Abstract
Objectives
To evaluate patient acceptance of noninvasive imaging tests for detection of coronary artery disease (CAD), including single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI), stress perfusion magnetic resonance imaging (MRI), coronary CT angiography (CTA) in combination with CT myocardial stress perfusion (CTP), and conventional coronary angiography (CCA).
Methods
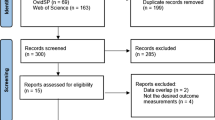
Intraindividual comparison of perception of 48 patients from the CORE320 multicentre multinational study who underwent rest and stress SPECT-MPI with a technetium-based tracer, combined CTA and CTP (both with contrast agent, CTP with adenosine), MRI, and CCA. The analysis was performed by using a validated questionnaire.
Results
Patients had significantly more concern prior to CCA than before CTA/CTP (p < 0.001). CTA/CTP was also rated as more comfortable than SPECT-MPI (p = 0.001). Overall satisfaction with CT was superior to that of MRI (p = 0.007). More patients preferred CT (46 %; p < 0.001) as a future diagnostic test. Regarding combined CTA/CTP, CTP was characterised by higher pain levels and an increased frequency of angina pectoris during the examination (p < 0.001). Subgroup analysis showed a higher degree of pain during SPECT-MPI with adenosine stress compared to physical exercise (p = 0.016).
Conclusions
All noninvasive cardiac imaging tests are well accepted by patients, with CT being the preferred examination.
Key Points
• A variety of cardiac imaging tests is available without known patient preference
• CTA/CTP shows a lower degree of concern than conventional coronary angiography
• CTA/CTP shows higher overall satisfaction compared to stress perfusion magnetic resonance imaging
• CTA/CTP is rated as more comfortable than SPECT-MPI
• CTA/CTP is the preferred cardiac imaging test
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary computed tomography angiography (CTA) noninvasively detects significant coronary stenoses with high sensitivity in patients with a low to intermediate pretest likelihood of coronary artery disease (CAD) [1–3] compared to conventional coronary angiography (CCA) as the reference standard.
The clinical outcome of patients with CAD is mainly determined by the presence of myocardial ischemia, which is often determined by nuclear imaging tests [4]. While there is a positive correlation between the degree of stenosis and reduced myocardial perfusion [5], CCA as an anatomic test does not allow reliable identification of myocardial ischemia [6, 7]. Myocardial ischemia and viability can be detected by both single-photon emission CT myocardial perfusion imaging (SPECT-MPI) and stress perfusion magnetic resonance imaging (MRI) [8, 9]. Compared to SPECT-MPI, CT myocardial stress perfusion (CTP) with adenosine administration shows good correlation in detecting perfusion abnormalities [10–13] and may, on this account, increase the diagnostic accuracy of CTA alone as an additional predictor of the functional relevance of a stenosis diagnosed by CTA [13–17]. Therefore, these four imaging tests, CTA/CTP, SPECT-MPI, MRI, and CCA are complementary.
Besides the diagnostic accuracy of a clinical test, patient acceptance is an important requirement before a test can be implemented in clinical routine. In general, patient-centred care may improve communication, compliance, and finally, clinical outcome of patients [18]. Several studies analysed the acceptance of noninvasive diagnostic imaging tests [19–22]. However, only a few studies addressed cardiac imaging, and those studies found greater patient preference for CT than for CCA for imaging of the coronary arteries [19, 23]. CCA was characterised by higher pain levels [19] and a higher incidence of adverse effects [23] compared to CTA. Studies analysing patient acceptance of CTA compared to coronary MR angiography and CCA [19] found CTA to be experienced as more comfortable in comparison to CCA and coronary MR angiography, while both MR angiography and CTA had lower pain levels than CCA. However, stress MR perfusion imaging and SPECT-MPI were not analysed in these previous studies and no study addressed patient satisfaction with CTP.
The objective of this study was, therefore, to compare intraindividually patient acceptance of four noninvasive imaging-based tests for detection of CAD: CTA/CTP, SPECT-MPI, stress perfusion MRI, and CCA.
Methods
Study design
This is a single-centre ancillary study of a multicentre trial [24–26]. Briefly, the multicentre study included patients who underwent combined CT, including CTA and CTP with administration of adenosine, rest and stress SPECT-MPI with a technetium-based tracer, and CCA for the analysis of the diagnostic accuracy in detecting significant coronary stenoses and myocardial perfusion deficits. In addition to these three tests, the patients in this substudy also underwent cardiac MRI with adenosine stress provocation. Physicians provided oral and written information on each test beforehand, and they informed the patients also about the research nature of the protocol. The examinations were performed within a maximum of 60 days, and CTA/CTP was always performed as the second to last examination before CCA. For the analysis of patient acceptance, the patients were administered a validated questionnaire 24 h after CCA. The study protocol was approved by the local ethics committees; all patients gave written informed consent for the analysis of patient acceptance, and also for the global research including the four tests. The steering committee of the multicentre study approved the analysis plan and manuscript of this ancillary study.
Study population and CT examination
In this single-centre substudy we approached 49 consecutive patients with known or suspected CAD and a clinical indication for CCA for participation in this patient preference study. If the heart rate was higher than 60 beats per minute (bpm), 75 mg of metoprolol (body mass index <30 kg/m2) or 150 mg of metoprolol (body mass index ≥30 kg/m2) was administered orally. An IV injection of metoprolol was additionally given in patients with a persistent heart rate above 60 bpm (2.5 – 5.0 mg every 5 min; maximum dose of 15 mg). Rest CTA was performed before CTP using 320-slice CT (Aquilion One, Toshiba Medical Systems, Tokyo, Japan). Nitroglycerin was administered sublingually if systolic blood pressure was >110 mmHg. The total dose of contrast agent (Isovue 370, Bracco Diagnostics, Monroe Township, NJ, USA) was 50 – 70 ml, dependent on the patient’s body weight [24]. The IV infusion of adenosine (Adenosin Life Medical, Carinopharm, Elze, Germany, 140 μg/kg/min) for subsequent CTP was performed 20 min after nitroglycerin administration. Four minutes after the beginning of the adenosine administration, the scanner settings were adjusted following the protocol and current heart rate [24], and the scan with contrast agent administration was initiated at 4:30 min. During adenosine administration, a physician monitored the patient.
SPECT myocardial perfusion imaging
SPECT-MPI was performed as a 1-day protocol or 2-day protocol (Table 1) by using Tc-99 m tracer with a mean dose of 377 ± 202 MBq (rest acquisition) and 285 ± 21 MBq (stress acquisition). Stress was induced pharmacologically in nine patients (60 ± 17 mg adenosine; 0.14 mg/kg body weight/min) and by physical exercise (treadmill) in 40 patients (127 ± 35 W; one patient underwent both pharmacological and physical stress). Images were acquired with a gamma camera (GE Sophy or Siemens Symbia R 10). The mean duration of the stress provocation was 469 ± 152 s.
Magnetic resonance myocardial perfusion imaging
Each patient underwent MRI at 1.5 Tesla (Magnetom Sonata, Siemens Medical Solutions, Erlangen, Germany) using a 32-channel dedicated surface breast coil. The patients laid supine and wore ear protection during the procedure. Patients with known claustrophobia did not undergo MRI. If necessary, the patients got blankets for their thermal comfort. Cine steady-state free precession sequences were acquired in the three long and short axes of the heart through the left ventricle. For myocardial stress perfusion, adenosine was administered (140 μg/kg/min over 4:30 min). Myocardial rest perfusion followed afterwards. After contrast agent injection (Magnevist; 0.1 mmol Gd/kg) for both the stress and rest phase, phase-sensitive inversion recovery sequences in the short and long heart axes were acquired for delayed enhancement imaging without additional contrast agent administration.
Conventional coronary angiography
In each case, CCA was performed after CTA/CTP. A transfemoral approach was used in 44 patients (92 %; radial artery approach in four patients; Table 1) by using 223 ± 64 μg nitroglycerin (Lidoject, Hexal AG, Holzkirchen, Germany). Additional measurement of fractional flow reserve (FFR) during CCA with adenosine injection was performed in eight patients (17 %). A mean amount of contrast agent of 138 ± 75 ml, including interventional procedures if necessary, was administered for CCA (Xenetix 350, Villepinte, France). If a vascular closure device (AngioSeal, St. Jude Medical, MN, USA; Starclose und Perclose, Abbott Laboratories, IL, USA) was used, the patients had to lie flat for 4 – 6 h. After manual compression, the bed rest time was 12 h. The pressure tourniquet was removed 2 h after placement of the closure device and 6 h after manual compression.
The questionnaire
The patients were handed the validated acceptance questionnaire (Appendix) 24 h after CCA. The questionnaire asked about patients’ subjective perceptions during the four examinations: CTA/CTP, SPECT-MPI, stress perfusion MRI, and CCA. By using an ordinal 5-point scale including the options “very good”, “good”, “moderate”, “poor”, and “very poor”, the patients evaluated preparation and information, comfort, and overall satisfaction. To assess the degree of concern, the degree of helplessness, and problems with the stress medication adenosine, the patients could choose from a 5-point scale including “no”, “little”, “moderate”, “intense”, and “very intense”. Additionally, the patients stated their willingness to undergo the tests again by using an ordinal scale including “no”, “yes”, and “don’t know”. The degree of pain was evaluated on a 100-mm unmarked visual analog scale (VAS). For CTA/CTP, the patients were asked to mark in different colours the amount of pain caused by CTA and CTP. Additionally, the patients could choose one of the four examinations as their preferred clinical test for future diagnostic examinations. Using free texts, the patients gave their subjective reasons for their degree of concern as well as advantages and disadvantages of each examination. For the comparison of CTA and CTP, the patients could state the degree of concern and their willingness to undergo the tests again as described above. Additionally, the occurrence of angina pectoris or dyspnoea during CTA and CTP was assessed with an ordinal scale including “yes” and “no”.
Statistical analysis
The values are given as mean ± standard deviation. First of all, an overall test was done, including the four examinations, SPECT-MPI, CTA/CTP, MRI, and CCA. For the analysis of the degree of pain, the analysis of variance (ANOVA) test for repeated measures was used for the examinations as multiple dependent variables. The Friedman test was used as an overall test for the ordinal and nominal variables preparation and information, comfort, overall satisfaction, degree of concern, degree of helplessness, problems with adenosine, and willingness to undergo the tests again. Only if the overall analyses showed a p-value ≤0.05, which was considered statistically significant, the following single tests were performed for each variable. The t-test for dependent variables was used for analysis of the degree of pain. For nominal and ordinal variables, the signs test was used. Preference was evaluated using the chi-square test. A p-value ≤0.008 was defined statistically significant after Bonferroni correction because of multiple testing for the following comparisons: SPECT-CT, SPECT-MRI, SPECT-CCA, CT-MRI, CT-CCA, and MRI-CCA. As an additional parameter for overall satisfaction, assessment of the variables preparation and information, concern, comfort, and degree of helplessness was summed. The possible sum ranged from 4 to 20 points, with a lower number of points indicating better assessment. Statistical analysis was performed according to the analysis of ordinal and nominal variables. The subgroup analyses were performed with the chi-square test, the t-test for independent variables, and the Mann-Whitney U test for preference, degree of pain, and ordinal and nominal variables, respectively. Statistical significance was defined for a p-value ≤0.05. The statistical analysis was performed using SPSS version 21.
Results
Patient population
Forty-nine patients underwent all four diagnostic tests. The questionnaire was completed by 48 patients (98 % response rate). The one patient who did not answer the questionnaire presented with atypical angina pectoris and had no history of prior myocardial infarction. He underwent no intervention during CCA. The included patients had a mean age of 64 years (64 ± 19.1 years) with a female-to-male ratio of 1:2 (Table 1). Eight patients had a prior myocardial infarction (17 %). CTA/CTP was performed on average 0.6 ± 3.0 days before MRI, and CCA was conducted 7.9 ± 7.5 days after CTA/CTP. PCI during the CCA was indicated in 15 patients, whereas 33 patients received no intervention during the CCA.
Patient acceptance
Preparation and information were rated as good or very good for both SPECT-MPI and CT by 47 patients (98 %), and for both MRI and CCA by 46 patients (96 %). There was no significant difference between the four tests (Table 2). More than half of the patients stated no or little concern before the diagnostic tests. Concern was lower for CTA/CTP as compared to CCA (p < 0.001). The comparison between CTA/CTP and MRI showed no significant difference. Regarding CT, the degree of concern was higher for CTP compared to CTA (p < 0.001). Reasons were the possible complications of adenosine during CTP and fear of the results of CTA. More than 90 % of the patients rated the comfort for each clinical examination as very good or good. CTA/CTP was rated as more comfortable than SPECT-MPI (p = 0.001). Forty-seven patients (98 %), 45 patients (94 %), 40 patients (83 %), and 41 patients (85 %) felt no or little helplessness during SPECT-MPI, CT, MRI, and CCA, respectively. The comparison of the degree of helplessness during the four examinations revealed no significant difference (Table 2). The sum of these four variables showed a significant advantage of CTA/CTP over SPECT-MPI (p = 0.001), MRI (p = 0.005), and CCA (p ≤ 0.001), which is consistent with the trends suggested by the results when each question is analysed separately.
Pain and adverse events
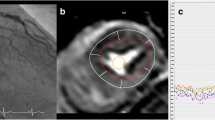
Forty-five patients (94 %) had pain during at least one diagnostic test (Fig. 1). The comparison of the pain between SPECT-MPI, CTA/CTP, MRI, and CCA showed no significant difference (p = 0.182). For combined CTA/CTP, CTP was characterised by higher pain levels than CTA (p < 0.001). CTP caused angina pectoris more frequently (n = 14) compared to CTA (n = 1; p < 0.001). There was no significant difference of the dyspnoea and combined dyspnoea with angina pectoris between the CTA and the CTP (p = 0.317 and p = 0.125). The problems with adenosine, as reflected by the occurrence of angina pectoris or dyspnoea during SPECT-MPI, CT, MRI, and CCA, were without significant difference (p = 0.118).
a Boxplot of pain intensity during combined coronary computed tomography angiography and CT myocardial stress perfusion (CTA/CTP), single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI), stress perfusion magnetic resonance imaging (MRI), and conventional coronary angiography (CCA). The repeated measures ANOVA test was used for overall analysis with the different diagnostic tests as multiple dependent variables. The degree of pain showed no significant difference between the four diagnostic tests (p = 0.182). b Intraindividual comparison of the 45 patients who felt pain during at least one examination
Overall satisfaction and preference
The overall satisfaction with SPECT-MPI, CT, MRI, and CCA was rated as very good or good by 44 (92 %), 46 (96 %), 46 (96 %), and 47 patients (98 %), respectively (Table 2). Overall satisfaction with CTA/CTP was superior to MRI (p = 0.007). More patients preferred CT (p < 0.001; Fig. 2) to SPECT-MPI, MRI, and CCA. Respectively, 81 %, 85 %, 67 %, and 67 % of the patients were willing to undergo SPECT-MPI, CT, MRI and CCA again. Comparison between the four tests showed no significant difference. The willingness to undergo CTA again for future diagnostic evaluation was higher than that for CTP (98 % versus 77 %; p < 0.001).
Patient preference for each diagnostic test. All patients were asked to state which of the four tests they would prefer for future cardiac diagnostic imaging: single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI), stress perfusion magnetic resonance imaging (MRI), combined coronary computed tomography angiography and CT myocardial stress perfusion (CTA/CTP), or conventional coronary angiography (CCA). Nearly half of the patients preferred CT to all three other tests (p < 0.001 by using chi-square test)
Open-ended questions
For SPECT-MPI and CTA/CTP, patients named more advantages than disadvantages (Table 3). The most frequent advantage of SPECT-MPI was the noninvasiveness, followed by the short duration of the clinical test, and the absence of hospitalisation. In the patients’ view, the limited diagnostic accuracy was the most common disadvantage of SPECT-MPI, followed by the long duration of the diagnostic test. The most frequently listed advantages for CTA/CTP were the noninvasiveness and the diagnostic accuracy of the test. The most frequently mentioned disadvantages were the limited diagnostic accuracy and administration of adenosine. For MRI and CCA, our patients listed more disadvantages than advantages. The additional diagnostic benefit and the noninvasiveness were frequently stated advantages of the MRI. The disadvantages of MRI experienced by our patients were the discomfort caused by slight claustrophobia due to the confined space of the bore and the long duration of the clinical examination. Diagnostic accuracy was the most frequently given advantage of CCA, followed by the short duration. Invasiveness was the most often given disadvantage, followed by the long laying time.
Subgroup analysis
In our patient population, there were 17 women (35 %) and 31 men (65 %). Gender had no significant influence on preference in our patient collective (p = 0.502). Pain was higher for women during SPECT-MPI and CT than for men (p = 0.026 and 0.010; Table 4). The occurrence of angina pectoris showed no correlation with problems with adenosine, pain, or helplessness during SPECT-MPI, CT, MRI, and CCA (Table 4). The pain during CCA was slightly higher in patients with percutaneous coronary intervention (PCI) compared to the patients without an intervention, but without a significant difference. A prior diagnosis of CAD showed no statistical correlation with pain, comfort, preparation, or overall satisfaction for CCA. The pain, the willingness to undergo the examination again, the comfort, and overall satisfaction with CCA were not significantly different between the patients with and without FFR (Table 4). The method of stress provocation during SPECT-MPI showed no relevant influence on comfort, helplessness, and overall satisfaction during SPECT-MPI (p = 0.478, p = 0.667, p = 0.901), whereas the degree of pain during SPECT-MPI was higher with adenosine stress compared to the use of physical stress (p = 0.016).
Discussion
Most patients in our study preferred CTA/CTP for future cardiac diagnostic examinations. CT showed a lower degree of concern than CCA and higher overall satisfaction compared to MRI and CTA/CTP was rated as more comfortable than SPECT-MPI. The sum of the variables concern, preparation, comfort, and helplessness showed an advantage of CTA/CTP over SPECT-MPI, MRI, and CCA. Regarding combined CTA/CTP, CTP was characterised by a higher degree of concern and a higher pain score on the VAS than CTA alone.
Interestingly, in our analysis, approximately half of the patients preferred combined CTA/CTP, while only 2 % preferred stress perfusion MRI for future evaluation of the coronary arteries. In contrast, pain, degree of concern, degree of helplessness, and comfort showed no significant differences between CTA/CTP and MRI. Reasons for this discrepancy were identified in the free text analysis; the discomfort and claustrophobia induced by the narrow MR gantry as well as the long duration of the examination were the most common disadvantages of MRI. This is in line with the higher overall satisfaction and sum of preparation, concern, comfort, and helplessness we found for CT in comparison to MRI in our patient collective and may explain the higher preference for CT. Interestingly, CT was also rated as slightly more comfortable than MRI, but without significant difference. Despite the high acceptance of combined CTA/CTP, the patients had a higher degree of pain and more frequently suffered angina pectoris during CTP compared to CTA. Additionally, patients were more concerned about CTP than about CTA. The main cause of concern was adenosine administration during CTP.
Comparison with prior studies
While the noninvasive imaging-based tests for detection of CAD have high diagnostic accuracy and may predict outcomes in patients with CAD, only a few studies compared patient acceptance. In cardiovascular imaging, patient-centred care including patient safety and patient involvement in decision making gains in importance [27]. An intraindividual comparison of 122 patients in the context of a study of Sandgaard et al. [23] showed a higher preference for coronary CT angiography against CCA and a lower presence of adverse effects during CT compared to CCA. A study of Schönenberger et al. compared patient satisfaction with CTA, MR angiography, and CCA. In this study CTA was evaluated as more comfortable than MR angiography and CCA, and the patients preferred CTA as a future method for imaging the coronary arteries. Both CTA and MR angiography were less painful than CCA. While in our study CT was also the preferred clinical examination, there was no significant difference between pain and comfort experienced during CTA/CTP, perfusion MRI, and CCA in our patient collective. A relevant reason for this discrepancy is that no adenosine was used during coronary CT and MR angiography in the study of Schönenberger et al. Mumma et al. showed a lower willingness to undergo CCA for women than for men [20]. In our patient collective, gender had no relevant influence on the acceptance of CCA or preference, although women experienced more severe pain during SPECT-MPI and CTA/CTP than men. In contrast to the study of Mumma et al., our patients underwent CTP and SPECT-MPI with adenosine administration or with physical stress, which could be a reason for the higher pain levels reported by women during the noninvasive tests compared to men. In general, adenosine has a high safety profile and is well tolerated by patients [28].
Limitations
An important limitation is the small number of only 48 patients analysed in our study. Nevertheless, we performed an intraindividual comparison of all four cardiac imaging tests in all 48 patients. For such an analysis, lower patient numbers are sufficient for statistical analysis than in cohort studies where only some of the patients underwent one test and other patients a different test. Patient acceptance may be influenced by the temporal sequence of the tests or by the moment when the test was handed. However, the CCA as a diagnostic test and also as a therapy option is usually performed after a noninvasive test. Thus, the CCA can not only be seen as an independent option. Moreover, the questionnaire could consider which combined examination with CCA would be chosen for the patient. All patients underwent CTP and stress perfusion MRI with adenosine administration, whereas only one fifth of the patients had combined CCA with FFR using adenosine and SPECT-MPI with pharmacologic stress (80 % of the patients had physical stress during SPECT-MPI). While our subgroup analysis showed no influence of the FFR on pain, comfort, overall satisfaction, and willingness to undergo CCA again, FFR could have influenced the acceptance of CCA. In addition, approximately one third of the patients had a PCI during the CCA. The necessity of a PCI might have influenced the patient acceptance. So, patients with PCI mentioned slightly higher pain levels during the CCA as compared to the patients without PCI. Different physicians explained the clinical examinations and obtained informed consent from the patients, which might also have influenced patients’ ratings of information and evaluation as well as the degree of concern but reflects clinical routine.
Conclusion
This study shows a higher preference for noninvasive cardiac imaging-based tests compared to CCA, among which CT was the preferred diagnostic test in our patient collective. CT was experienced to be more comfortable than SPECT-MPI. Additionally, CTA/CTP showed an overall satisfaction superior to that of MRI and a lower degree of concern compared to CCA.
Abbreviations
- bpm:
-
Beats per minute
- CAD:
-
Coronary artery disease
- CCA:
-
Conventional coronary angiography
- MRI:
-
Stress perfusion magnetic resonance imaging
- CTA:
-
Coronary computed tomography angiography
- CTP:
-
Computed tomography myocardial stress perfusion
- FFR:
-
Fractional flow reserve
- IV:
-
Intravenous
- PCI:
-
Percutaneous coronary intervention
- SPECT-MPI:
-
Single-photon emission computed tomography myocardial perfusion imaging
- VAS:
-
Visual analog scale
References
Dewey M, Zimmermann E, Deissenrieder F, Laule M, Dübel HP et al (2009) Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 120:867–875
Nasis A, Leung MC, Antonis PR, Cameron JD, Lehman SJ et al (2010) Diagnostic accuracy of noninvasive coronary angiography with 320-detector row computed tomography. Am J Cardiol 106:1429–1435
de Graaf FR, Schuijf JD, van Velzen JE, Kroft LJ, de Roos A et al (2010) Diagnostic accuracy of 320-row multidetector computed tomography coronary angiography in the non-invasive evaluation of significant coronary artery disease. Eur Heart J 31:1908–1915
Beller GA, Zaret BL (2000) Contributions of nuclear cardiology to diagnosis and prognosis of patients with coronary artery disease. Circulation 101:1465–1478
Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T et al (1994) Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med 330:1782–1788
Di Carli MF, Dorbala S, Curillova Z, Kwong RJ, Goldhaber SZ et al (2007) Relationship between CT coronary angiography and stress perfusion imaging in patients with suspected ischemic heart disease assessed by integrated PET-CT imaging. J Nucl Cardiol 14:799–809
Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG et al (2006) Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation 114:1761–1791
Paterson I, Mielniczuk LM, O’Meara E, So A, White JA (2013) Imaging heart failure: current and future applications. Can J Cardiol 29:317–328
Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J et al (2012) Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 379:453–460
Nasis A, Ko BS, Leung MC, Antonis PR, Nandurkar D et al (2013) Diagnostic accuracy of combined coronary angiography and adenosine stress myocardial perfusion imaging using 320-detector computed tomography: pilot study. Eur Radiol 23:1812–1821
George RT, Arbab-Zadeh A, Miller JM, Vavere AL, Bengel FM et al (2012) Computed tomography myocardial perfusion imaging with 320-row detector computed tomography accurately detects myocardial ischemia in patients with obstructive coronary artery disease. Circ Cardiovasc Imaging 5:333–340
Wang Y, Qin L, Shi X, Zeng Y, Jing H et al (2012) Adenosine-stress dynamic myocardial perfusion imaging with second-generation dual-source CT: comparison with conventional catheter coronary angiography and SPECT nuclear myocardial perfusion imaging. AJR Am J Roentgenol 198:521–529
Rochitte CE, George RT, Chen MY, Arbab-Zadeh A, Dewey M et al (2014) Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J 35:1120–1130
Hosokawa K, Kurata A, Kido T, Shikata F, Imagawa H et al (2011) Transmural perfusion gradient in adenosine triphosphate stress myocardial perfusion computed tomography. Circ J 75:1905–1912
Schuijf JD, Wijns W, Jukema JW, Atsma DE, de Roos A et al (2006) Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol 48:2508–2514
Ko SM, Choi JW, Hwang HK, Song MG, Shin JK et al (2012) Diagnostic performance of combined noninvasive anatomic and functional assessment with dual-source CT and adenosine-induced stress dual-energy CT for detection of significant coronary stenosis. AJR Am J Roentgenol 198:512–520
Rief M, Zimmermann E, Stenzel F, Martus P, Stangl K et al (2013) Computed tomography angiography and myocardial computed tomography perfusion in patients with coronary stents: prospective intraindividual comparison with conventional coronary angiography. J Am Coll Cardiol 62:1476–1485
Keirns CC, Goold SD (2009) Patient-centered care and preference-sensitive decision making. JAMA 302:1805–1806
Schönenberger E, Schnapauff D, Teige F, Laule M, Hamm B et al (2007) Patient acceptance of noninvasive and invasive coronary angiography. PLoS One 2:e246
Mumma BE, Baumann BM, Diercks DB, Takakuwa KM, Campbell CF et al (2011) Sex bias in cardiovascular testing: the contribution of patient preference. Ann Emerg Med 57:551–560.e554
Achiam MP, Løgager V, Chabanova E, Thomsen HS, Rosenberg J (2010) Patient acceptance of MR colonography with improved fecal tagging versus conventional colonoscopy. Eur J Radiol 73:143–147
Liedenbaum MH, de Vries AH, Gouw CI, van Rijn AF, Bipat S et al (2010) CT colonography with minimal bowel preparation: evaluation of tagging quality, patient acceptance and diagnostic accuracy in two iodine-based preparation schemes. Eur Radiol 20:367–376
Sandgaard NC, Diederichsen AC, Petersen H, Høilund-Carlsen PF, Mickley H (2012) Patients’ views of cardiac computed tomography angiography compared with conventional coronary angiography. J Thorac Imaging 27:36–39
George RT, Arbab-Zadeh A, Cerci RJ, Vavere AL, Kitagawa K et al (2011) Diagnostic performance of combined noninvasive coronary angiography and myocardial perfusion imaging using 320-MDCT: the CT angiography and perfusion methods of the CORE320 multicenter multinational diagnostic study. AJR Am J Roentgenol 197:829–837
Vavere AL, Simon GG, George RT, Rochitte CE, Arai AE et al (2011) Diagnostic performance of combined noninvasive coronary angiography and myocardial perfusion imaging using 320 row detector computed tomography: design and implementation of the CORE320 multicenter, multinational diagnostic study. J Cardiovasc Comput Tomogr 5:370–381
Cerci RJ, Arbab-Zadeh A, George RT, Miller JM, Vavere AL et al (2012) Aligning coronary anatomy and myocardial perfusion territories: an algorithm for the CORE320 multicenter study. Circ Cardiovasc Imaging 5:587–595
Einstein AJ, Berman DS, Min JK, Hendel RC, Gerber TC et al (2014) Patient-centered imaging: shared decision making for cardiac imaging procedures with exposure to ionizing radiation. J Am Coll Cardiol
Cerqueira MD, Verani MS, Schwaiger M, Heo J, Iskandrian AS (1994) Safety profile of adenosine stress perfusion imaging: results from the Adenoscan Multicenter Trial Registry. J Am Coll Cardiol 23:384–389
Acknowledgements
The scientific guarantor of this publication is Professor Marc Dewey. The authors of this manuscript declare relationships with the following companies: Prof. Dewey has received grant support from the Heisenberg Program of the DFG for a professorship (DE 1361/14-1), the FP7 Program of the European Commission for the randomized multicenter DISCHARGE trial (603266-2, HEALTH-2012.2.4.-2), the European Regional Development Fund (20072013 2/05, 20072013 2/48), the German Heart Foundation/German Foundation of Heart Research (F/23/08, F/27/10), the Joint Program from the German Research Foundation (DFG) and the German Federal Ministry of Education and Research (BMBF) for meta-analyses (01KG1013, 01KG1110, 01KG1110), GE Healthcare, Bracco, Guerbet, and Toshiba Medical Systems.
Prof. Dewey has received lecture fees from Toshiba Medical Systems, Guerbet, Cardiac MR Academy Berlin, and Bayer (Schering-Berlex).
Prof. Dewey is a consultant to Guerbet and one of the principal investigators of multi-center studies (CORE-64 and 320) on coronary CT angiography sponsored by Toshiba Medical Systems. He is also the editor of Coronary CT Angiography and Cardiac CT, both published by Springer, and offers hands-on workshops on cardiovascular imaging (www.ct-kurs.de). Prof. Dewey is an associate editor of Radiology and European Radiology.
Institutional master research agreements exist with Siemens Medical Solutions, Philips Medical Systems, and Toshiba Medical Systems. The terms of these arrangements are managed by the legal department of Charité – Universitätsmedizin Berlin. The CORE-320 study has received funding from Toshiba Medical Systems. Two of the authors (FR, RR) have significant statistical expertise. Institutional review board approval was obtained. Written informed consent was obtained from all patients in this study.
The study subjects or cohorts have not been previously reported in regards to patient acceptance. The CORE-320 main study publication in regards to diagnostic accuracy has been published recently be Rochitte et al. (Eur Heart J 2014) and this is a single-centre substudy on the intraindividual patient perception of four cardiac imaging tests. Methodology: prospective, non-randomised controlled trial / intraindividual comparison, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Dewey and E. Schönenberger should be considered equally contributing senior authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 41 kb)
Rights and permissions
About this article
Cite this article
Feger, S., Rief, M., Zimmermann, E. et al. Patient satisfaction with coronary CT angiography, myocardial CT perfusion, myocardial perfusion MRI, SPECT myocardial perfusion imaging and conventional coronary angiography. Eur Radiol 25, 2115–2124 (2015). https://doi.org/10.1007/s00330-015-3604-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3604-8