 % (range: 22.4 %–33.3 %) to 40.9 % (range: 33.6–59.3 %), resulting in a mean degree of hypertrophy of 12.7 % (FRL before surgery – FRL before LVD) (Fig. 5).
Coronal CT-scan performed one day after LVD in a 71-year-old patient, showing glue/lipiodol in the right portal venous branches and the Amplatzer vascular plug in the right HV. The first branch of the right HV (draining segment VIII) was not occluded although the proximal part of the plug was placed beyond the origin of this branch. Please note the hypoattenuated area in the venous-deprived area (star)
Evolution of liver volumes over time seems to result from a two-step process: during the first 7 days, venous-deprived liver volume strongly increased (from 1253 to 1420 cc; +13.4 %) in 3/3 patients, probably reflecting initial vascular congestion. On the contrary, important liver atrophy (mean volume atrophy: 229 cc; range [112–352 cc]; -21.3 % as compared to baseline) of the venous-deprived liver was observed at 3-4 weeks in 4/4 patients.
Histological analysis
Histological results were consistent with a two-step process. Both morphological and immunostaining analyses showed histological lesions in embolized-lobe in all samples: centro- and medio-lobular hepatic plates were atrophied, especially in the vicinity of sinusoidal dilatation; variable stages of focal necrosis were noted in centro- and medio-lobular areas (Fig. 6). In one case, an extensive hepatocyte necrosis was observed.
Reticulin staining showed heavy diffuse staining indicating collapse of liver parenchyma of the embolized-lobe whereas in non-embolized lobe, the reticulin network was reduced with a few fibres delimitated regenerative bigger hepatocytes (Fig. 7). CD31 immunostaining showed a low capillarization of sinusoids in the embolized lobe and a high capillarization (i.e., high angiogenesis) in non-embolized lobe (Fig. 7). Ki67 index did not differ between embolized and non-embolized lobes. Hepatocyte 1 immunostaining was helpful to confirm atrophy of hepatocyte plates in the embolized lobe (Fig. 7).
Reticulin fibre staining (Original magnification × 200) : Heavy diffuse staining by hepatocyte plates atrophy in embolized lobe (A) and reticulin contracting due to hypertrophy of hepatocyte plates in non-embolized lobe (B). CD31 immunostaining (Original magnification × 200). Endothelial cells are stained reddish-brown. Lower capillarization of sinusoids in embolized lobe (C) and higher capillarization of sinusoids in non-embolized lobe (D). Hepatocyte 1 immunostaining (Original magnification × 200). Hepatocyte plates (stained reddish-brown) atrophied in embolized lobe (E) and not atrophied in non-embolized lobe (F)
Discussion
In the literature, we found only one case-report from Nagino et al. in 2002 [17] reporting HVE following PVE in the same day. Embolization of the right HV was used to modulate outflow and derive venous blood to the inferior-right HV in order to perform left hepatic trisegmentectomy with right HV resection. Sequential HVE after PVE has been proposed in other studies [13–16]. In the first reports, HVE was performed with coils either alone or in combination with vena cava filters in the HV. Minor and severe complications were reported due to migration of coils and/or filters. The use of Amplatzer vascular plugs strongly reduces the risk of migration (no case in our series), provided the plug is oversized by at least 50 %. Moreover, plugs can be re-captured (if necessary) and launched very precisely under both US and angiographic guidance to preserve the 10 mm necessary for the surgical ligation of HV using a stapler. In the literature, we found no report of HVE embolization through a trans-hepatic access. We think that this approach is better than the endovascular approach for the following reasons: 1) catheterization of HVs through a transjugular approach is not always easy, especially for accessory right HVs ; 2) inadvertent embolization of the middle HV can occur as reported in the series by Hwang et al. [14] because right and middle HV can be confounded during catheterization ; 3) US transhepatic puncture of a main and/or accessory HV(s) is technically easy using micropuncture sets ; and 4) although the surgical literature claimed that intrahepatic veno-venous collaterals need several weeks to develop after HV ligation, we observed in several patients these collaterals just several minutes after plug deployment. Because these vessels only develop when the plug is occluded, they can be embolized only through an intrahepatic access.
As for PVE, we choose to conduct embolization of feeding branches and collaterals of HVs using n-butyl-cyanoacrylate. This liquid agent is well designed for embolization of the remaining branches of HVs after plug deployment, but high experience is needed to conduct embolization of intrahepatic veno-venous collaterals without inadvertent embolization of middle HV and downstream migration of glue. Onyx might be safer but its cost was a strong limiting factor. We are currently experiencing other cyanoacrylates that might be better designed for such embolizations.
HVE following PVE has been proposed to induce more severe liver damage than PVE alone and as a consequence, to induce more and/or faster contralateral liver hypertrophy. The concept of HVE comes from living donor liver transplantation (LDLT). Anatomically, two portal vein branches drain into three HVs. When the liver is split, the middle HV remains either in the graft or in the remnant liver, thereby causing focal outflow obstruction either in the remnant or in the graft. This results in impaired regeneration of segments with focal outflow obstruction, and ultimately in liver atrophy [13, 14, 22, 23]. A similar phenomenon is observed after right hemi-hepatectomy with middle HV harvesting [24]. Interestingly, there is a strong relationship between hepatic congestion and liver regeneration. In LDLT [13, 14, 22, 23] as well as in resected patients with middle HV harvesting [24], the regeneration of segments with preserved outflow is increased. Physiologically in case of acute HV occlusion, compensatory increase in arterial flow is observed together with intrahepatic arterio-portal regurgitation. As a consequence, the portal vein acts as a draining vein with reversed flow [14, 15]. This could be useful in case of incomplete PVE due to challenging portal venous anatomy. However, these hemodynamic changes cannot occur if PVE is complete. Arterial flow in the venous-deprived parenchyma is preserved as observed on CT-scans of our patients but probably decreased due to the limited outflow route. Because centrolobular veins were not embolized, arterial blood should go either through sinusoids to reach a zone with preserved outflow, or through intrahepatic arterio-arterial communications between embolized and not-embolized areas. We were not able to elucidate the predominant mechanism in this study.
In 2012, van Lienden et al. reported that HVE combined with PVE had no short-term additional effect on hypertrophy in a rabbit model [25]. Human extrapolation of the results must be cautious. First, the regenerative response of rabbit liver is known to be fast but authors investigated it only during the first 7 days. Second, embolizations of both portal and HVs were conducted using proximal coils explaining that some distal branches were still patent. Our technique using proximal and distal embolization with glue is completely different. Third, in their paper, the hypertrophy response following HVE + PVE was higher than after PVE alone. Caudal-to-liver volume and the amount of proliferating hepatocytes showed a trend towards an increase after HVE + PVE. Thus, a limited sample size and/or a too limited study time could have explained non-significant results. In 107 consecutive patients who underwent PVE, a kinetic growth rate (KGR) of 2.4 % per week was noted in the weeks following PVE [26]. In our series, we observed a 4.2 % per week KGR (mean degree of hypertrophy divided by number of weeks) after LVD, meaning a +75 % increase in KGR as compared to PVE.
Interestingly, besides these excellent results in terms of hypertrophy, histological findings after LVD were considerably different from those observed after PVE alone [4, 27, 28]: hepatocellular damage is not usually observed after PVE, whereas extensive or focal necrosis in centro- and medio-lobular areas was noted in all patients after LVD. This can explain the 2-4 times increase in transaminase levels, whereas transaminase only slightly increased after PVE [27]. Moderate sinusoidal dilatation is sometimes reported after PVE, whereas a severe sinusoidal dilatation was systematically observed in our series. In LVD, hepatocyte atrophy was observed in the vicinity of sinusoidal dilatation in all cases. Histological atrophy was much more important than that usually observed after PVE. It translated into gross atrophy of venous-deprived liver, since a -21.3 % volume atrophy was noted 3-4 weeks after LVD, whereas a -12.3 % atrophy has been reported after PVE in 593 patients [7].
Several limitations must be acknowledged: 1) the limited number of patients, even though these patients were not selected; and 2) no cirrhotic patient was included. We know that hypertrophy response to PVE is impaired in case of cirrhosis [7]. The LVD technique needs to be explored in this setting in the future; and 3) all patients were operated on during the first 4 weeks, i.e., earlier than commonly reported after PVE [7]. Consequently, we have no data after 4 weeks. Additional increase in FRL volume and/or atrophy of venous-deprived liver might exist after 4 weeks; and 4) we evaluated only the liver volumes whereas the clinical endpoint is liver function. With 99 m-Tc labelled mebrofenin scintigraphy, it has been shown that the increase in liver function exceeds the increase in liver volume after PVE [29]. This technique would be of great interest for LVD; and 5) our study did not compare the results to PVE alone. Although we highlighted the differences between PVE and LVD in terms of parenchymal changes on post-operative imaging, histological findings and atrophy of embolized liver, it is much too early to change our practice. We are about to start a phase II randomized trial with both volumetric and functional evaluation to assess and maybe confirm the benefit of LVD over PVE.
In conclusion, trans-hepatic LVD technique is feasible, well-tolerated, and provides fast and important hypertrophy of the future liver remnant. This new technique needs to be further evaluated in a large series and compared to PVE.
Abbreviations
- PVE:
-
Portal vein embolization
- FRL:
-
Future remnant liver
- HV:
-
Hepatic vein
- HVE:
-
Hepatic vein embolization
- LVD:
-
Liver venous deprivation
- AST:
-
Aspartate aminotransferase
- ALT:
-
Serum alanine aminotransferase
- GGT:
-
Gamma-glutamyl-transpeptidase
- ALP:
-
Alkaline phosphatase
- PT:
-
Prothrombin time
- LDLT:
-
Living donor liver transplantation
References
Kinoshita H, Sakai K, Hirohashi K, Igawa S, Yamasaki O, Kubo S (1986) Preoperative portal vein embolization for hepatocellular carcinoma. World J Surg 10:803–808
Abulkhir A, Limongelli P, Healey AJ et al (2008) Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg 247:49–57
Yokoyama Y, Nagino M, Nimura Y (2007) Mechanisms of hepatic regeneration following portal vein embolization and partial hepatectomy: a review. World J Surg 31:367–374
de Baere T, Denys A, Paradis V (2009) Comparison of four embolic materials for portal vein embolization: experimental study in pigs. Eur Radiol 19:1435–1442
van den Esschert JW, van Lienden KP, Alles LK et al (2012) Liver regeneration after portal vein embolization using absorbable and permanent embolization materials in a rabbit model. Ann Surg 255:311–318
Guiu B, Bize P, Gunthern D, Demartines N, Halkic N, Denys A (2013) Portal vein embolization before right hepatectomy: improved results using n-butyl-cyanoacrylate compared to microparticles plus coils. Cardiovasc Intervent Radiol 36:1306–1312
van Lienden KP, van den Esschert JW, de Graaf W et al (2013) Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol 36:25–34
Gruttadauria S, Gridelli B (2007) Sequential preoperative ipsilateral portal and arterial embolization in patients with liver tumors: is it really the best approach? World J Surg 31:2427–2428
Kyokane T, Nagino M, Oda K, Nimura Y (2001) An experimental study of selective intrahepatic biliary ablation with ethanol. J Surg Res 96:188–196
am Esch JS, Schmelzle M, Furst G et al (2012) Infusion of CD133+ bone marrow-derived stem cells after selective portal vein embolization enhances functional hepatic reserves after extended right hepatectomy: a retrospective single-center study. Ann Surg 255:79–85
Schnitzbauer AA, Lang SA, Goessmann H et al (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255:405–414
Schadde E, Ardiles V, Robles-Campos R et al (2014) Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg 260:829–836, discussion 836-828
Balzan SM, Gava VG, Magalhaes MA, Dotto ML (2014) Outflow modulation to target liver regeneration: something old, something new. Eur J Surg Oncol 40:140–143
Hwang S, Lee SG, Ko GY et al (2009) Sequential preoperative ipsilateral hepatic vein embolization after portal vein embolization to induce further liver regeneration in patients with hepatobiliary malignancy. Ann Surg 249:608–616
Ko GY, Hwang S, Sung KB, Gwon DI, Lee SG (2010) Interventional oncology: new options for interstitial treatments and intravascular approaches: right hepatic vein embolization after right portal vein embolization for inducing hypertrophy of the future liver remnant. J Hepatobiliary Pancreat Sci 17:410–412
Munene G, Parker RD, Larrigan J, Wong J, Sutherland F, Dixon E (2013) Sequential preoperative hepatic vein embolization after portal vein embolization for extended left hepatectomy in colorectal liver metastases. World J Surg Oncol 11:134
Nagino M, Yamada T, Kamiya J, Uesaka K, Arai T, Nimura Y (2003) Left hepatic trisegmentectomy with right hepatic vein resection after right hepatic vein embolization. Surgery 133:580–582
Pomerantz BJ (2009) Biliary tract interventions. Tech Vasc Interv Radiol 12:162–170
De Baere T, Roche A, Elias D, Lasser P, Lagrange C, Bousson V (1996) Preoperative portal vein embolization for extension of hepatectomy indications. Hepatology 24:1386–1391
Guiu B, Bize P, Gunthern D, Demartines N, Halkic N, Denys A (2013) Portal vein embolization before right hepatectomy: improved results using n-butyl-cyanoacrylate compared to microparticles plus coils. Cardiovasc Intervent Radiol. doi:10.1007/s00270-013-0565-7
Scatton O, Plasse M, Dondero F, Vilgrain V, Sauvanet A, Belghiti J (2008) Impact of localized congestion related to venous deprivation after hepatectomy. Surgery 143:483–489
Akamatsu N, Sugawara Y, Kaneko J et al (2003) Effects of middle hepatic vein reconstruction on right liver graft regeneration. Transplantation 76:832–837
Dirsch O, Madrahimov N, Chaudri N et al (2008) Recovery of liver perfusion after focal outflow obstruction and liver resection. Transplantation 85:748–756
Zappa M, Dondero F, Sibert A, Vullierme MP, Belghiti J, Vilgrain V (2009) Liver regeneration at day 7 after right hepatectomy: global and segmental volumetric analysis by using CT. Radiology 252:426–432
van Lienden KP, van den Esschert JW, Rietkerk M et al (2012) Short-term effects of combined hepatic vein embolization and portal vein embolization for the induction of liver regeneration in a rabbit model. J Vasc Interv Radiol 23:962–967
Shindoh J, Truty MJ, Aloia TA et al (2013) Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg 216:201–209
Imamura H, Shimada R, Kubota M et al (1999) Preoperative portal vein embolization: an audit of 84 patients. Hepatology 29:1099–1105
Komori K, Nagino M, Nimura Y (2006) Hepatocyte morphology and kinetics after portal vein embolization. Br J Surg 93:745–751
de Graaf W, van Lienden KP, van den Esschert JW, Bennink RJ, van Gulik TM (2011) Increase in future remnant liver function after preoperative portal vein embolization. Br J Surg 98:825–834
Aknowledgments
The scientific guarantor of this publication is Prof. Boris Guiu. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: retrospective, case-control study, multicenter study.
Authors thank Valérie Macioce for revising the English and Marie-Christine Saint Paul for histological assessment.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Guiu, B., Chevallier, P., Denys, A. et al. Simultaneous trans-hepatic portal and hepatic vein embolization before major hepatectomy: the liver venous deprivation technique. Eur Radiol 26, 4259–4267 (2016). https://doi.org/10.1007/s00330-016-4291-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4291-9