Abstract
Objectives
To assess diagnostic performance of traction MR arthrography of the hip in detection and grading of chondral and labral lesions with arthroscopic comparison.
Methods
Seventy-five MR arthrograms obtained ± traction of 73 consecutive patients (mean age, 34.5 years; range, 14–54 years) who underwent arthroscopy were included. Traction technique included weight-adapted traction (15–23 kg), a supporting plate for the contralateral leg, and intra-articular injection of 18–27 ml (local anaesthetic and contrast agent). Patients reported on neuropraxia and on pain. Two blinded readers independently assessed femoroacetabular cartilage and labrum lesions which were correlated with arthroscopy. Interobserver agreement was calculated using κ values. Joint distraction ± traction was evaluated in consensus.
Results
No procedure had to be stopped. There were no cases of neuropraxia. Accuracy for detection of labral lesions was 92 %/93 %, 91 %/83 % for acetabular lesions, and 92 %/88 % for femoral cartilage lesions for reader 1/reader 2, respectively. Interobserver agreement was moderate (κ = 0.58) for grading of labrum lesions and substantial (κ = 0.7, κ = 0.68) for grading of acetabular and femoral cartilage lesions. Joint distraction was achieved in 72/75 and 14/75 hips with/without traction, respectively.
Conclusion
Traction MR arthrography safely enabled accurate detection and grading of labral and chondral lesions.
Key Points
• The used traction technique was well tolerated by most patients.
• The used traction technique almost consistently achieved separation of cartilage layers.
• Traction MR arthrography enabled accurate detection of chondral and labral lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Imaging of the central compartment of the hip which includes the labral-chondral interface, articular cartilage layers, and the ligamentum teres is a radiologic challenge [1]. Direct MR arthrography improved the diagnostic accuracy in detection of labral tears compared to native MRI, but there is still room for improvement regarding its low specificity [2] and the definition of reliable imaging criteria [3]. MR imaging of the gradual loss of articular cartilage or cartilage delamination remains difficult with intra-articular contrast administration [4, 5]. Restricted visualization of articular cartilage layers as two distinct layers is a substantial problem inherent to conventional direct MR arthrography. Hence, the application of axial leg traction during MR arthrography was proposed [5, 6]. It has been shown that application of traction using different techniques is technically feasible, but neither technique has been validated with arthroscopy [6, 7].
Thus, the aim of this study was to assess the diagnostic performance of traction MR arthrography of the hip in detection and grading of chondral and labral lesions with arthroscopic comparison.
Material & methods
Patients
This retrospective study was conducted with approval of the institutional review board and a waiver for informed consent. During a period of 10 months (July 2012 – May 2013) 150 consecutive patients with symptoms suggestive for FAI underwent MR arthrography according to the institutional routine protocol. Inclusion criteria were subsequent arthroscopy at the institution. Exclusion criteria were osteoarthritis grade 3 according to the Tönnis classification (Tönnis 0= no signs of osteoarthritis; Tönnis 1= slight narrowing of joint space, slight femoral/acetabular sclerosis; Tönnis 2= small cysts, increasing narrowing of joint space; Tönnis 3= large cysts, severe narrowing of joint space [8]), LCEA <25°, Perthes disease, previous surgery, interval > 6 months between imaging and arthroscopy, and no arthroscopic report of labrum and articular cartilage due to limited arthroscopic accessibility of the central compartment.
Ninety-eight subjects (101 hips) underwent subsequent arthroscopy for treatment of FAI. After exclusion, 75 MR arthrograms of 73 patients remained in the study group (Fig. 1). The study group (mean age, 34.5 years; range, 14–54 years) included 45 men (mean age, 34.2 years; range, 14–53 years) and 28 women (mean age, 35 years; range, 16–54 years). Mean interval between MR arthrography and arthroscopy was 14 weeks (range, 1–26 weeks).
Traction MR arthrography
The used technique for traction MR arthrography was previously described in the literature [7]. Intra-articular injection was performed anterolaterally, under sterile conditions and under fluoroscopic guidance with a 21 G needle. The affected hip was flexed to 5–10 degrees. The injected volume contained 18–27 ml (2–5 ml of local anaesthetic [ropivacaine hydrochloride; 2 mg/mL; Ropinaest; Gebro Pharma, Fieberbrunn, Austria], 1–2 ml of iodinated contrast agent [iopamidol, 200 mg/mL; Iopamiro 200; Bracco, Milan, Italy], 15–20 ml of diluted MR contrast agent [gadopentetate dimeglumine, 2 mmol/L; Magnevist; Bayer Healthcare, Berlin, Germany]). A 1.5 T scanner (Magnetom Symphony; Siemens Medical Solutions, Erlangen, Germany) and large flexible coils were used. An MR-compatible traction device (TRACView; Menges Medical, Gallspach, Austria) was used which consists of a pulley, a cable connected to a weight, and a supporting plate for the contralateral leg. The affected leg was put into a positioning splint and was connected to the traction device with an ankle brace. Traction load was adapted to the patient’s body weight. Fifteen kilograms was used for patients who weighed < 60 kg. Eighteen kilograms was used for patients who weighed 60–80 kg. Twenty-three kilograms was used for patients who weighed > 80 kg. The contralateral leg was stabilized with the foot positioned at the supporting plate to avoid tilting of the pelvis (Fig. 2). The imaging protocol is given in Table 1. MRI under leg traction lasted 19 min. Patients were instructed to terminate the examination at any time if needed. They were instructed to report on neuropraxia and on experienced pain during injection, during MR examination, and after 24 h, respectively. For pain assessment, a score of 0 (no pain) to 10 (unbearable pain) was used.
Distraction of right hip with 23 kg of weight load (1). Fixation with an ankle brace (2) which is connected to the traction device and positioning of the splint (3) for stabilization of the affected extremity. The supporting plate (4) avoids tilting of the pelvis. Traction force is transmitted via a pulley (5) and a cable winch
Arthroscopic hip surgery
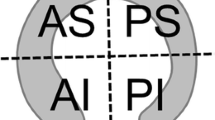
All arthroscopies were performed by two orthopaedic surgeons with 5 years total of experience in hip arthroscopy. A modified version of the arthroscopic MAHORN classification was used for grading of chondral and labral lesions at the time of surgery [9, 10] (Table 2). Localization of acetabular cartilage and labrum lesions was documented as being located anteriosuperiorly, anterioinferiorly, posteriosuperiorly, and posterioinferiorly using a clockface scale [3]. Localization of femoral cartilage lesions was described as anterior or posterior. If more than one lesion was present in the joint the severest damage was documented and used for grading. These classification and localization criteria were used in the initial surgical documentation.
Review of MR arthrograms
Chondral and labral lesions were retrospectively assessed independently by two radiologists with 12 and 5 years of experience in musculoskeletal radiology and who were blinded to the arthroscopic records and to the original interpretations. Only traction sequences were used for assessment of labral and chondral lesions. The same classification as for arthroscopy, adopted for MR, was used to grade labral and chondral lesions (Table 2). Localization of cartilage and labrum lesions was documented in accordance to arthroscopy. The 6 o’clock position was set at the midpoint of the transverse ligament [3]. If more than one lesion was present in the joint, the severest damage was documented and used for grading. Cartilage delamination had to be detectable on two planes. In a second assessment both readers evaluated in consensus whether articular cartilage layers could be differentiated on coronal images obtained with and without traction (Figs. 3, 4 and 5) (Illustrations 1, 2, 3, 4, 5, 6, 7, 8, 9 and 10).
Forty-three-year-old man with cam type FAI (a-c). Coronal T1-weighted fat-suppressed FLASH MR arthrogram (repetition time [TR], 475 ms; echo time [TE], 9.8 ms; flip angle, 60) (a) Without traction cartilage layers could not be differentiated, but complex tear (black and white arrowheads) is detectable. Coronal T1-weighted fat-suppressed traction MR arthrogram (TR, 475 ms; TE, 9.8 ms; flip angle, 60) (b) With traction cartilage layers could be differentiated. Both readers detected delamination tear of the acetabular cartilage (white arrows) and dislocation of intrasubstance labrum component of the complex labral tear (black arrowhead). Sagittal T1-weighted fat-suppressed traction MR arthrogram (TR, 475 ms; TE, 9.8 ms; flip angle, 60) (c) A hyperintense line deep to the acetabular cartilage layers is visible (white arrows)
Thirty-eight-year-old man with mixed type FAI (a-b). Coronal T1-weighted fat-suppressed MR arthrogram (TR, 475 ms; TE, 9.8 ms; flip angle, 60) (a) Without traction cartilage layers could not be differentiated. Coronal T1-weighted fat-suppressed traction MR arthrogram (TR, 475 ms; TE, 9.8 ms; flip angle, 60) (b) With traction cartilage layers could be differentiated. Both readers detected confirmed partial labral tear (white arrow) and hyperintense signal undermining chondral flap (black arrowhead) corresponding to an arthroscopically proven delamination tear
Twenty-nine-year-old woman with mixed type FAI (a-b). Coronal T1-weighted fat-suppressed MR arthrogram (TR, 475 ms; TE, 9.8 ms; flip angle, 60) (a) Without traction cartilage layers were not seen as distinct entities, but labral-chondral separation is detectable (white arrow). Coronal T1-weighted fat-suppressed traction MR arthrogram (TR, 475 ms; TE, 9.8 ms; flip angle, 60) (b) Traction enabled differentiation of intact articular cartilage. Both readers detected hyperintense signal extending between labrum and acetabular rim (white arrow) corresponding to proven partial labrum tear
Statistical analysis
For sensitivity, specificity, positive predicative value, negative predicative value, and accuracy of traction MR arthrography, each with arthroscopy as reference, exact 95 % Clopper-Pearson confidence intervals were calculated. Labral-chondral separation, partial tears, complete tears, intrasubstance tears, and complex tears were defined as abnormal. Loss of less respectively more than 50 % of cartilage thickness, bubble lesions, delamination tears, and cartilage defects were defined as abnormal. Cohen’s Kappa with 95 % confidence intervals was calculated to assess inter-rater agreement between radiologists [11–13]: 0, poor agreement; 0.01–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60 moderate agreement; 0.61–0.80, substantial agreement; 0.81–1.00 excellent agreement. No adjustment for the type I error was made. Hence, confidence intervals and p values are only descriptive. Agreement within one grade was calculated for both readers. This was defined as proportion of arthroscopically confirmed lesions which were graded identically with traction MR arthrography and arthroscopy. Statistical analysis was performed by a biostatistician using the statistical computing software R Version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org).
Results
Traction MR arthrography
No patient asked for termination of the MR examination and no cases of neuropraxia were reported. Seventy-one (71/75 = 95 %; median pain 3; range, 1–9) patients reported on pain during injection. Fifty (50/75 = 67 %; median pain 2; range 1–8) patients reported on pain during MR imaging. Seven (7/75 = 9 %; median pain 1; range 1–5) patients reported on pain on the following day. Femoral and acetabular cartilage layers could be seen as distinct entities in 72 (72/75 = 96 %) cases with traction and in 14 (14/75 = 19 %) cases without traction.
Arthroscopic hip surgery
At arthroscopy 68 labral lesions and 73 chondral (52 acetabular cartilage lesions, 21 femoral cartilage) lesions were identified in 75 hips. Four hips (5 %) did not have any cartilage or labrum lesions. Combined labral and chondral damage was present in 52 (69 %) cases. Labral defects were restricted to one quadrant in 46 hips (68 %) and were distributed as follows: 43 (94 %) anteriosuperior lesions, two (4 %) anterioinferior lesions, one (2 %) posteriosuperior lesions. Twenty-two (32 %) lesions extended over two quadrants: 10 (46 %) lesions were located in the anteriosuperior and anteriorinferior quadrants; 12 (55 %) lesions were located in anteriosuperior and posteriosuperior quadrants. Acetabular cartilage lesions were restricted to one quadrant in 39 (75 %) cases and were distributed as follows: 38 (97 %) anteriosuperior lesions, one (3 %) posteriosuperior lesion, respectively. Thirteen (25 %) acetabular cartilage lesions extended over the anteriosuperior and posteriosuperior quadrant. Femoral cartilage lesions were distributed as follows: nine (43 %) anterior and nine (43 %) posterior lesions; three (14 %) femoral cartilage lesions were located anteriorly and posteriorly.
Diagnostic performance of traction MR arthrography
Accuracy of traction MR arthrography was 92 % for reader 1 and 93 % for reader 2 in detection of labrum lesions. Accuracy of traction MR arthrography was 91 % for reader 1 and 83 % for reader 2 in detection in acetabular cartilage lesions. Accuracy of traction MR arthrography was 92 % for reader 1 and 88 % for reader 2 in detection of femoral cartilage lesions. Results are summarized in Table 3.
Interobserver agreement between readers 1 and 2 was moderate (κ = 0.58, 95 % CI [0.44–0.73], p < 0.001) in the grading of labral integrity. Substantial (κ = 0.7, 95 % CI [0.56–0.83], p < 0.001; κ = 0.68, 95 % CI [0.52–0.84], p < 0.001) agreement was achieved for characterization of acetabular respectively femoral cartilage layers between readers 1 and 2.
Concordance between arthroscopic and MR gradings is illustrated in Table 4. Agreement of traction MR arthrography with arthroscopy within one grade for labrum lesions was 65 % (44/68) for reader 1 and reader 2. Agreement of traction MR arthrography with arthroscopy within one grade for acetabular cartilage lesions was 75 % (39/52) for reader 1 and 65 % (34/52) for reader 2. Agreement of traction MR arthrography with arthroscopy within one grade for femoral cartilage lesions was 67 % (14/21) for both readers.
Discussion
To best of the authors’ knowledge this is the first study which assessed the diagnostic performance of traction MR arthrography. The used technique [7] is different from the one which was described by Llopis and colleagues [6] who applied 6 kg of traction force regardless of the patient’s constitution. More weight (15–23 kg) which was adapted to the patient’s constitution and a supporting plate to avoid pelvic tilt, as proposed previously [14], was used in the current study. Patients with LCEA < 25° were excluded from the study because there was no standardized traction protocol for patients with dysplasia of the hip at the time of the MR examination. Status of cartilage degeneration determines postoperative outcome after hip arthroscopy [15]. Therefore, preoperative imaging should facilitate proper patient selection and treatment. The goal was to present the diagnostic performance of traction MR arthrography in patients with early stages of joint degeneration which are often difficult to detect with conventional MR arthrography [1]. Hence, patients with osteoarthritis (Tönnis grade 3) were excluded from the study.
Most patients reported transient pain which resolved completely after 24 h. There were no cases of neuropraxia. These findings are in accordance with a previous investigation on traction MR arthrography of the hip [7].
In their study with 1,085 patients who underwent direct MR arthrography, Saupe and colleagues [16] showed that the pain experienced did not depend on the volume of injected contrast agent. More volume (18–27 ml) than previously described (8–18 ml) [5, 6, 16, 17] was injected in the current study. Injection of a larger volume of contrast agent combined with traction enables joint distraction in most cases, according to the authors’ experience. This was also the case in the current study (72/75 cases = 96 %). In contrast to previous reports intra-articular injection was made in 5–10 degrees of hip flexion [5, 6, 16, 17]. According to the authors’ experience, this position facilitates intra-articular injection of large volumes of contrast agent which may be explained by the fact that the hip capsular ligaments become more lax with flexion [18]. These observations have to be further investigated.
Some patients reported considerable pain. Pain before the procedure was not assessed. This may falsify some of the reported pain levels in the subset of patients who complained about severe groin pain on the day of the MR examination. Among these individuals, two patients underwent subsequent hip arthroscopy within 1 week. In one case a dislocated labral flap caused acute symptoms, and in another case a massively hypertrophic and torn ligamentum teres required timely arthroscopic treatment. According to a meta analysis [19] on complications inherent to hip arthroscopy, transient neuropraxia of the pudendal, ischial, or femoral nerve is a rare complication which is associated with portal placement, long traction times, and compression of the perineum with the counterpost. Traction time was shorter than mean arthroscopic traction time (19 min versus mean of 51.8 ± 24.2 min) and neither portals nor perineal abutment were needed with the used traction technique. Hence, this procedure is considered to be safe though the investigated cohort was small.
According to a meta analysis by Smith and colleagues, sensitivity and specificity of conventional MR arthrography at 1.5 T in detection of labrum defects is 83 % and 57 %, respectively [2]. Diagnostic performance of traction MR arthrography (sensitivity, 93–97 %; specificity, 57–86 %) in the detection of labrum lesions was comparable with previous results of conventional MR arthrography [4, 20, 21] or non-contrast MRI [22] with sensitivity and specificity values ranging from 85–97 % and 33–100 %, respectively. Prevalence of labrum defects was high among these studies including the current report, hence interpretation of specificity should be made with caution.
Accurate characterization of signal extending into the base of the labrum was difficult in some cases between radiologists and between each radiologist and the arthroscopic gradings. A finding which may be explained by the fact that intersubstance tears may present as focal areas of intermediate signal on T1-weighted images [23]. Furthermore, focal signal alterations or fibrillation were occasionally mistaken for intrasubstance tears (Table 4). One should be aware of these variants when assessing MR arthrograms of the hip.
In the literature, diagnostic performance of MR imaging varies substantially in detection of acetabular cartilage lesions [4, 5, 17, 22, 24, 25].
Predominant pattern of acetabular cartilage lesions were delamination tears in the current study (Table 4; Figs. 3 and 4). Diagnostic studies on cartilage delamination are sparse [5, 26]. Intra-articular injection of contrast agent improved diagnostic performance compared to conventional MRI of the hip in a recent prospective study in the assessment of partial-thickness acetabular cartilage lesions for all surfaces combined with a sensitivity and specificity of 71–92 % and 25–100 %, respectively [4]. In contrast to that, Mintz and coworkers reported a sensitivity, specificity of 91–93 %, 75–85 %, and 86–93 %, 72–88 %, for two readers, respectively, in the evaluation of acetabular femoral cartilage lesions in a cohort of 92 patients on conventional high-resolution MR images [22]. The use of an iterative decomposition of water and fat with echo asymmetry and least squares estimation (IDEAL)-spoiled gradient-recalled echo sequence yielding the advantage of thin contiguous imaging did not improve the combined diagnostic performance of MR arthrography with a sensitivity and specificity of 74 % and 78 %, respectively, in detection of femoroacetabular cartilage lesions compared to conventional sequences [17].
According to previous investigations a subchondral line of high signal intensity is a highly specific, but rare finding on T1- and intermediate-weighted MR arthrograms [5, 26]. Alternatively, hypointense lines within the cartilage on coronal T1- and intermediate-weighted images had a sensitivity and specificity of 35–74 % and 90–95 %, respectively, in the assessment of cartilage delamination [5]. It was hypothesized that femoroacetabular coaptation prevents contrast agent from undermining delaminated cartilage areas [5, 26, 27]. Hence, Pfirrmann and colleagues [5] proposed the application of axial leg traction. Unlike conventional MR arthrography, application of leg traction achieved a sufficient femoroacetabular interface in most patients (Figs. 3, 4 and 5). In the current study, acetabular cartilage lesions were detected with a sensitivity of 85–88 % and a specificity of 78–96 % for both readers on traction MR arthrograms. Traction enabled visualization of subchondral contrast accumulation corresponding to cartilage delamination in most cases (Figs. 3 and 4), a finding which was highly specific for reader 1, whereas the less experienced reader 2 misdiagnosed curvilinear lines within acetabular cartilage as delamination tears in some cases. These findings most likely represent truncation artefacts [28] and emphasize the need for visualization in multiple planes to avoid such pitfalls.
Sensitivity and specificity values of MR arthrography range from 40–83 % and 46–91 %, respectively, in detection of femoral cartilage layers [4, 24, 25]. Femoral cartilage lesions were detected with a sensitivity and specificity of 81–86 % and 91–94 %, respectively, for both readers on traction MR arthrograms. These results are comparable with the findings of Mintz and colleagues [22].
There are several limitations of this study inherent to the retrospective study design. The arthroscopists were aware of the initial radiologic report which could have led to a potential bias. Although the presented results are encouraging, direct comparison between conventional MR arthrography and traction MR arthrography is needed to evaluate whether the application of axial leg traction improves detection of chondral and labral lesions. This was not possible since the used protocol only included multiplanar imaging for traction imaging.
In conclusion traction MR arthrography safely achieved separation of articular cartilage layers and enabled accurate detection and grading of labral and chondral lesions in this study.
Abbreviations
- FAI:
-
femoroacetabular impingement
- FLASH:
-
fast low-angle shot
- FISP:
-
fast imaging with steady-state precession
- LCEA:
-
lateral centre edge angle
References
Sutter R, Zanetti M, Pfirrmann CWA (2012) New developments in hip imaging. Radiology 264:651–667
Smith TO, Hilton G, Toms AP, Donell ST, Hing CB (2011) The diagnostic accuracy of acetabular labral tears using magnetic resonance imaging and magnetic resonance arthrography: a meta-analysis. Eur Radiol 21:863–874
Blankenbaker DG, de Smet AA, Keene JS, Fine JP (2007) Classification and localization of acetabular labral tears. Skelet Radiol 36:391–397
Sutter R, Zubler V, Hoffmann A, Mamisch-Saupe N, Dora C, Kalberer F, Zanetti M et al (2014) Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol 202:160–169
Pfirrmann CWA, Duc SR, Zanetti M, Dora C, Hodler J (2008) MR arthrography of acetabular cartilage delamination in femoroacetabular cam impingement. Radiology 249:236–241
Llopis E, Cerezal L, Kassarjian A, Higueras V, Fernandez E (2008) Direct MR arthrography of the hip with leg traction: feasibility for assessing articular cartilage. AJR Am J Roentgenol 190:1124–1128
blinded
Tonnis D, Heinecke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 81:1747–1770
Safran MR, Hariri S (2010) Hip arthroscopy assessment tools and outcomes. Oper Tech Orthop 20:264–277
Griffin D, Karthikeyan S (2012) Normal and pathological arthroscopic view in hip arthroscopy. In: Marín-Peña Ó (ed) Femoroacetabular Impingement. Springer, Berlin Heidelberg, pp 113–122
Fleiss JL, Levin B, Paik MC (2003) The measurement of interrater agreement. In: Balding DJ (ed) Statistical methods for rates and proportions. John Wiley & Sons, Hoboken New Jersey, pp 599–608
Agresti A (2002) Categorical data analysis, 2nd edn. John Wiley & Sons, Hoboken, New Jersey
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Wettstein M, Guntern D, Theumann N (2008) Direct MR arthrography of the hip with leg traction: feasibility for assessing articular cartilage. AJR Am J Roentgenol 191:W206–W207, author reply
Ng VY, Arora N, Best TM, Pan X, Ellis TJ (2010) Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med 38:2337–2345
Saupe N, Zanetti M, Pfirrmann CWA, Wels T, Schwenke C, Hodler J (2009) Pain and other side effects after MR arthrography: prospective evaluation in 1085 patients. Radiology 250:830–838
Blankenbaker DG, Ullrick SR, Kijowski R, Davis KW, De Smet AA, Shinki K et al (2011) MR arthrography of the hip: comparison of IDEAL-SPGR volume sequence to standard mr sequences in the detection and grading of cartilage lesions. Radiology 261:863–871
Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B (2008) The function of the hip capsular ligaments: a quantitative report. Arthrosc: J Arthrosc Relat Surg 24:188–195
Harris JD, McCormick FM, Abrams GD, Gupta AK, Ellis TJ, Bach BR et al (2013) Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy 29:589–595
Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP (2006) Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol 186:449–453
Czerny C, Hofmann S, Urban M, Tschauner C, Neuhold A, Pretterklieber M et al (1999) MR arthrography of the adult acetabular capsular-labral complex: correlation with surgery and anatomy. AJR Am J Roentgenol 173:345–349
Mintz DN, Hooper T, Connell D, Buly R, Padgett DE, Potter HG (2005) Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy 21:385–393
Ziegert AJ, Blankenbaker DG, de Smet AA, Keene JS, Shinki K, Fine JP (2009) Comparison of standard hip MR arthrographic imaging planes and sequences for detection of arthroscopically proven labral tear. AJR Am J Roentgenol 192:1397–1400
Schmid MR, Nötzli HP, Zanetti M, Wyss TF, Hodler J (2003) Cartilage lesions in the hip: diagnostic effectiveness of MR arthrography. Radiology 226:382–386
Neumann G, Mendicuti AD, Zou KH, Minas T, Coblyn J, Winalski CS et al (2007) Prevalence of labral tears and cartilage loss in patients with mechanical symptoms of the hip: evaluation using MR arthrography. Osteoarthr Cartil 15:909–917
Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR (2009) Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am 91:305–313
Ellermann J, Ziegler C, Nissi MJ, Goebel R, Hughes J, Benson M et al (2014) Acetabular cartilage assessment in patients with femoroacetabular impingement by using T2* mapping with arthroscopic verification. Radiology 271:512–523
Frank LR, Brossmann J, Buxton RB, Resnick D (1997) MR imaging truncation artifacts can create a false laminar appearance in cartilage. AJR Am J Roentgenol 168:547–554
Acknowledgments
The scientific guarantor of this publication is Ehrenfried Schmaranzer. The authors of this manuscript declare relationships with the following companies: Menges Medical GmBH.The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmaranzer, F., Klauser, A., Kogler, M. et al. Diagnostic performance of direct traction MR arthrography of the hip: detection of chondral and labral lesions with arthroscopic comparison. Eur Radiol 25, 1721–1730 (2015). https://doi.org/10.1007/s00330-014-3534-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3534-x