Abstract
Objective
The hyperintense acute reperfusion marker (HARM) on fluid-attenuated inversion recovery (FLAIR) images is associated with blood-brain barrier (BBB) permeability changes. The aim of this study was to examine the influence of contrast agent dosage on HARM incidence in acute ischaemic stroke patients.
Methods
We prospectively included 529 acute ischaemic stroke patients (204 females, median age 71 years). Patients underwent a first stroke-MRI within 24 hours from symptom onset and had a follow-up on day 2. The contrast agent Gadobutrol was administered to the patients for perfusion imaging or MR angiography. The total dosage was calculated as ml/kg body weight and ranged between 0.04 and 0.31 mmol/kg on the first examination. The incidence of HARM was evaluated on day 2 FLAIR images.
Results
HARM was detected in 97 patients (18.3 %). HARM incidence increased significantly with increasing dosages of Gadobutrol. Also, HARM positive patients were significantly older. HARM was not an independent predictor of worse clinical outcome, and we did not find an association with increase risk of haemorrhagic transformation.
Conclusions
A higher dosage of Gadobutrol in acute stroke patients on initial MRI is associated with increased HARM incidence on follow-up. MRI studies on BBB should therefore standardize contrast agent dosages.
Key Points
• Hyperintense acute reperfusion marker on MRI indicates blood-brain barrier disruption.
• This observational study on stroke patients characterizes HARM.
• Incidence depends on contrast agent dosage on the previous day.
• HARM is also associated with older age and poor kidney function.
• Interpretation of HARM must take dosage into consideration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In a proportion of acute stroke patients, hyperintensities in the cerebrospinal fluid (CSF) filled spaces can be observed on fluid-attenuated inversion recovery (FLAIR) images [1, 2]. In 2012, Köhrmann and colleagues showed that these hyperintensities stem from significant amounts of MR contrast agent in the CSF, which hamper the signal suppression of water on FLAIR images [3]. Gadobutrol and other clinically used Gadolinium-containing MR contrast agents have a considerable molecular size; their transfer across the intact blood-brain barrier (BBB) is unlikely [4]. Therefore, this marker is considered a sign for early BBB permeability changes and was termed “hyperintense acute reperfusion marker” (HARM) in previous studies. HARM is associated with reperfusion of the initially occluded vessels [5, 6] and seems to occur more often in elderly [5]. Data on association of HARM with an increased risk of haemorrhagic transformation are scarce and rather inconsistent. While some groups found an increased risk of haemorrhages in patients showing HARM [5, 7], others could not prove this association [6, 8]. Nevertheless, HARM could still be considered as a potential MRI biomarker for haemorrhagic complications or unfavourable outcome in the course of ischaemic stroke. It would imply possible therapeutic consequences such as protection of the BBB, adequate blood pressure management or handling of anticoagulation in patients with acute stroke and early BBB disruption.
The impact of contrast agent dosage on incidence of HARM has not been studied yet. The usual dosage of Gadolinium-containing contrast agents for perfusion imaging is 0.1 mmol/kg body weight [9]. At our centre we apply fixed contrast agent volumes for perfusion MRI and contrast enhanced MR angiography irrespective of individual body weight. However, in the clinical routine the total dosage of contrast agent often varies greatly between patients, due to the need of application of additional contrast agent-based MRI sequences. In this study, we therefore examined the influence of the total dosage of Gadobutrol on the incidence of HARM in a large cohort of acute stroke patients. We hypothesize that dosage (measured in mmol/kg body weight) has an impact on the incidence of HARM. Clarification of this matter may help interpretation of the relevance of HARM in the clinical context and implicate the importance of dosage in design of future studies on BBB disruptions.
Methods
Patients
Data was acquired as part of the 1000 Plus study [10]. This study was approved by the local ethics committee and registered on clinicaltrials.gov (NCT00715533). All patients gave written informed consent. We prospectively included consecutive acute stroke patients that had a MRI examination within 24 h from symptom onset and a follow-up MRI examination on day 2. Exclusion criteria were MRI contraindications, a history of renal failure, and age under 18 years.
Image acquisition
The MRI examinations were performed on a 3 Tesla MRI (TRIO TIM; Siemens AG, Germany). All included patients underwent an MRI examination with our standard stroke protocol, which includes diffusion-weighted imaging (DWI) to confirm the diagnosis of stroke, T2*-weighted imaging to evaluate haemorrhages, FLAIR, time-of-flight MR angiography, and perfusion imaging (PI). Sequence parameters for the FLAIR images were: TE = 100 ms; TR = 8000 ms; matrix size = 256 × 256; FOV = 220 mm; and 25 transversal slices with a slice thickness of 5 mm.
All patients received PI with a fixed dosage of 5 ml Gadovist® (Gadobutrol, 1 M, Bayer Schering Pharma AG, Berlin, Germany) followed by a 20 ml intravenous saline flush when weighing 50-100 kg. Only if patients’ weight was below 50 kg or above 100 kg, 4 ml or 6 ml of contrast agent was injected, respectively. Due to clinical reasons, approximately half of the included patients underwent contrast enhanced MR angiography during the same examination and received an additional 5 to 6 ml of contrast agent. A minority of the patients received a follow-up MRI examination on the same day about 2-4 h after the first examination, adding even further doses of contrast agent. We calculated the total dosage received by the patients on the first day in mmol and in dependence of the body weight of the patients.
Image analysis and clinical data collection
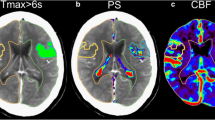
HARM was evaluated on day 2 FLAIR images that were acquired approximately 24 h after the last contrast agent administration. An experienced rater (M.R.) was instructed to judge if sulci or ventricles showed hyperintensities compared to the baseline FLAIR image that was acquired before contrast agent administration. When these hyperintensities were observed on more than two consecutive slices and were not confounded by artefacts, patients were considered HARM positive. For image examples, see Fig. 1. We evaluated T2*-weighted images for new haemorrhagic transformations (HT) and parenchymal haemorrhages (PH) and specifically excluded subarachnoid haemorrhage as a reason for the observed hyperintensities in all HARM positive patients. The DWI lesion volumes and volumes of hypoperfusion were delineated with MRIcro (version 1.4, © Chris Rorden). Final infarct volumes were determined on FLAIR images on day 5-7. National Institutes of Health Stroke Scale (NIHSS) scores were assessed on day 1, modified Rankin Scale (mRS) scores were, if possible, determined after three months. As an estimate for kidney function, the glomerular filtration rate (GFR) was calculated from serum creatinine using the Modification of Diet in Renal Disease formula [11].
Statistical tests
Statistics was performed using SPSS (version 21; IBM, USA). Differences between HARM positive and HARM negative patients were tested for imaging and clinical parameters that were likely to have an impact on HARM according to recent studies. The Chi-square or Fisher’s exact test was used for nominal data and the Mann-Whitney U test for ordinal and metric data. All parameters that significantly differed between groups in the univariate analysis were additionally entered in a binary logistic regression analysis to determine the independent predictors of HARM. In the same manner, we performed a univariate analysis and binary logistic regression to predict the independent predictors of outcome at three months. To simplify the interpretation, the dosage of contrast agent was used as mmol per kg body weight, and these values were multiplied by 100 before being entered in the logistic regression.
The reported p-values are 2-tailed and uncorrected. The level of significance was fixed at a p-value < 0.05 for all tests.
Results
General
We included 529 patients with the confirmed diagnosis of ischaemic stroke. All patients were examined with perfusion imaging on the first day. Additional contrast agent-based MR angiography during the same examination was applied in 229 patients (43.29 %). Twenty-five (4.73 %) of the patients received a follow-up examination on the same day. This resulted in contrast agent dosages ranging between 0.04 and 0.31 mmol/kg body weight in the whole cohort. Demographical data on our whole cohort are listed in Table 1.
Differences between HARM groups
Of all 529 patients, 97 (18.3 %) showed HARM on the follow-up examination. Details on the differences between HARM positive and HARM negative patients as well as p-values can be found in Table 2. The HARM positive patients were significantly older (p < 0.001) and received more contrast agent on the previous day (p < 0.001), compared to HARM negative patients (see also Fig. 2). Furthermore, HARM was associated with a lower GFR (p = 0.002) and HARM positive patients showed a trend towards larger DWI volumes (p = 0.05). Only age and dosage remained as significant independent predictors of HARM in the binary logistic regression (p < 0.001 for both variables).
Association of HARM and outcome
The HARM positive patients had significantly higher mRS at three months (2 (IQR 0-4) versus 1 (IQR 0-2), p = 0.002). In the binary logistic regression (including age, gender, thrombolysis treatment, recanalization, HARM, DWI , PI volumes, and NIHSS at baseline) only age (OR of 1.052, 95 % CI 1.022 – 1.082, p = 0.001), NIHSS (OR of 1.165, 95 % CI 1.076 – 1.263, p < 0.001), and perfusion volumes at baseline (OR of 1.005, 95 % CI 1.001 – 1.009, p = 0.025) were significant independent predictors of outcome. HARM did not predict a worse outcome in this model.
We also found no significant difference between HARM positive and HARM negative patients in the number of patients showing HT or PH: HT occurred in 31 (7.2 %) of HARM negative versus seven (7.2 %) of HARM positive patients (p = 1.000). PH occurred in eight (1.9 %) of HARM negative versus five (5.2 %) of HARM positive patients (p = 0.70).
In 93 patients (17.6 %) intravenous thrombolysis was administered as standard treatment. HARM occurred in 73 (16.7 %) of the non-treated patients and in 24 (25.8 %) of the thrombolysed patients (p = 0.054). In thrombolysed patients alone, there was no association between HT and HARM (p = 0.550).
Discussion
HARM has previously been shown to be a reperfusion marker [5, 7] and a potential indicator of HT. Therefore, thorough knowledge about this phenomenon, its clinical implication, and impact on future research and diagnostics concerning early BBB disruption in the course of acute stroke is warranted. HARM is a quite common observation in acute ischaemic stroke patients, with incidences of 30-40 % in previous studies [5, 7, 8]. In our study, the incidence of HARM was 18.3 %. Since we showed that HARM is also associated with the size of the initial lesion, the relatively small lesion sizes in our cohort might be a reason why we found a lower incidence of HARM compared to other studies.
It has been previously shown that age is a factor associated with HARM, and we were able to replicate those findings. Moreover, we found that a reduced kidney function is correlated with increased incidence of HARM.
Furthermore, increasing dosages of contrast agent administered on the first day lead to a considerable increase in the proportions of patients with HARM on follow-up. With both higher administered dosages and reduced kidney function, relevant amounts of contrast agent remained in the bloodstream in higher concentration. This might enable Gadobutrol molecules to pass the BBB and achieve sufficient concentration to be visible on FLAIR.
To our knowledge, this is the first study reporting a dose-dependent occurrence of hyperintensities on FLAIR images in larger cohorts of stroke patients. The only animal study on this topic contained case reports on healthy animals [12]. Considering how strong the dosage influences the incidence of HARM, we recommend that studies on HARM should always control and report the dosage of contrast agent administered to the patients. We are aware that in the acute clinical setting, this is difficult to implement, since the kind and number of contrast agent-based examinations is determined by clinical needs. Therefore, we state that HARM should always be interpreted carefully taking into consideration the age and contrast agent dosages of the patients.
In the whole cohort of 529 patients, we found no significant association between HARM and the occurrence of HT or PH. The entire incidence of HT and PH was relatively low, and therefore the results have to be interpreted with caution. However, if HARM was a direct predictor of increased risk for bleeding, we would expect the incidence of HT und PH in our cohort to be higher.
Overall, we found significant differences in clinical outcome between HARM positive and HARM negative patients, regardless of the dosage administered. These results are in line with previous studies on HARM [7]. However, the higher age of the HARM positive patients might be the more dominating factor, leading to poor recovery rates and a worse outcome. After all, a worse clinical outcome at three month was predicted by age and baseline NIHSS, but not by HARM. Whether HARM could be a potential surrogate for biological ageing or loss of resistance against ischaemic stress, requires further studies.
With this study, we primarily aimed to characterize HARM as precisely as possible and to analyse the parameters that have an impact on its incidence. However, our goal was not to determine the prognostic value of HARM. With this study, we provide a good basis of knowledge on how age and contrast agent dosage influence the incidence of HARM. This should facilitate implementation and interpretation of future studies on the clinical relevance of BBB disruptions in ischaemic stroke.
Abbreviations
- HARM:
-
Hyperintense acute reperfusion marker
- FLAIR:
-
Fluid-attenuated inversion recovery
- CSF:
-
Cerebrospinal fluid
- BBB:
-
Blood-brain barrier
- DWI:
-
Diffusion-weighted imaging
- PI:
-
Perfusion imaging
- HT:
-
Haemorrhagic transformation
- PH:
-
Parenchymal haemorrhage
- NIHSS:
-
National Institutes of Health Stroke Scale
- mRS:
-
Modified Rankin Scale
- GFR:
-
Glomerular filtration rate
References
Dechambre SD, Duprez T, Grandin CB et al (2000) High signal in cerebrospinal fluid mimicking subarachnoid haemorrhage on FLAIR following acute stroke and intravenous contrast medium. Neuroradiology 42:608–611
Stuckey SL, Goh TD, Heffernan T, Rowan D (2007) Hyperintensity in the subarachnoid space on FLAIR MRI. Am J Roentgenol 189:913–916
Köhrmann M, Struffert T, Frenzel T et al (2012) The hyperintense acute reperfusion marker on fluid-attenuated inversion recovery magnetic resonance imaging is caused by gadolinium in the cerebrospinal fluid. Stroke J Cereb Circ 43:259–261
Ewing JR, Knight RA, Nagaraja TN et al (2003) Patlak plots of Gd-DTPA MRI data yield blood– brain transfer constants concordant with those of 14C-sucrose in areas of blood–brain opening. Magn Reson Med 50:283–292
Warach S, Latour LL (2004) Evidence of reperfusion injury, exacerbated by thrombolytic therapy, in human focal brain ischemia using a novel imaging marker of early blood-brain barrier disruption. Stroke J Cereb Circ 35:2659–2661
Hjort N, Wu O, Ashkanian M et al (2008) MRI detection of early blood-brain barrier disruption - Parenchymal enhancement predicts focal hemorrhagic transformation after thrombolysis. Stroke 39:1025–1028
Latour LL, Kang D-W, Ezzeddine MA et al (2004) Early blood-brain barrier disruption in human focal brain ischemia. Ann Neurol 56:468–477
Rozanski M, Ebinger M, Schmidt WU et al (2010) Hyperintense acute reperfusion marker on FLAIR is not associated with early haemorrhagic transformation in the elderly. Eur Radiol 20:2990–2996
Manka C, Träber F, Gieseke J et al (2005) Three-dimensional dynamic susceptibility-weighted perfusion MR imaging at 3.0 T: feasibility and contrast agent dose. Radiology 234:869–877
Hotter B, Pittl S, Ebinger M et al (2009) Prospective study on the mismatch concept in acute stroke patients within the first 24 h after symptom onset - 1000Plus study. BMC Neurol. doi:10.1186/1471-2377-9-60
Levey AS, Bosch JP, Breyer Lewis J et al (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 130:461–470
Mamourian AC, Hoopes PJ, Lewis LD (2000) Visualization of intravenously administered contrast material in the CSF on fluid-attenuated inversion-recovery MR images: an in vitro and animal- model investigation. AJNR 21:105–111
Acknowledgements
The scientific guarantor of this publication is Jochen B. Fiebach. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding from the Federal Ministry of Education and Research via the Grant Center for Stroke Research Berlin (01EO0801 and 01EO1301). No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all patients in this study. Methodology: prospective, observational study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ostwaldt, AC., Rozanski, M., Schaefer, T. et al. Hyperintense acute reperfusion marker is associated with higher contrast agent dosage in acute ischaemic stroke. Eur Radiol 25, 3161–3166 (2015). https://doi.org/10.1007/s00330-015-3749-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3749-5