Abstract
Objectives
To identify the clinical significance of primary tumour thickness (TT) and its direction in patients with oral tongue squamous cell carcinoma (OTSCC), we measured TT in all axial/coronal/sagittal views on magnetic resonance imaging (MRI) and evaluated their meaning.
Methods
A total of 53 OTSCC patients were analysed who had undergone preoperative three-dimensional MRI and had been surgically treated. TT measured on axial (mediolateral direction), coronal (superoinferior direction), and sagittal (anteroposterior direction) views was compared to that in pathologic specimens. The association between TT on MRI and other pathologic parameters was also evaluated.
Results
TT on MRI in each plane showed relatively high concordance rates with the histological measurements. TT in all three planes was significantly correlated with lymph node (LN) metastasis. Occult LN metastasis was found in 15 of 39 (38.5 %) patients, and the cutoff value of TT in axial/coronal/sagittal MRI predicting occult LN metastasis was 6.7 mm, 7.2 mm, and 12.3 mm, respectively. TT on MRI did not show any significant association with recurrence and survival.
Conclusions
TT on MRI in all three planes showed relatively high coincidence with TT on histopathology and presented a potential cut-off value as a predictive indicator for occult LN metastasis.
Key Points
• Three-dimensional measurement of tumour thickness (TT) is important for oral cancer treatment.
• Magnetic resonance imaging (MRI) is a useful diagnostic tool for oral cancer.
• TT on MRI has a high coincidence with TT on histopathology.
• TT on MRI is a predictive marker for occult lymph node metastasis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Oral cavity cancer (OCC) consists of more than 26,000 cases of incident cancers in the United States alone, and an estimated 263,900 new patients and 128,000 deaths occur annually from OCC worldwide [1, 2]. The oral tongue is the most common primary site of OCC, and squamous cell carcinoma represents the majority of the pathologic types. Oral tongue squamous cell carcinoma (OTSCC) has a relatively unfavourable prognosis despite recent improvements in treatment modalities and in early cancer detection methods [3]. Its poor prognosis may be caused by the anatomical characteristics of the oral tongue. The oral tongue only consists of muscular structures without a strong barrier for preventing tumour propagation. Additionally, the lymphovascular system around the oral tongue is relatively well developed, so there may be a high risk of metastases to adjacent structures and to cervical lymph nodes (LN) [4].
The Tumour-Node-Metastasis (TNM) staging system of the American Joint Committee of Cancer (AJCC) defines tumour stage by the largest tumour diameter and invasion of the surrounding structures [5]. To date, TNM is still the most commonly utilized system for diagnosis and treatment planning for OCC. However, many reports have demonstrated the limitations of the conventional TNM staging system as a prognosticator for OCC, and various clinicopathological parameters—including tumour thickness (TT) and depth of invasion (DOI) [6]—have been introduced for better prediction of patient survival outcomes [7]. A recent study also focused on the problem of the T4a stage in the conventional TNM staging system; namely, that the styloglossus and hyoglossus consist of extrinsic tongue muscles superficial to and near the lateral oral tongue and that tumour invasion to those muscles should be re-considered from T4a staging [8]. Therefore, developing a new risk stratification system may be necessary, especially when considering the primary tumour features on the preoperative radiographs for appropriate treatment planning.
Magnetic resonance imaging (MRI) is considered the most useful imaging modality for prediction of tumour size in OCC [9]. Park et al. reported that preoperative MRI measurement of the degree of involvement of the primary tumour in the oral cavity and oropharynx showed excellent correlations with the surgical specimen [10]. On the other hand, because the tumour is a three-dimensional feature, the definition of tumour thickness (TT) and DOI should be considered not only in terms of the lengths, but also the tumour extent in the anterior-posterior, superior-inferior, and medial-lateral directions. This may better represent the extent (i.e., ‘how much’ and ‘where to’) of invasion of OCC and will be a very important factor in deciding the range of surgery and predicting prognosis.
In this study, we identified the thickness and direction of primary tumour propagation using MRI including all of the axial-plane, coronal-plane, and sagittal-plane images to evaluate the potential clinical significance of using a three-dimensionally measured TT in patients with OTSCC. Contrary to previous reports, which were merely focused on the correlation between pathologic TT and occult LN metastasis, this is the first report of the positive impact of using a three-dimensionally measured TT from MRI on the recurrence and survival of OTSCC patients.
Materials and methods
Patients
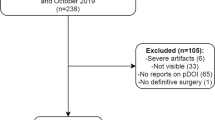
A total of 118 OTSCC patients diagnosed and treated with a curative intent in our tertiary referral hospital between 2005 and 2012 were initially included. Patients with history of prior therapy (n = 4), distant metastases at initial diagnosis (n = 7), primary tumour resection only (n = 10), unclear pathologic reports (n = 16), or inadequate clinical follow-up data (n = 17) were excluded from the study. Additionally, 11 patients were excluded because of a lack of a pretreatment MRI in all three planes or an impossible measurement (e.g., a very small/superficial lesion, unclear tumour demarcation, dental artefact) of the primary tumour. Therefore, 53 patients were included in the final analysis. This study was reviewed and approved by the Institutional Review Board of our hospital, and informed consent from each patient was waived.
Treatments and follow-up
All patients received a radical resection of the primary tumour with 1–1.5 cm resection margins and combined neck dissection (ND). Patients without clinical nodal metastasis underwent selective ND including levels I–III or I–IV. Modified radical or radical ND involving levels I–V was performed in the patients with metastatic LN. A bilateral ND was done if primary tumours crossed the midline of tongue or a contralateral neck metastasis was suspected. High-risk patients, such as those with an advanced-stage or with adverse pathologic features, received postoperative radiotherapy (RT) or concurrent chemoradiotherapy (CRT). Patients were scheduled for regular clinic visits after the completion of initial treatment. If an index cancer recurrence on clinical or radiological findings was suspected during follow-up, the diagnosis was confirmed by biopsy and specific additional diagnostic tests. All of the study subjects were followed more than one year, and patients with a recurrence were scheduled for salvage or palliative treatment.
Measurement of TT on MRI
All preoperative MRI was performed using the same machine (Achieva, Philips Medical Systems, Amsterdam, Netherlands) possessing a 3 Tesla scanner and an eight-channel head coil. All images were obtained in the axial/coronal/sagittal planes. All of the TT measurements were performed on T2-weighted images (T2WI), because differentiating the tumour mass from peritumoural inflammation or post-biopsy changes was easier compared to contrast-enhanced T1-weighted images (T1WI). Axial T2-weighted imaging was performed with the following parameters: repetition time (TR) = 4487.2 msec; effective echo time (effective TE) = 100 msec; flip angle = 90°; number of signal averages (NSA) = 2; echo train length (ETL) = 70; number of encoding steps = 300; matrix = 300 × 300 (reconstruction matrix = 512 × 512); voxel size = 0.69 × 0.69 × 0.69 mm3; slice thickness = 3.0 mm; spacing between slices = 0.0 mm; SENSE factor = 1.8. Coronal and sagittal T2-weighted imaging was performed with the following parameters: TR = 5550.8 msec; effective TE = 70.7 msec; flip angle = 90°; NSA = 2; ETL = 70; number of encoding steps = 300; matrix = 300 × 300 (reconstruction matrix = 512 × 512); voxel size = 1 × 1 × 1 mm3; slab number = 1; slab thickness = 40 mm; slice thickness = 4.0 mm; spacing between slices = 1.0 mm; SENSE factor = 2.5. A single radiologist (*blinded*) specializing in head and neck diseases performed the measurements, and no clinicopathological information was given to the interpreter before the analysis. The protocol of TT measurement was as follows: the reference line was defined as the longest tumour diameter anteroposteriorly on the axial view, mediolaterally on the coronal view, and superoinferiorly on the sagittal view, respectively. TT was obtained from the summation of the distance of the perpendicular line from the reference line to the deepest infiltration point and to the most projecting point of tumour. Therefore, TT demonstrates the tumour extent of infiltration mediolaterally on the axial view, superoinferiorly on the coronal view, and anteroposteriorly on the sagittal view, respectively. Representative images are illustrated in Fig. 1.
Measurement of tumour thickness (TT) on MRI. The reference line was defined as the longest tumour diameter anteroposteriorly on the axial view (a), mediolaterally on the coronal view (b) and superoinferiorly on the sagittal view (c), respectively. TT was obtained from the summation of the distance of the perpendicular line from the reference line to the deepest infiltration point (a) and to the most projecting point (b) of tumour
Variables
Clinical data, including age at the time of diagnosis, gender, smoking history, alcohol intake, initial treatments, and follow-up information (e.g., recurrence of tumour and patient deaths according to the causes), were obtained from patient medical records. A heavy smoker was defined as a patient with a smoking history ≥ 20 pack-years, and one drink of alcohol was defined as 15.6 mL of pure ethanol [11]. The postoperative pathologic findings containing primary tumour size, histological TT, grade, margin status, perineural invasion (PNI), lymphovascular invasion (LVI), LN involvement, and pathologic TNM stage were also investigated.
Statistical analysis
The relationship between TT measured on MRI and on pathological specimens was estimated using Bland-Altman plot. Logistic regression analysis was used for the comparison between TT on MRI and other pathologic parameters. The cutoff value of TT for predicting nodal status was determined by a receiver operation characteristic (ROC) curve analysis. Analyses of the relationship between clinicopathologic parameters and disease-free survival (DFS)/specific survival (DSS) were performed using a Cox proportional hazards model. The hazard ratios (HR) and 95 % confidence intervals (CI) were calculated. All statistical analyses were performed using IBM SPSS software version 21.0 (IBM Corp., Armonk, NY). A two-sided p value < 0.05 was considered statistically significant.
Results
Patient characteristics
The clinicopathological characteristics of the patients are summarised in Table 1. They consisted of 26 men and 27 women with a median age of 48 (range, 25–76) years. All of the primary tumours were located in the oral tongue lateral border. On the preoperative MRI, 20 (37.7 %) patients had an advanced T stage, and extrinsic tongue muscle (ETM) invasion was also suspected in 20 (37.7 %) patients. The median TT of the primary tumours on axial/coronal/sagittal images was 10.6 (range, 4.0–34.9) mm, 11.9 (4.1–30.3) mm, and 18.5 (4.3–47.4) mm, respectively. Pathologic findings were also evaluated, and the resection margin was involved in four (7.5 %) patients. PNI and LVI were found in ten (18.9 %) and seven (13.2 %) patients, respectively. Fifteen (28.3 %) patients had a pathologically advanced T stage, and a positive cervical LN was identified in 28 (52.8 %) patients.
Forty-one (77.4 %) patients, including 39 initially without clinical nodal metastasis, underwent ipsilateral ND and another 12 (22.6 %) patients received bilateral ND. Thirty-three (62.2 %) patients were treated with postoperative RT or CRT with a median of 60 Gy (range, 42–74 Gy) administered in a single daily fraction. During a median follow-up of 44 (range, 13–119) months recurrences were found in 17 (32.1 %) patients [locoregional (n = 15) and distant (n = 7), with mutual overlap between them]. Of the 15 (28.3 %) identified deaths at the last follow-up, 14 (26.4 %) patients died of the index OTSCC, and one died of a non-cancerous cause.
Correlation of TT on MRI with clinicopathological parameters
TT measured on MRI mediolaterally on the axial view, superoinferiorly on the coronal view, and anteroposteriorly on the sagittal view were compared to the comparable lengths in the pathologic specimen. Bland-Altman plot on each comparison showed relatively significant correlation within the 95 % limits of agreement (Fig. 2).
Correlation of tumour thickness (TT) between MRI data and the specimens. TT measured on MRI mediolaterally on the axial view (a), superoinferiorly on the coronal view (b) and anteroposteriorly on the sagittal view (c) were compared to the corresponding distances in the pathologic specimen. Bland-Altman plot on each comparison showed relatively significant correlation within the 95 % limits of agreement
We also evaluated the association between TT on MRI and other pathologic parameters. TT on the axial view showed significant correlation with LN metastasis [odds ratio (OR) 1.152, 95 % CI 1.038–1.277, p = 0.007] and LVI (OR 1.130, 95 % CI 1.017–1.254, p = 0.023). TT on the coronal view presented a greater risk of LN metastasis (OR 1.177, 95 % CI 1.052–1.316, p = 0.004) and LVI (OR 1.122, 95 % CI 1.004–1.253, p = 0.041). Finally, TT on the sagittal view had strong association with LN metastasis (OR 1.132, 95 % CI 1.042–1.231, p = 0.004) and positive margin (OR 1.104, 95 % CI 1.005–1.213, p = 0.038).
The possible association between TT and ETM invasion on MRI was also analysed, and ETM invasion was identified in 20 patients [styloglossus (n = 14), palatoglossus (n =12), hyoglossus (n = 9), and genioglossus (n = 6), with some of them mutually overlapped]. ETM invasion showed significant positive correlations with TT measured on all three planes, medial-lateral (OR = 1.231, 95 % CI 1.092–1.388, p = 0.001), superior-inferior (OR = 1.268, 95 % CI 1.108–1.451, p = 0.001), and anterior-posterior (OR = 1.179, 95 % CI 1.070–1.300, p = 0.001), respectively (Table 2).
Association of TT on MRI with occult LN metastasis
The number of clinically node-negative patients at initial diagnosis was 39, and occult LN metastases were found in 15 (38.5 %) of these cases. Figure 3 shows the ROC curves reflecting the association between TT and occult LN metastasis. The area under the ROC curve was 0.750 for TT in the medial-lateral direction on the axial view, 0.753 for TT in the superior-inferior direction on the coronal view, and 0.750 for TT in the anterior-inferior direction on the sagittal view, respectively. The cutoff value of TT on the axial/coronal/sagittal MRI predicting occult LN metastasis was 6.7 mm, 7.2 mm, and 12.3 mm, respectively (p < 0.05).
Receiver operation characteristic (ROC) curves reflecting the association between tumour thicknesses (TT) measured on MRI and occult lymph node (LN) metastasis. The area under the ROC curve (AUC) was 0.750 in TT in the medial-lateral direction on the axial view (a), 0.753 in TT in the superior-inferior direction on the coronal view (b), and 0.750 in TT in the anterior-inferior direction on the sagittal view (c). The cut-off values of the TT in axial/coronal/sagittal MRI predicting occult LN metastasis were 6.7 mm, 7.2 mm, and 12.3 mm, respectively. All cut-off values were statistically significant (P < 0.05)
Predictive findings on recurrence and survival of the OTSCC patients
We sought to find the prognostic significance of TT on a preoperative MRI in terms of recurrence (i.e., DFS) and cancer-specific death (i.e., DSS) of OTSCC patients. Table 3 demonstrates the associations between parameters measured on MRI and DFS/DSS of the patients; however, TT did not have significant impact on recurrence or survival. Other MRI findings including tumour size, ETM invasion, and tumour stage also had no meaningful association with DFS/DSS. Only the presence of a LN metastasis showed statistical significance in both recurrence and cancer-specific death.
Other clinicopathologic parameters affecting index cancer recurrence were TT measured in the anterior-posterior direction in the specimen (HR = 1.042, 95 % CI 1.008–1.078, p = 0.016), a positive margin (HR = 6.113, 95 % CI 1.717–21.759, p = 0.005), and a pathologic LN metastasis (HR = 1.042, 95 % CI 1.008–1.078, p = 0.016). OTSCC-specific death was significantly affected by TT measured in the specimen in the superior-inferior direction (HR = 1.084, 95 % CI 1.013–1.161, p = 0.020) and in the anterior-posterior direction (HR = 1.056, 95 % CI 1.017–1.096, p = 0.005), a positive margin (HR = 7.033, 95 % CI 1.918–25.797, p = 0.003), and a pathologic LN metastasis (HR = 6.737, 95 % CI 1.505–30.167, p = 0.013, Table 4).
Discussion
Of the patients with OTSCC, 76 % and 74 % are expected to achieve 5-year DFS and DSS, respectively. TNM stage, TT, and extranodal extension are known as prognostic factors for OTSCC [12]. Having an elevated TT or DOI can bring about an increasing cervical LN metastasis rate even in early T-staged OTSCC and may also serve as an independent prognostic factor [13]. The concept of TT primarily originated from histopathologic measurements [14]. However, preoperative imaging would be necessary in order to determine the surgical extent including the primary tumour and ND. Therefore, there have been various techniques using ultrasound, computed tomography, or MRI for preoperative evaluation of TT in OCC [15].
Previous studies about TT on MRI usually measured TT as the medial-lateral length in an axial view [9, 15, 16]. However, the direction of tumour progression may be variable, and identifying the location of the invasion front of the tumour into adjacent structures, such as lymphatics, vasculature, nerve, and bone is very important. Okura et al. reported that TT and the distance to the paralingual space (i.e., the space between the genioglossus and intrinsic tongue muscles) measured in the MRI coronal view had a predictable value for cervical LN metastasis in OTSCC [17]. The affected area is located under the intrinsic tongue muscles with plenty of lymphoneurovascular structures, and consequently, is a crucial channel to the cervical space for tumour metastasis. Therefore, TT on MRI should be considered not only on an axial view, but on all three planes, as in our study.
In this study, we newly defined reference lines in each plane of MRI for three-dimensional measurement of TT. The universal concept of TT indicates extent of tumour penetration perpendicularly to the long axis of the tumour growing along the epithelial surface of lateral border of tongue (i.e., epicentre of origin), but according to this definition, measurement of TT with anterolateral and of superoinferior directions will be virtually impossible. Another debatable point of our study is the use of T2WI instead of gadolinium-enhanced T1WI for TT measurement on MRI. Because inflammatory or post-biopsy changes as well as tumour mass can be well-enhanced by contrast agent, tumour size might be overestimated on contrast-enhanced T1WI, especially in the oral cavity, which is prone to secondary inflammation from ulceration or combined infection. Therefore, we used high resolution T2WI rather than contrast-enhanced T1WI to measure more exact TT in our study.
We also evaluated herein the correlations between TT on preoperative MRI and other clinicopathologic parameters. First, we identified the relevance of TT in surgical specimens and found a relatively high coincidence among them in all three planes with a linear relationship. Larger TT is associated with a greater risk of ETM invasion and cervical LN metastasis. We hypothesized that LVI risk would be elevated if TT increased in the medial-lateral or superior-inferior direction for tumours located on the lateral border of the tongue, and the results of this study support that hypothesis. Another notable outcome is that a positive margin is more frequently found in patients with a larger anterior-posterior TT. Head and neck surgeons usually focus on acquiring a safe, deep margin with regard to the medial-lateral TT, but there would be a risk of overlooking submucosal extent of TT in the anterior-posterior and superior-inferior directions, as we found in our study.
Our study shows that ETM invasion is more frequently found with increasing TT on MRI. However, both ETM invasion and TT itself do not affect recurrence or survival of the patients. ETM invasion of tumour is defined as T4a stage according to the AJCC TNM staging system, regardless of tumour size or TT. Patients with a T4a stage tumour are recommended to receive postoperative adjuvant treatment [18]. The problem at this point is that it would be hard to distinguish ETM from intrinsic tongue muscles in the dissected surgical specimens. Consequently, pathologists occasionally refer to the radiologic description to define ETM invasion from a pathologic finding with skeletal muscle involvement. Therefore, decisive demarcation of ETM invasion and its clinical significance are needed for better patient treatment outcomes.
Occult LN metastasis rate in OTSCC is approximately 42 % even in an early T1/T2 staged tumour, and elective ND is routinely recommended [19, 20]. There have been many reports about the impact of TT on occult cervical LN metastasis in OCC, and diverse cutoff values of TT in a surgical specimen have been suggested as an indicator for an elective ND [21]. On the other hand, articles related to MRI have reported various values of TT ranging from 6.0–9.7 mm for predicting occult LN metastasis [10, 16, 17]. Differences between MRI and histology may be due to shrinkage of tissue and peritumoural inflammation signals on the images [9]. In this study, 15 of 39 (38.5 %) patients with clinically negative nodal status had pathologically positive cervical LN metastasis. We can define the cutoff values of TT on MRI for prediction of occult LN metastasis as 6.7 mm, 7.2 mm, and 12.3 mm in the axial, coronal, and sagittal planes. Our results are in line with previous studies, and these cut-off values will be helpful to determine the need for elective ND in OTSCC and postoperative follow-up of the patients.
In our study, LN metastasis detected by both MRI and pathology was observed to be a crucial prognostic factor for recurrence and survival, and the significance of cervical LN involvement in OCC is well known [6, 12]. LN metastasis is affected by TT of the primary tumour, and therefore, we assumed that TT would be an independent prognostic factor associated with recurrence and cancer-specific survival and that the significance of TT on each MRI plane would be different. However, we do not find any statistical significance of TT on recurrence and survival.
The above negative result might be due to a relatively small study population and limited MRI values including image artefacts. In addition, relatively short time for clinical application of three-dimensional scanning including sagittal view on MRI and lack of follow-up data on the subjects would be another cause. Additionally, there may be overlooking of other interrelated factors influencing the patients’ prognosis as well as TT. We did not compare the predictive significance of TT on each of the three planes, nor did we perform a multivariate analysis on DFS and DSS due to a lack of compatibility in the data from the univariate analyses. However, our study is the first report to analyse tumour extent in terms of length plus direction on a three-dimensionally measured preoperative MRI in patients with OTSCC. TT on MRI in all three planes shows relatively high coincidence with TT on histopathology, and presents a potential cutoff value as a good predictive indicator for occult LN metastasis. Head and neck oncologic surgeons should keep TT in all three dimensions in mind, and make a proper plan for primary tumour resection with ND referring to the results of this study.
Abbreviations
- AJCC:
-
American Joint Committee of Cancer
- CI:
-
Confidence interval
- CRT:
-
Chemoradiotherapy
- DFS:
-
Disease-free survival
- DOI:
-
Depth of invasion
- DSS:
-
Disease-specific survival
- ETL:
-
Echo train length
- ETM:
-
Extrinsic tongue muscle
- HR:
-
Hazard ratio
- LN:
-
Lymph node
- LVI:
-
Lymphovascular invasion
- NSA:
-
Number of signal averages
- OCC:
-
Oral cavity cancer
- OR:
-
Odds ratio
- OTSCC:
-
Oral tongue squamous cell carcinoma
- PNI:
-
Perineural invasion
- ROC:
-
Receiver operation characteristic
- RT:
-
Radiotherapy
- TE:
-
Echo time
- TNM:
-
Tumour-Node-Metastasis
- TR:
-
Repetition time
- TT:
-
Tumour thickness
References
Jemal A, Bray F, Centre MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Koo BS, Lim YC, Lee JS, Choi EC (2006) Recurrence and salvage treatment of squamous cell carcinoma of the oral cavity. Oral Oncol 42:789–794
Chen MK, Chen CM, Lee MC, Chen LS, Chen HC (2011) Primary tumor volume is an independent predictor of outcome within pT4a-staged tongue carcinoma. Ann Surg Oncol 18:1447–1452
Edge SB, Byrd DR, Compton CC, Fritz AG, Green FL, Trotti A (2010) AJCC cancer staging manual, 7th edn. Springer-Verlag, New York
Pentenero M, Gandolfo S, Carrozzo M (2005) Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: a review of the literature. Head Neck 27:1080–1091
Okuyemi OT, Piccirillo JF, Spitznagel E (2014) TNM staging compared with a new clinicopathological model in predicting oral tongue squamous cell carcinoma survival. Head Neck 36:1481–1489
Boland PW, Pataridis K, Eley KA, Golding SJ, Watt-Smith SR (2013) A detailed anatomical assessment of the lateral tongue extrinsic musculature, and proximity to the tongue mucosal surface. Does this confirm the current TNM T4a muscular subclassification? Surg Radiol Anat 35:559–564
Lam P, Au-Yeung KM, Cheng PW et al (2004) Correlating MRI and histologic tumor thickness in the assessment of oral tongue cancer. AJR Am J Roentgenol 182:803–808
Park JO, Jung SL, Joo YH, Jung CK, Cho KJ, Kim MS (2011) Diagnostic accuracy of magnetic resonance imaging (MRI) in the assessment of tumor invasion depth in oral/oropharyngeal cancer. Oral Oncol 47:381–386
Hashibe M, Brennan P, Benhamou S et al (2007) Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst 99:777–789
Rogers SN, Brown JS, Woolgar JA et al (2009) Survival following primary surgery for oral cancer. Oral Oncol 45:201–211
Melchers LJ, Schuuring E, van Dijk BA et al (2012) Tumour infiltration depth >/=4 mm is an indication for an elective neck dissection in pT1cN0 oral squamous cell carcinoma. Oral Oncol 48:337–342
O’Brien CJ, Lauer CS, Fredricks S et al (2003) Tumor thickness influences prognosis of T1 and T2 oral cavity cancer—but what thickness? Head Neck 25:937–945
Lwin CT, Hanlon R, Lowe D et al (2012) Accuracy of MRI in prediction of tumour thickness and nodal stage in oral squamous cell carcinoma. Oral Oncol 48:149–154
Iwai H, Kyomoto R, Ha-Kawa SK, Lee S, Yamashita T (2002) Magnetic resonance determination of tumor thickness as predictive factor of cervical metastasis in oral tongue carcinoma. Laryngoscope 112:457–461
Okura M, Iida S, Aikawa T et al (2008) Tumor thickness and paralingual distance of coronal MR imaging predicts cervical node metastases in oral tongue carcinoma. AJNR Am J Neuroradiol 29:45–50
National Comprehensive Cancer Network. Head and Neck Cancers, Version 2. Available via http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed 2 Sept 2014
Ho CM, Lam KH, Wei WI, Lau SK, Lam LK (1992) Occult lymph node metastasis in small oral tongue cancers. Head Neck 14:359–363
Ferlito A, Silver CE, Rinaldo A (2009) Elective management of the neck in oral cavity squamous carcinoma: current concepts supported by prospective studies. Br J Oral Maxillofac Surg 47:5–9
Huang SH, Hwang D, Lockwood G, Goldstein DP, O’Sullivan B (2009) Predictive value of tumor thickness for cervical lymph-node involvement in squamous cell carcinoma of the oral cavity: a meta-analysis of reported studies. Cancer 115:1489–1497
Acknowledgments
The scientific guarantor of this publication is Prof. Soon Yuhl Nam. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. None of the study subjects or cohorts have been previously reported. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kwon, M., Moon, H., Nam, S.Y. et al. Clinical significance of three-dimensional measurement of tumour thickness on magnetic resonance imaging in patients with oral tongue squamous cell carcinoma. Eur Radiol 26, 858–865 (2016). https://doi.org/10.1007/s00330-015-3884-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3884-z