Abstract
Purpose
The purpose of this study was to assess the diagnostic performance of contrast-enhanced sonography (CEUS) for the differentiation of focal nodular hyperplasia (FNH) from hepatocellular adenoma (HCA) according to lesion size.
Materials and methods
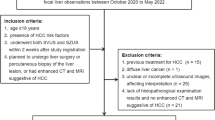
Forty patients with a definite diagnosis of FNH or HCA who underwent CEUS were included in this institutional review board (IRB)-approved study. A total of 43 FNHs and 20 HCAs, including 15 inflammatory HCAs and five unclassified HCAs, were analysed. Two radiologists reviewed the diagnostic CEUS parameters separately and in consensus, including the presence or absence of centrifugal filling and central vessels. The sensitivity (Se), specificity (Sp), and inter-observer confidence (Kappa) of CEUS diagnostic parameters were assessed.
Results
Inter-observer agreement of CEUS for FNH diagnosis was high (kappa = 0.81) with an overall Se of 67.4 % [29/43 (CI 95 %: 51.4–80.1 %)] and an Sp of 100 % [20/20 (CI 95 %: 81–100 %)]. Significantly higher Se figures were found for lesions ≤ 35 mm than for lesions > 35 mm [respectively, 93 % (28/30) (CI 95 %: 77.6–99.2) vs. 7.7 % (1/13) (CI 95 %: 0.2–36 %), p = 0.002] with unchanged specificity.
Conclusion
CEUS is highly specific for the diagnosis of FNH, with very good inter-observer agreement, whatever the size, but its sensitivity is significantly reduced in diagnosing lesions larger than 35 mm.
Key Points
• CEUS is highly specific for the diagnosis of FNH, regardless of lesion size
• CEUS shows reduced sensitivity in diagnosing FNH lesions larger than 35 mm
• The filling patterns of hepatocellular adenomas are not affected by lesion size
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The differentiation of focal nodular hyperplasia (FNH) from hepatocellular adenomas (HCA) is an important challenge because the management of these two benign hepatocellular tumours differs drastically: FNHs are treated conservatively, while HCAs may need to be surgically removed because of their potential risk of malignant transformation and bleeding [1–5].
Two distinct, typical vascular profiles have been described with contrast-enhanced sonography (CEUS) for the differential diagnosis of FNH and HCA, including distinct arterial filling direction and vessel distribution. FNH is predicted on the basis of stellate vascularity, centrifugal filling, and sustained enhancement on the portal phase, whereas HCA is associated with a mixed or centripetal filling without stellate vascularity, and washout on the portal venous phase [6–11].
However, and despite these two distinct patterns, the accurate distinction of FNH from HCA on CEUS suffers from several limitations: Inflammatory HCA, the most frequent subtype of the HCA tumour, is known to mimic FNH on CEUS [12–14]. In addition, different CEUS features of FNH have been reported in relation to their size [11, 15, 16]. Wang et al. [11] recently examined computed tomography (CT) and CEUS for the diagnosis of FNH, and suggested that centrifugal filling was more common in small FNHs than in larger lesions. To the contrary, Bartolotta et al. reported in a study on 92 FNH lesions that the typical presentation on CEUS, including spoke-wheel morphology, was more frequent in large lesions [15]. Interestingly, in both of these studies, only FNHs were included, and the CEUS presentations of FNH and HCA were not compared.
The purpose of our study was therefore to assess the diagnostic performance of CEUS for the differentiation of FNH from HCA according to lesion size.
Materials and methods
Patient population
Our institutional review board approved this monocentric, retrospective study, and the requirement for informed consent was waived.
Patient population
Between January 2009 and March 2013, we reviewed the files of all patients with a definite diagnosis of either FNH or HCA. Patients with cystic lesions, malignant lesions and hemangiomas, and chronic liver disease were not included. A total of 40 patients—31 patients with only FNHs, seven patients with only HCAs, and two patients with both FNHs and HCAs—were included, with a total of 63 lesions (43 FNHs and 20 HCAs). The mean age was 41.6 years (range 20–76 years). There were 32 female patients and eight male patients. The mean size of all lesions was 33 mm (range 10–183 mm). There were no significant differences between the group of patients with FNHs and HCAs in terms of age (42.9 years +/- 14.1 vs 36.4 years +/- 10.1, respectively; p = 0.25) or the mean size of lesions (31.1 +/- 20.4 mm vs 37.1 +/- 35.9 mm, respectively, p = 0.73). The size distribution of all included lesions was as follows: 22 lesions ≤ 19 mm (15 FNHs and seven HCAs); 22 lesions ≥ 20 mm and ≤ 39 mm (15 FNHs and seven HCAs); 19 lesions ≥ 40 mm (13 FNHs and six HCAs). The main radiological and pathologic data of the study population are summarised in Table 1.
Diagnosis confirmation
-
HCA: Overall, 20/20 HCAs (100 %) were diagnosed based on pathology, including immunohistochemistry data. There were 15 inflammatory HCAs and five HCAs of the unclassified form [17].
-
FNH: In total, 8/43 FNHs (18.6 %) were diagnosed based on pathology. Pathologic confirmation was recommended by a multidisciplinary staff decision because of the absence of any visible central scar for seven FNH lesions, and the presence of intra-lesional fat and concomitant absence of a central scar for one FNH lesion. The size of the eight FNHs that were confirmed on pathology ranged from 12 mm to 57 mm (mean 32.7 mm +/- 17 mm). The diagnosis of the remaining 35 FNH lesions was confirmed on typical gadobenate dimeglumine (Gd-BOPTA) magnetic resonance imaging (MRI) presentation and a follow-up for at least six months demonstrating no change on imaging examinations (mean follow-up: 10.5 months +/- 6.8). FNHs were characterised based on both typical presentation on T1-WI, T2-WI, dynamic Gd-enhanced MRI, and hepatobiliary phase MRI [18].
Sonography technique
All CEUS examinations were performed on Aplio (Toshiba Medical Systems), by two radiologists with seven and 10 years of experience in liver CEUS. CEUS was performed with Sonovue® (Bracco, Milan, Italy), injected via the peripheral venous route. The image frame rate was 11 Hz.
First, baseline gray-scale sonography and color Doppler were performed to identify each hepatic lesion. Then, low-mechanical-index (<0.1) contrast-enhanced ultrasound was performed after the bolus injection of 2.4 mL Sonovue® (Bracco, Milan, Italy) followed by a 20-ml saline flush. Multiple cineloops and still frames were recorded to show gray-scale sonography and enhancement kinetics after the injection of microbubbles until five minutes had passed. The arterial phase was defined as the 0–35-s interval after the flush was completed, the portal phase was 35–120 s, and the late phase began after 120 s. All imaging data were archived on the institution PACS system for further analyses.
Sonography analysis
Two radiologists with 10 (reader 1) and five (reader 2) years of experience in liver imaging, blinded to clinical, other imaging, and pathology findings, independently assessed the following CEUS parameters on the archived cine-loops: arterial phase enhancement (hypervascular, isovascular, or hypovascular), portal venous phase enhancement (iso-, hyper-, or hypoechoic relative to the adjacent normal liver parenchyma), filling direction (centrifugal, centripetal, or mixed), presence of a central artery, transient peripheral unenhanced zone, central scar, and central necrosis.
The following previously published criteria were used for CEUS analysis [7]: centrifugal filling was defined as initial central enhancement that progressed toward the periphery of the lesion over time. The initial presence of microbubbles elsewhere than in the centre of the lesion was not considered centrifugal (i.e., mixed or centripetal). Centripetal filling was defined as initial peripheral enhancement that progressed toward the centre of the lesion over time. The arterial phase filling pattern was considered mixed if the enhancement occurred throughout the lesion and did not show either a centrifugal or a centripetal filling direction. A transient peripheral unenhanced zone was defined as a non-enhancing rim-like area in the periphery of the lesion in the arterial phase that gradually disappeared over time. Central arteries were defined by the presence of enhancing central arteries with either linear or star-like or spoke-wheel morphology. A central scar was defined as a central stellate hypoechoic linear without contrast enhancement in the portal venous phase. Central necrosis was defined as an irregular area without contrast enhancement on all phases.
According to these established literature criteria, each reader was asked to grade each lesion as follows: score 1, definitely FNH; score 2, probably an FNH; score 3, possibly an FNH; score 4, probably an HCA; score 5, definitely an HCA [6–11, 19, 20]. An FNH with a score of 1 showed both centrifugal filling and at least two other criteria among the following, while an FNH with a score of 2 showed both centrifugal filling and one other criteria among the following: central artery, central scar, transient peripheral unenhanced zone, and absence of hypoechoicity in the portal venous phase. Lesions with mixed or centripetal filling were graded with scores of 3, 4, or 5.
A consensus analysis of each lesion was performed by the two readers in a distinct reading session performed 12 weeks after the first one, all cases being reviewed in a random order. In the case of a disagreement between the two readers, a third reader with 15 years of experience in liver imaging decided the final score.
Statistical analysis
Patient and lesion characteristics are presented as the number and percentage for qualitative variables, and as the mean with standard deviation for quantitative variables. Comparisons between groups were performed with Fisher’s exact test and the Mann–Whitney U test, and McNemar’s test was used to compare sensitivities. Sensitivity, specificity, positive predictive value, and accuracy in differentiating FNH from HCA were calculated for each diagnostic sign—arterial filling, central artery and scar, transient unenhanced zones, central necrosis, enhancement in the portal venous phase—and for the overall classification.
A diagnosis of FNH was considered positive for lesions graded with a score of 1 or 2.
Consensus analysis of diagnostic performance according to lesion size was performed using a receiver operating characteristic (ROC) curve, and the size cut-off value providing the highest Youden index was noted. The comparison of CEUS features and CEUS diagnostic performance between the two groups using this cut-off value was carried out based on consensus analysis.
Weighted Kappa statistics were calculated to assess inter-observer agreement. Agreement was graded as k < 0.20, poor; 0.20–0.39, fair; 0.40–0.59, moderate; 0.60–0.79, substantial; or 0.80–1.00, almost perfect [21].
For all analyses, a two-sided p-value of ≤ 0.05 was considered statistically significant. Statistical analysis was performed with Graphpad Prism software, version 5.0 (LA Jolla, CA).
Results
CEUS presentation of all lesions
The CEUS features based on consensus and individual analysis are summarised in Table 2. All 63 lesions were hypervascular on the arterial phase.
Centrifugal filling was significantly more commonly observed in FNHs than in HCAs (p < 0.001 for both readers) (Fig. 1). On the other hand, centripetal filling was significantly more frequent in HCAs (p < 0.001 for reader 1 and p < 0.0001 for reader 2). There was no significant difference regarding the mixed filling between FNHs and HCAs (p = 0.055 for reader 1 and p = 0.27 for reader 2). The analysis of the filling pattern between readers showed an almost perfect inter-observer agreement (Kappa = 0.81).
The presence of a transient peripheral unenhanced zone was significantly more common in FNHs than in HCAs (p < 0.001 for reader 1 and p < 0.009 for reader 2), with substantial inter-observer agreement (Kappa = 0.71).
Central arteries were more commonly observed in FNHs than in HCAs, and were significantly more frequent for reader 1 (p < 0.001), with a fair inter-observer agreement (Kappa = 0.29) (Fig. 1).
Sustained portal venous phase enhancement was more commonly observed in FNHs and hypoechoicity in the portal venous phase was more commonly observed in HCAs (p = 0.002 for reader 1 and p = 0.03 for reader 2), with almost perfect inter-observer agreement (Kappa = 0.9).
There was no significant difference regarding the presence or absence of a central scar between FNHs and HCAs (p = 0.2 for reader 1 and p = 1 for reader 2).
Central necrosis was never observed in either FNH or HCA.
Overall CEUS diagnostic performance, whatever lesion size
The grading of all lesions based on consensus analysis is summarised on Table 3. Overall, 29/43 FNHs (67.4 %) were graded with a score of 1 and 2, while 15/20 HCAs (75 %) were graded 4 and 5.
For the diagnosis of all FNHs, whatever the size, the sensitivity, specificity and positive predictive value of CEUS were, respectively, 67 % (CI 95 %: 51.4–89.9 %), 100 %, and 100 % for reader 1 and 56 % (CI 95 %: 41.1–69.6 %), 95 % (CI 95 %: 74.6–100 %), and 96 % (CI 95 %: 78.9–100 %) for reader 2.
Overall, the inter-observer agreement for the diagnosis of FNH was almost perfect (kappa = 0.81).
On consensus analysis, the sensitivity and specificity of CEUS for the diagnosis of FNH were 67.4 % (CI 95 %: 51.4–80.1 %) and 100 % (CI 95 %: 81–100 %), respectively.
Consensus analysis of the impact of lesion size on CEUS diagnostic confidence
Based on ROC curve analysis, the highest diagnostic accuracy was provided using a 35-mm lesion size cut-off value (AUC: 0.88 [CI 95 %: 0.79–0.97], p < 0.0001), as shown in Fig. 2.
For the diagnosis of an FNH ≤ 35 mm, the sensitivity, specificity, and positive predictive value of CEUS were, respectively, 93 % (CI 95 %: 77.6–99.2 %), 100 %, and 100 % for reader 1 and 77 % (CI 95 %: 58.8–88.5 %), 93 % (CI 95 %: 66.5–100 %), and 96 % (CI 95 %: 78.1–100 %) for reader 2. For the diagnosis of an FNH > 35 mm, the sensitivity, specificity, and positive predictive value of CEUS were, respectively, 8 % (CI 95 %: 0.2–36 %), 100 % and 100 % for both readers.
Based on consensus analysis, the sensitivity for FNH diagnosis was significantly lower in FNH lesions > 35 mm compared to FNHs ≤ 35 mm [7.7 % (CI 95 %: 0.2–36 %) vs 93.3 % (CI 95 %: 77.6–99.2 %), p = 0.002], as shown in Table 4.
The mean size of the 29 FNHs scored as 1 or 2, according to the consensus analysis (Fig. 3), was significantly smaller than that of the 14 FNHs scored as 3, 4, or 5 (20.2 mm +/- 8.2 mm and 53.5 mm +/- 19.5 mm, respectively, p < 0.0001).
Impact of lesion size on CEUS features
-
FNH lesions:
The CEUS features for FNHs ≤ 35 mm and for FNHs > 35 mm are summarised in Table 5 and Fig. 4. Centrifugal filling and transient peripheral unenhanced zones were significantly more commonly observed in FNHs ≤ 35 mm (respective OR = 124.7 [11.3; 6927.3], p < 0.0001; and OR = 25.8 [3; 1242.4], p = 0.0002) (Fig. 4). Central arteries (OR = 1.5 [0.3; 8.2], p = 0.73), or central scar (OR = 0.38 [0.04; 3.3], p = 0.38) were equally detected in FNHs, no matter the lesion size.
Hypoechoic FNHs during the portal venous phase were detected in 3/30 (10 %) of the FNHs ≤ 35 mm and in 1/13 (8 %) of the FNHs > 35 mm. These four hypoechoic FNHs were all associated with liver steatosis and were all hypoechoic on baseline gray-scale sonography. There were no statistically significant differences in terms of sustained enhancement or hypoechoicity in the portal venous phase between FNHs ≤ 35 mm and FNHs > 35 mm (OR = 0.75 [0.001; 10.6], p = 1.0).
-
HCA lesions:
The CEUS features for HCAs ≤ 35 mm and HCAs > 35 mm are summarised in Table 6.
Centrifugal filling, central arteries, or central scar were never observed in any HCAs. The presence of centripetal, mixed filling, or of a transient peripheral unenhanced zone (Figs. 5 and 6) was equally distributed between HCAs ≤ 35 mm or HCAs > 35 mm (p = 1).
Image from a 29-year-old woman with both a large, 45-mm focal nodular hyperplasia and a 10-mm large hepatocellular adenoma, each diagnosed based on pathology. Contrast-enhanced sonograms after injection show a large lesion with mixed filling on the arterial phase (arrow) corresponding to the FNH lesion, and a second small lesion with centripetal filling (arrowhead) corresponding to the hepatic adenoma. The large mass was misdiagnosed as hepatic adenoma on CEUS because of mixed filling
Hypoechoic appearance in the portal venous phase was more common in HCAs > 35 mm than in HCAs ≤ 35 mm (p = 0.05, OR = 12.5 [1.4; 112.2]).
Discussion
Differentiating FNH from HCA remains challenging, as these benign hepatocellular lesions share common clinical and radiological features. Previous publications have suggested that CEUS is efficient for differentiation between FNH and HCA [7–10, 22]. This study first confirms the high specificity of CEUS for the diagnosis of FNH, for any lesion size [11, 12]. In addition, this study suggests that the key diagnostic features of FNH are less frequently recognised in FNH lesions > 35 mm, thereby reducing the diagnostic performance of CEUS.
In lesions smaller than 35 mm, the observed sensitivity and specificity of CEUS for the diagnosis of FNH were 93.3 % and 100 %, respectively. These results confirm that CEUS could be complementary to MRI, which is known to be less accurate for small FNH analysis because of frequently absent central stellate areas [3, 23].
Both the centrifugal filling pattern and the transient peripheral unenhanced zone were significantly less frequently encountered in FNHs larger than 35 mm. These results confirm those of a recent study [11] in which a centrifugal filling was more commonly associated with FNHs < 3 cm. Larger lesions are associated with an increased vascular supply and the presence of several feeding arteries [24]. This probably alters the early imaging presentation of FNH, and hence, the diagnostic performance of CEUS. As a result, we observed that the mean size of typical FNH (score 1 or 2) was significantly smaller than that of FNH lesions with scores of 3, 4 or 5. Interestingly, there was no statistical difference between FNH and HCA in terms of lesion size, suggesting that both large FNH lesions and HCAs showed mixed or centripetal enhancement.
In this study, of the 13 FNH lesions associated with liver steatosis, four were hypoechoic in the portal venous phase (31 %), all of which were already hypoechoic prior to contrast injection. This result is in accordance with the study of Bartolotta et al. [25], in which five out of 16 FNH lesions (31 %) associated with liver steatosis were hypoechoic in the portal venous phase on CEUS.
Regarding HCA feature presentation according to lesion size, the results of this study show that the filling patterns of HCAs were not affected by lesion size. However, large HCAs were more commonly hypoechoic in the portal venous phase than small lesions. In comparison to previous studies dealing with FNH and HCA observed on CEUS, we report lower sensitivity and higher specificity figures for FNH diagnosis. Kim et al. reported sensitivity figures ranging from 86 to 95 % and specificity figures ranging from 74 to 79 % [7]. In the present study, FNHs were considered typical only if they were graded with scores 1 and 2, while scores of 1, 2, and 3 were considered typical in the study of Kim et al. In addition, centrifugal filling was strictly defined as initial central enhancement progressing over time toward the periphery of the lesion. The initial presence of microbubbles anywhere beyond the centre of the lesion was enough to consider the filling as mixed or centripetal. Moreover, FNH lesions were analysed together with a high proportion of inflammatory adenomas, which share with FNH an early and intense enhancement on arterial phase imaging.
Interestingly, the overall inter-observer agreement regarding the CEUS-based diagnosis of FNH (lesion score 1 or 2) was almost perfect (kappa = 0.81). Moreover, no matter the lesion size, the inter-observer agreement on CEUS features in individual analysis was excellent for all criteria except the identification of a central artery, a point which has already been reported in the literature [7], suggesting that this parameter is the least reproducible. In addition, the ambiguous definition of spoke-wheel artery, spoke-wheel sign, and feeding artery could explain the variable detection rate of these signs in the literature [7, 11, 15, 16]. This could also explain why central arteries as defined here were not more frequently observed in larger FNH lesions, conversely to the study of Wang et al [11].
This study bears several limitations. First, only FNH and HCA lesions were included, thereby excluding malignant primary or metastatic lesions. Although HCAs are known mimickers of FNHs, this selection bias probably improved the overall accuracy. Second, the diagnostic performance of CEUS for HCA diagnosis was not performed. Indeed, HCAs are diagnosed based on pathology in order to exclude the possibility of hepatocellular carcinoma. In addition, our aim was rather to fully characterise FNHs and differentiate them from HCAs. Third, ß-catenin-mutated and steatotic HCAs were not present in this study. However, it is well-known that the most troublesome situation is the differential diagnosis between FNH and inflammatory HCA, as this subtype shares common imaging features with FNH, especially regarding early and intense enhancement, unlike the steatotic form, which is hypovascular [14]. Fourth, although all HCA lesions underwent percutaneous biopsy or surgical resection, a large proportion of FNH lesions lacked pathological confirmation; however, in all of these latter cases, the diagnosis was reached with Gd-BOPTA MRI, a hepatobiliary contrast agent with optimal sensitivity and specificity [18, 23, 26]. Moreover, it is now well-accepted that FNH lesions should not be biopsied when they show typical aspects on MRI [3, 18]. Lastly, our aim was not to test the performance of CEUS as compared to Gd-BOPTA MRI, but rather to determine the impact of lesion size on diagnostic confidence with CEUS.
In conclusion, this study shows that CEUS is highly specific for the diagnosis of FNH for any lesion size, with very good inter-observer agreement, but that its sensitivity is significantly reduced in lesions larger than 35 mm. Hence, CEUS could be a useful adjunct tool in assessing smaller lesions, whereas MRI should probably be used for larger lesions.
Abbreviations
- FNH:
-
Focal nodular hyperplasia
- HCA:
-
Hepatocellular adenoma
- CEUS:
-
Contrast-enhanced ultrasound
- Gd-BOPTA:
-
Gadobenate dimeglumine
References
Herman P, Pugliese V, Machado MA et al (2000) Hepatic adenoma and focal nodular hyperplasia: differential diagnosis and treatment. World J Surg 24:372–376
De Carlis L, Pirotta V, Rondinara GF et al (1997) Hepatic adenoma and focal nodular hyperplasia: diagnosis and criteria for treatment. Liver Transpl Surg 3:160–165
Cherqui D, Rahmouni A, Charlotte F et al (1995) Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology 22:1674–1681
Weimann A, Ringe B, Klempnauer J et al (1997) Benign liver tumors: differential diagnosis and indications for surgery. World J Surg 21:983–990, discussion 990-981
Terkivatan T, de Wilt JH, de Man RA et al (2001) Indications and long-term outcome of treatment for benign hepatic tumors: a critical appraisal. Arch Surg 136:1033–1038
Vilgrain V (2006) Focal nodular hyperplasia. Eur J Radiol 58:236–245
Kim TK, Jang HJ, Burns PN, Murphy-Lavallee J, Wilson SR (2008) Focal nodular hyperplasia and hepatic adenoma: differentiation with low-mechanical-index contrast-enhanced sonography. AJR Am J Roentgenol 190:58–66
Zhu XL, Chen P, Guo H et al (2011) Contrast-enhanced ultrasound for the diagnosis of hepatic adenoma. J Int Med Res 39:920–928
Dietrich CF, Schuessler G, Trojan J, Fellbaum C, Ignee A (2005) Differentiation of focal nodular hyperplasia and hepatocellular adenoma by contrast-enhanced ultrasound. Br J Radiol 78:704–707
Leen E, Ceccotti P, Kalogeropoulou C, Angerson WJ, Moug SJ, Horgan PG (2006) Prospective multicenter trial evaluating a novel method of characterizing focal liver lesions using contrast-enhanced sonography. AJR Am J Roentgenol 186:1551–1559
Wang W, Chen LD, Lu MD et al (2013) Contrast-enhanced ultrasound features of histologically proven focal nodular hyperplasia: diagnostic performance compared with contrast-enhanced CT. Eur Radiol 23:2546–2554
Soussan M, Aube C, Bahrami S, Boursier J, Valla DC, Vilgrain V (2010) Incidental focal solid liver lesions: diagnostic performance of contrast-enhanced ultrasound and MR imaging. Eur Radiol 20:1715–1725
Paradis V, Benzekri A, Dargere D et al (2004) Telangiectatic focal nodular hyperplasia: a variant of hepatocellular adenoma. Gastroenterology 126:1323–1329
Laumonier H, Cailliez H, Balabaud C et al (2012) Role of contrast-enhanced sonography in differentiation of subtypes of hepatocellular adenoma: correlation with MRI findings. AJR Am J Roentgenol 199:341–348
Bartolotta TV, Midiri M, Scialpi M, Sciarrino E, Galia M, Lagalla R (2004) Focal nodular hyperplasia in normal and fatty liver: a qualitative and quantitative evaluation with contrast-enhanced ultrasound. Eur Radiol 14:583–591
Ungermann L, Elias P, Zizka J, Ryska P, Klzo L (2007) Focal nodular hyperplasia: spoke-wheel arterial pattern and other signs on dynamic contrast-enhanced ultrasonography. Eur J Radiol 63:290–294
Dokmak S, Paradis V, Vilgrain V et al (2009) A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology 137:1698–1705
Grazioli L, Morana G, Kirchin MA, Schneider G (2005) Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study. Radiology 236:166–177
Trillaud H, Bruel JM, Valette PJ et al (2009) Characterization of focal liver lesions with SonoVue-enhanced sonography: international multicenter-study in comparison to CT and MRI. World J Gastroenterol 15:3748–3756
Quaia E (2011) The real capabilities of contrast-enhanced ultrasound in the characterization of solid focal liver lesions. Eur Radiol 21:457–462
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Quaia E, Calliada F, Bertolotto M et al (2004) Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology 232:420–430
Grazioli L, Morana G, Federle MP et al (2001) Focal nodular hyperplasia: morphologic and functional information from MR imaging with gadobenate dimeglumine. Radiology 221:731–739
Kamel IR, Liapi E, Fishman EK (2006) Focal nodular hyperplasia: lesion evaluation using 16-MDCT and 3D CT angiography. AJR Am J Roentgenol 186:1587–1596
Bartolotta TV, Taibbi A, Galia M et al (2007) Characterization of hypoechoic focal hepatic lesions in patients with fatty liver: diagnostic performance and confidence of contrast-enhanced ultrasound. Eur Radiol 17:650–661
Hussain SM, Terkivatan T, Zondervan PE et al (2004) Focal nodular hyperplasia: findings at state-of-the-art MR imaging, US, CT, and pathologic analysis. Radiographics 24:3–17, discussion 18-19
Acknowledgements
The scientific guarantor of this publication is Dr. Vincent Roche. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roche, V., Pigneur, F., Tselikas, L. et al. Differentiation of focal nodular hyperplasia from hepatocellular adenomas with low-mecanical-index contrast-enhanced sonography (CEUS): effect of size on diagnostic confidence. Eur Radiol 25, 186–195 (2015). https://doi.org/10.1007/s00330-014-3363-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3363-y