Abstract
Introduction
Suspicious lesions on breast MRI are often initially evaluated using targeted ultrasound. However, workup varies. Data on the rate of correlate detection by morphology [mass, non-mass enhancement (NME), or focus] would be useful for developing practice guidelines.
Materials and methods
Breast MRI examinations from 1 January 2008 to 31 December 2010 were reviewed. BI-RADS 4 or 5 lesions on MRI evaluated with targeted ultrasound where definitive diagnosis was obtained were included. Statistical analysis was performed on aggregate data and at the lesion level.
Results
A total of 204 lesions were included in the study. A statistically significant difference in ultrasound correlate identification by morphology was found; a correlate was found in 49.3 % of masses, 15 % of NME, and 42.3 % of foci (p = 0.0006). Additional analysis within each morphology demonstrated significantly greater rate of malignancy in masses with an ultrasound correlate than masses without a correlate (p = 0.0062), while the rate of malignancy in NME and foci did not differ with ultrasound correlation.
Conclusions
Morphology of a suspicious lesion on breast MRI affects the probability of identifying an ultrasound correlate. As sonographic correlates are found in nearly half of masses and foci, targeted ultrasound should be the initial step in their workup.
Key Points
• Lesion morphology on breast MRI affects the probability of ultrasound correlate identification.
• An ultrasound correlate is significantly more likely for masses and foci.
• Mass or focus should undergo targeted ultrasound before MRI-guided biopsy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Suspicious lesions identified on magnetic resonance imaging (MRI) of the breast are often pursued using targeted (“second-look”) ultrasound. The aim of targeted ultrasound in this setting is to identify an ultrasound correlate for the MRI finding. This correlate could then serve as a target for ultrasound-guided biopsy, and thereby avoid the need for MRI-guided biopsy. However, not all suspicious lesions identified on breast MRI are evaluated in this manner. At many institutions, further workup of an MRI-detected lesion is left to the discretion of the interpreting radiologist and may include targeted ultrasound (and potentially ultrasound-guided biopsy) or solely MRI-guided biopsy. A survey of Society of Breast Imaging members in 2008 highlighted the notable practice variations in this arena. When asked if they perform second-look ultrasound after identifying a lesion on MRI, 54 % of respondents said “always”, 33 % said “frequently”, 10 % said “sometimes” and 3 % said “rarely” or “never” [1]. To date, there remain no widely accepted guidelines designating which lesions identified on breast MRI are appropriate for targeted ultrasound, and which should go directly to MRI-guided biopsy.
As per the Breast Imaging Reporting and Data System (BI-RADS) lexicon, a lesion identified on breast MRI is characterized morphologically as a mass, non-mass enhancement (NME), or a focus [2]. Data on the rate of ultrasound correlate detection for each of these morphologies, and on the rate of malignancy for each morphology with or without an ultrasound correlate, would be particularly useful in developing detailed, clinically relevant practice guidelines. However, data from existing studies varies substantially [3–11].
The primary goal of this study is to determine the likelihood of ultrasound correlate detection for each lesion morphology (mass, NME, and focus) on breast MRI. Secondary goals are to identify the risk of malignancy associated with each lesion morphology when an ultrasound correlate is identified and the risk of malignancy associated with each lesion morphology when an ultrasound correlate is not identified.
Materials and methods
Patient selection
The institution’s Committee for Human Research approved this retrospective review of patient imaging and charts. An automated search identified breast MRI examinations performed between 1 January 2008 and 31 December 2010 that contained the following key terms: “suspicious” or “BI-RADS 4” or “BI-RADS 5” or “biopsy” or “second look” or “ultrasound” or “sonographic” or “correlate” or “targeted” or “suggestive”. The search algorithm was designed to strip all punctuation and formatting such that all possible permutations of terms would be included.
Inclusion criteria for the study required a targeted ultrasound to have been performed following diagnostic MRI. If not pathognomonically benign on ultrasound, the lesion in question must have undergone image-guided percutaneous sampling (to ensure the pathologic finding was a true correlate to that on imaging). Lesions were excluded from the study if MRI biopsy was performed without preceding targeted US. Additionally, lesions were excluded if pathology results came from lumpectomy or mastectomy specimens (where the site of tissue sampling could not be confirmed to correlate with the suspicious MRI finding). In patients with known breast cancer, findings described as satellite lesions were excluded. Patients with palpable lesions, lesions seen on mammography or those lost to follow-up were also excluded.
Final lesion diagnosis was based on pathology or, in a small number of cases, pathognomonic features of benignity on targeted ultrasound. Pathologic findings considered malignant included ductal carcinoma in situ (DCIS), invasive ductal or lobular carcinoma and sarcoma. All other pathologies were considered benign.
Imaging and interpretation
Bilateral axial breast MRI studies were performed on a 1.5-Tesla scanner (Signa; GE Medical Systems, Milwaukee, WI) using a 7-channel dedicated breast coil (Sentinelle Medical, Toronto, CAN) with patients in the prone position. Standard sequences included a bilateral axial T2-weighted series and dynamic, fat-suppressed T1-weighted 3D fast gradient-recalled-echo series. 3D fast gradient-recalled-echo imaging sequence was performed to produce high-spatial-resolution, fat-suppressed images with full coverage of both breasts. Bilateral axial studies were imaged with the following parameters: repetition time/echo time, 9/4.4 ms; flip angle, 10; number of excitations (NEX), 1; matrix, 512 × 320; field of view, 29–36 cm; slice thickness, 2 mm. The contrast agent, gadopentetate dimeglumine (Magnevist; Berlex, Wayne, NJ), was administered intravenously at a dose of 0.1 mmol/kg of body weight. Injections were performed with an MRI-compatible remote-controlled power injector (Spectris; Medrad, Indianola, PA) at a rate of 1.2 mL/s. Contrast material injection was followed by a 10-mL saline flush administered at the same flow rate. Acquisition times were approximately 180 s. The central phase-encoding lines of each data set were acquired halfway through the acquisition yielding an effective sample time following contrast injection of approximately 90 s for the early post-contrast series. Subtraction images were created using the T1 unenhanced and dynamic contrast-enhanced series. Additional colour kinetic maps were created on a dedicated breast MR interpretation workstation (Aegis 2.0, Sentinelle Medical, Toronto) as needed by the interpreting radiologist.
Common indications for breast MRI at our institution are evaluation of known malignancy (extent of disease, neoadjuvant treatment response, post-lumpectomy with positive margins, etc.) and high-risk screening. Less frequent indications include problem solving (indeterminate conventional imaging, clinical symptom with no conventional imaging correlate, radiologic–pathologic discordance from percutaneous biopsy, etc.) and in the setting of axillary metastases suggesting a breast primary with negative mammogram. All MRI examinations were interpreted by subspecialized breast radiologists with experience ranging from 2 to 37 years. Further evaluation was recommended for all lesions characterized as BI-RADS 4 or 5. However, it was at the discretion of the interpreting radiologist whether this further evaluation should entail targeted ultrasound (and potentially ultrasound-guided biopsy) or only MRI-guided biopsy.
Toshiba SSA-770A ultrasound machines (Toshiba America Medical Systems, Tustin, CA) were used with a 14.0-MHz linear transducer. Targeted breast ultrasound was performed and interpreted exclusively by subspecialized breast radiologists. Only studies directed towards a suspicious finding on recent MRI were considered ‘targeted’. MR images were reviewed by the radiologist prior to the targeted ultrasound. The clock position, distance from nipple and approximate depth were used for lesion targeting. A more extensive surrounding area was scanned to compensate for positional differences between prone MRI and supine ultrasound.
In cases where an ultrasound correlate was identified and the correlate was not definitively benign (intramammary lymph node), an ultrasound-guided sampling was performed. Although there was occasional variation, ultrasound-guided biopsies were usually performed using a 14-G spring-loaded device with five samples obtained. Rarely, a 25-G fine-needle aspiration was performed instead of, or in conjunction with, larger core biopsy. In such cases, a cytopathologist was present and immediately reviewed the aspiration sample for adequacy. A localizing marker was placed at the site of sampling. At our institution, benign ultrasound-guided biopsies generally returned to annual screening.
When an ultrasound correlate could not be identified, patients underwent MRI-guided biopsy. These were performed on our 1.5-T magnet (as detailed above) with patient positioned prone in a dedicated breast biopsy coil (Sentinelle Medical, Inc, Toronto) using a 9-G vacuum-assisted biopsy system (Suros, Hologic, Bedford Massachusetts). Twelve samples were typically obtained. An MRI-compatible localizing marker was placed at the site of biopsy. At our institution, it is recommended that all benign MRI-guided biopsies undergo 6-month follow-up MRI.
Statistical analysis
For all lesions (aggregate data), the rate of ultrasound correlate identification, rate of malignancy, rate malignancy in lesions with an ultrasound correlate and rate of malignancy in lesions without an ultrasound correlate were analysed.
Analysis was then subdivided by morphology. Within each morphologic subgroup (mass, NME, focus), the rate of ultrasound correlation was analysed. Additionally, within each morphologic subgroup, the overall rate of malignancy, the rate of malignancy in lesions with an ultrasound correlate, and the rate of malignancy in lesions without an ultrasound correlate were studied.
Statistical testing of an association between ultrasound correlate detection and morphologic subgroup was performed using Fisher’s exact test for 2 × 2 tables and Chi-square tests for larger tables with a nominal p <0.05 considered statistically significant. Estimated proportions and 95 % confidence intervals (CI) were calculated using two methods to ascertain sensitivity to treating lesions as independent: (1) binomial modelling and (2) generalized estimating equations (with no predictors, a binomial outcome, and logistic link function) to account for clustered observations (i.e. potential correlation of lesion pathology within a single patient). Estimates and Wald CIs of differences in proportions were generated from z-test approximations. Analysis was performed in SAS v. 9.2 by the biostatistical consulting service at the Clinical and Translational Science Institute (CTSI), UCSF.
Results
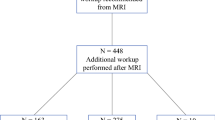
A total of 2,580 contrast-enhanced MR examinations were performed at our institution from 2008 to 2010. In this time period, 505 MR examinations (19.6 %) contained a BI-RADS 4 or 5 lesion. Of these, 204 lesions in 168 patients met inclusion criteria for this study. Indications for the included studies were evaluation of known malignancy (51.8 %), high-risk screening (34.5 %), problem solving (11.9 %) and axillary metastases suggesting breast primary (1.8 %). The average patient age at the time of exam was 48.7 years (26–80 years). Analysis using generalized estimating equations showed no difference from nonparametric modelling. Results are presented using the binomial model.
Ultrasound correlation aggregate data
Eighty-five of the 204 patients had an ultrasound correlate (41.7 %). Of these 85, 33 (38.8 %) were proven to be malignant on ultrasound-guided sampling. Of the remaining 119 patients without an ultrasound correlate (58.3 %), MRI-guided biopsy demonstrated 20 (16.8 %) of these lesions to be malignant. The probability of malignancy in patients with an ultrasound correlate was higher than those without an ultrasound correlate (Fisher’s exact test p = 0.0006; estimated difference 0.22, 95 % z-test confidence interval (CI) 0.10–0.34). Overall, 53 of the 204 lesions (26.0 %) were found to be malignant (39 invasive, 14 in situ).
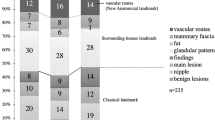
Ultrasound correlation by MRI lesion morphology
The probability of identifying an ultrasound correlate for a lesion seen on breast MRI differed according to the lesion’s morphology; 49.3 % of masses, 15 % of NME, and 42.3 % of foci had ultrasound correlates (p = 0.0006 Chi-square test for null hypothesis of no difference with respect to morphology). Direct comparisons demonstrated the probability of finding an ultrasound correlate for a mass was significantly higher than the probability of finding an ultrasound correlate for NME (p < 0.0001; 0.34, CI 0.19–0.50). The probability of finding an ultrasound correlate for focus was significantly higher than the probability of finding an ultrasound correlate for NME (p = 0.021; 0.27, CI 0.02–0.52). The probability of identifying an ultrasound correlate for a mass was not significantly different from the probability of finding an ultrasound correlate for a focus (p = 0.53; 0.07, CI −0.16 to 0.30).
Masses (Table 1)
One hundred and thirty-eight of the 204 lesions (67.6 %) were masses. Sixty-eight of the 138 masses (49.3 %) had a correlate identified on targeted ultrasound. Ultrasound-guided biopsy demonstrated 30 of these 68 masses (44.1 %) to be malignant, and the remaining 38 (55.9 %) benign. Of the 70 (50.7 %) masses lacking an ultrasound correlate, MRI-guided biopsy demonstrated 15 (21.4 %) to be malignant, and the remaining 55 (78.6 %) benign. In total, as proven by either ultrasound- or MRI-guided biopsy, 45 of the 138 masses (32.6 %) represented malignancy. For masses seen on breast MRI, the likelihood of cancer was statistically significantly greater if an ultrasound correlate was found (p = 0.0062; 0.23, CI 0.07–0.38).
NME (Table 1)
Forty of the 204 suspicious lesions (19.6 %) were NME. Six of these (15.0 %) had an ultrasound correlate identified on targeted ultrasound. Ultrasound-guided biopsy demonstrated 1 of the 6 NME (16.7 %) to be malignant, and the remaining 5 (83.3 %) benign. Of the 34 (85.0 %) cases of NME lacking an ultrasound correlate, MRI-guided biopsy demonstrated 3 (8.8 %) to be malignant, and the remaining 31 (91.2 %) benign. In total, as determined via either ultrasound- or MRI-guided biopsy, 4 cases (10.0 %) of NME were malignant. For NME seen on breast MRI, the estimated difference in the proportion of cancer cases was 0.08 (CI −0.39 to 0.23) if an ultrasound correlate was found; this difference was not statistically significant (p = 0.49). In other words, for NME, the likelihood of cancer was not greater if an ultrasound correlate was found.
Foci (Table 1)
Twenty-six of the 204 suspicious lesions (12.7 %) were foci. Eleven of the 26 (42.3 %) had an ultrasound correlate identified on targeted ultrasound. Ultrasound-guided biopsy demonstrated 2 of the 11 (18.2 %) to be malignant, and the remaining 9 (81.8 %) benign. Of the remaining 15 (57.7 %) foci lacking an ultrasound correlate, MRI-guided biopsy demonstrated 2 (13.3 %) to be malignant, and the remaining 13 (86.7 %) benign. In total, as proven by either ultrasound- or MRI-guided biopsy, 4 (15.4 %) foci were malignant. For foci seen on breast MRI, the estimated difference in the proportion of cancer cases was −0.05 (CI −0.33 to 0.24) if an ultrasound correlate was found; this difference was not statistically significant (p = 1.0). In other words, for foci, the likelihood of cancer was not greater if an ultrasound correlate was found.
Discussion
Our study demonstrates that the morphology of a suspicious lesion on breast MRI affects the probability of identifying an ultrasound correlate for that lesion. When assessing our aggregate data (i.e. lesions not divided by morphology), nearly one half (42 %) of suspicious lesions on MRI had an ultrasound correlate. While within the range of earlier publications (23–89 %) [3, 6–11], this data is of limited value in guiding clinical decision making. Our decision to subdivide lesions based on morphology mirrors clinical practice. In clinical practice, the primary feature used to characterize an abnormality identified on MRI is its morphology. Thus, morphology-based data can help radiologists decide when to recommend targeted ultrasound, thereby having a direct and important clinical impact.
Our morphology-based data demonstrates that an ultrasound correlate was significantly more likely to be identified when an MRI finding was a mass (49 % correlation rate) or a focus (42 %) than when NME (15 %). Similar to our results, recent work by Candelaria et al. [11] and Abe et al. [10] demonstrated a greater likelihood of ultrasound correlate detection for masses and foci than for NME. Meissnitzer et al. [9] did not specifically address ultrasound correlation for foci. However, when the ‘mass’ lesions in Meissnitzer’s study were subdivided by size, lesions <5 mm (potentially classifiable as foci) had a 50 % ultrasound correlation rate; this was very similar to our results (42 %) and those of Abe et al. (46 %). Demartini et al. found a significantly higher ultrasound correlate identification rate for masses (58 %) versus NME (30 %), but not for foci (37 %) [7]. Given the considerable ultrasound correlation rate for lesions demonstrating mass or focus morphology on MRI, targeted ultrasound is an appropriate first step in most cases.
The morphology least likely to have an ultrasound correlate is NME. This information can have varying clinical applications. It could be argued that even NME should undergo targeted ultrasound. Ultrasound is inexpensive, well tolerated by patients, and radiation-free. Even at the lowest end of the spectrum, a 12 % (as seen by Abe et al.) to 15 % (as seen in the current study) chance of identifying an ultrasound correlate and facilitating ultrasound-guided biopsy may be valuable. On the other hand, the 12–15 % correlation rate for NME could also be used to justify the alternate approach. Some might suggest that the 85–88 % chance of not identifying an ultrasound correlate is sufficient evidence to forgo ultrasound and take patients with NME directly to MRI-guided biopsy for efficiency. Given the widely variable data, uniform guidelines for this particular lesion morphology will likely be difficult to develop, and an individual institution’s experience, restrictions, and preferences will have to be considered.
Foci deemed suspicious on MRI had a considerable overall malignancy rate of 16 %. Data reported by Gutierrez et al. [12] is strikingly similar to our results, showing a 15 % rate of malignancy for suspicious foci identified on MRI. Subdividing our data set into those with and without ultrasound correlate demonstrated 19 % of foci with an ultrasound correlate to be malignant and 13 % of foci without an ultrasound correlate to be malignant (Table 1). These figures illustrate the need to sample foci with or without an ultrasound correlate, and counter prior suggestions that foci of enhancement can essentially be ignored [13]. Advances in spatial resolution available in current MRI technology have allowed even foci to often be appropriately regarded as suspicious. If suspicious, foci should be pursued as with any other (larger) mass.
Our aggregate data demonstrated the risk of malignancy to be greater when a lesion seen on MRI had an ultrasound correlate (38.8 %) than when a lesion did not have an ultrasound correlate (16.8 %, p = 0.0006). However, the risk of malignancy in lesions without ultrasound correlates was sufficiently high (9–21 %) to warrant MRI-guided sampling. Had any particular lesion morphology shown an extremely low malignancy rate in the setting of no ultrasound correlate, perhaps the MRI-biopsy could have been averted. Our data does not support this approach for any individual lesion morphology. In keeping with previous data on malignancy rates in the presence or absence of an ultrasound correlate [3, 7–10], lesions without ultrasound correlates nonetheless require tissue sampling with MRI-guided biopsy.
This study has a number of limitations. It is a retrospective review from a single institution. Our institution does not have a protocol regarding the recommendation for targeted ultrasound after diagnostic MRI. The decision to recommend targeted ultrasound is left to the discretion of the individual radiologist. As a result, in some cases where the interpreting radiologist believes an MRI lesion is unlikely to have an ultrasound correlate, a recommendation to proceed directly to MRI-guided biopsy may be made. Such cases would have been excluded from our study, potentially introducing bias. However, this limitation was part of the impetus for undertaking the study. Our correlate detection was maximized because in the study cases, the radiologist interpreting the MRI believed the lesion was sufficiently likely to have a correlate to be recommended for targeted ultrasound. Had targeted ultrasound been performed uniformly on all MRI lesions recommended for biopsy, correlation rates would likely have been lower. Data obtained has allowed us to develop a morphology-based guideline for the appropriateness of targeted ultrasound after an abnormality is identified on MRI.
Bias may also have been introduced into our data set because of our institutional policy of subspecialty breast radiologists reading all breast MRIs and performing all breast ultrasound examinations. Technologists do not perform breast ultrasound at our institution. The proportion of lesions deemed suspicious on MRI and the identification of ultrasound correlates may differ from those in a non-specialized setting. At our institution, ultrasound-guided sampling is only recommended if the subspecialized breast radiologist is confident the lesion identified sonographically is the MRI correlate. Therefore, immediate post-biopsy MRI to confirm MRI-ultrasound correlation is rarely performed. Six-month follow-up MRI is recommended for all benign concordant biopsies.
Finally, our analysis of ultrasound correlation is limited to lesion characterization by morphology. Within each morphologic category, it is possible that further lesion differentiation based on additional features (e.g. size, margins, internal enhancement and enhancement kinetics) would impact ultrasound correlation rates.
In conclusion, our study illustrates that the morphology of a lesion on breast MRI affects the probability of finding an ultrasound correlate, with the probability of finding a mass or focus correlate to be similar to one another, and statistically greater than the probability of finding a correlate for NME. As sonographic correlates are found in nearly half of masses and foci, targeted ultrasound should be the initial step in the workup of most such cases. Even in cases where no ultrasound correlate is identified, the rate of malignancy for all lesion morphologies is considerable. Tissue sampling should be pursued even in the absence of an ultrasound correlate.
References
Bassett LW, Dhaliwal SG, Eradat J et al (2008) National trends and practices in breast MRI. AJR Am J Roentgenol 191:332–339
D'Orsi CJ, Sickles EA, Mendelson EB, Morris EA et al (2013) Breast imaging reporting and data system: ACR BI-RADS - breast imaging atlas, 5th edn. American College of Radiology, Reston
LaTrenta LR, Menell JH, Morris EA, Abramson AF, Dershaw DD, Liberman L (2003) Breast lesions detected with MR imaging: utility and histopathologic importance of identification with US. Radiology 227:856–861
Beran L, Liang W, Nims T, Paquelet J, Sickle-Santanello B (2005) Correlation of targeted ultrasound with magnetic resonance imaging abnormalities of the breast. Am J Surg 190:592–594
Sim LS, Hendriks JH, Bult P, Fook-Chong SM (2005) US correlation for MRI-detected breast lesions in women with familial risk of breast cancer. Clin Radiol 60:801–806
Wiratkapun C, Duke D, Nordmann AS et al (2008) Indeterminate or suspicious breast lesions detected initially with MR imaging: value of MRI-directed breast ultrasound. Acad Radiol 15:618–625
Demartini WB, Eby PR, Peacock S, Lehman CD (2009) Utility of targeted sonography for breast lesions that were suspicious on MRI. AJR Am J Roentgenol 192:1128–1134
Destounis S, Arieno A, Somerville PA et al (2009) Community-based practice experience of unsuspected breast magnetic resonance imaging abnormalities evaluated with second-look sonography. J Ultrasound Med 28:1337–1346
Meissnitzer M, Dershaw DD, Lee CH, Morris EA (2009) Targeted ultrasound of the breast in women with abnormal MRI findings for whom biopsy has been recommended. AJR Am J Roentgenol 193:1025–1029
Abe H, Schmidt RA, Shah RN et al (2010) MR-directed (“Second-Look”) ultrasound examination for breast lesions detected initially on MRI: MR and sonographic findings. AJR Am J Roentgenol 194:370–377
Candelaria R, Fornage BD (2011) Second-look US examination of MR-detected breast lesions. J Clin Ultrasound 39:115–121
Gutierrez RL, DeMartini WB, Eby PR, Kurland BF, Peacock S, Lehman CD (2009) BI-RADS lesion characteristics predict likelihood of malignancy in breast MRI for masses but not for nonmasslike enhancement. AJR Am J Roentgenol. 193(4):994–1000
Liberman L, Mason G, Morris EA, Dershaw DD (2006) Does size matter? Positive predictive value of MRI-detected breast lesions as a function of lesion size. AJR Am J Roentgenol 186:426–430
Acknowledgements
The scientific guarantor of this publication is Bonnie Joe MD, PhD. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. University of California San Francisco Clinical and Translational Science Institute provided statistical advice for this manuscript. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Some study subjects or cohorts have been previously reported in presentation format at ARRS 2012. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hollowell, L., Price, E., Arasu, V. et al. Lesion morphology on breast MRI affects targeted ultrasound correlation rate. Eur Radiol 25, 1279–1284 (2015). https://doi.org/10.1007/s00330-014-3517-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3517-y