Abstract
Objectives
To investigate whether DTI allows assessment of renal impairment and pathology in patients with chronic glomerulonephritis.
Materials and methods
Seventy-five patients and 20 healthy volunteers were enrolled in this study. Renal function and kidney biopsies were evaluated. For DTI, a respiratory-triggered coronal EPI sequence was performed (TR, 1400 ms; TE, 76 ms; diffusion direction, 6; NEX, 4; b values, 0 and 600 s/mm2; slices thickness, 6 mm, with no intersection gap). Renal ADC and FA values were calculated and compared between the groups. Correlations between ADC/FA and histopathology were evaluated.
Results
ADC values decreased with increased stages. ADC differences in renal parenchyma at different disease stages were found, with the exception of the control group compared with stage 1 patients; similar results were obtained for FA. ADC values in the cortex and medulla in stage 1-3 patients were both statistically different, similar to the FA values. A significant negative correlation was found between the percentage of glomerulosclerosis and FA in the renal cortex (r = -0.74), similar to the degree of tubulointerstitial fibrosis with FA in the medulla (r = -0.76).
Conclusions
ADC and FA values are correlated with the degree of renal impairment, the percentage of glomerulosclerosis, and area of interstitial fibrosis.
Key Points
• DTI can be used to assess renal function impairment in patients with chronic glomerulonephritis.
• ADC and FA values were correlated with tubulointerstitial fibrosis and glomerulosclerosis.
• Identification of renal impairment is helpful for timely treatment.
• DTI can be used for non-invasive assessment of renal pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic glomerulonephritis is the most common cause of end-stage renal disease in China [1]. The condition develops over a period of several years, up to 20 years, and is followed by progression to end-stage renal disease. Structural abnormalities in chronic glomerulonephritis include kidney hypertrophy, thickening of the glomerular basement membrane, nodular and diffuse glomerulosclerosis, tubular damage, and interstitial fibrosis [1–3]. At present, kidney biopsy is the only method to evaluate histopathological changes in chronic glomerulonephritis. However, biopsy is an invasive procedure and may cause complications, and thus non-invasive imaging techniques are needed.
Diffusion-weighted imaging (DWI) of the kidney is a feasible approach in the characterization of renal diseases and is used in an increasing number of studies [4–10]. DWI visualizes water motion at the molecular level and provides useful information on parenchyma microstructure and function, with the major advantages of not using ionizing radiation or potentially nephrotoxic contrast agents [11, 12]. The apparent diffusion coefficient (ADC) is a quantitative parameter calculated from MR-DWI images, which is altered by various physiological and pathological conditions of the renal system. Previous studies have shown that ADC values are decreased in chronic kidney disease, depending upon the degree of renal function impairment [13–15]. Togao et al. [16] demonstrated a relationship between decreased ADC and renal fibrosis.
The predominant function of the kidneys is to transport water, and the anisotropic diffusion properties in the kidneys are the result of structures such as vessels, tubules, and collecting ducts that are oriented in a radial fashion [17]. Diffusion is a three-dimensional process, and molecular mobility in organized tissue is not necessarily the same in all directions. DWI does not allow analysis of diffusion in multiple directions, but tissue anisotropy can be analysed using diffusion tensor imaging (DTI), which provides additional information on diffusion direction and degree of directed diffusion (fractional anisotropy, FA) by analysing water diffusion in different directions. DTI was first used by Ries et al. in the kidneys of healthy volunteers [18]. Renal DTI has recently been used for the detection of allograft dysfunction in humans and ischemia-reperfusion injury in a rat model, in which FA was significantly reduced [19, 20].
The purpose of this study was to investigate whether DTI can be used to assess renal function and to determine the correlation between diffusion anisotropy and the degree of renal pathology in disorders such as glomerulosclerosis and tubulointerstitial fibrosis in patients with chronic glomerulonephritis.
Materials and methods
The study population
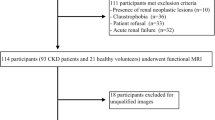
A total of 75 patients (39 men and 36 women) admitted to the nephrology department in our hospital were retrospectively recruited to participate in this study. Patients had chronic kidney disease (CKD) stages 1 to 5, with 15 cases per stage. Kidney biopsies were performed in all patients with CKD stage 1–3; biopsy was performed in only one patient with stage 4 CKD. Before renal biopsy, all subjects underwent functional MRI and laboratory tests, and MRI scans were performed within seven days of hospital admission. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) formula for Chinese subjects, which is eGFR (mL/min per 1.73 m2) = 186 × (Scr)-1.154 × (age)-0.203 × 1.233 × (0.742 if female), as recommended by the Chinese Society of Nephrology. The diagnosis of CKD was based on a chronic decline in eGFR (<60 ml/min per 1.73 m2) and was classified into stages as follows: stage 1, eGFR >90; stage 2, 60–89; stage 3, 30–59; stage 4, 15–29; and stage 5, <15. Chronic glomerulonephritis was diagnosed based on clinical history, laboratory findings, and renal biopsy results. Twenty volunteers with no history of renal disease, hypertension, diabetes, or vascular disease were included in the study. The study was approved by the local ethics committee, and informed consent was obtained from the participants prior to MRI examination.
MR protocol
All examinations were performed using a 1.5 T whole-body scanner (MAGNETOM Avanto, Siemens Healthcare, Erlanger, Germany) with a maximum gradient strength of 45 mT/m, a minimum rise time of 225 μs, and 32 receiver channels. For DTI, fat-saturated coronal EPI sequences were performed in six directions using the Siemens multidirectional diffusion-weighted protocol with b-values of 0–600 s/mm2.
The remaining parameters for respiratory-triggered imaging were as follows: 10 slices; slice thickness, 6 mm with no intersection gap; TR, 1400 ms; TE, 76 ms; bandwidth, 1370 Hz/pixel; field of view in read direction, 400 mm; field of view in phase direction, 100 %; voxel size, 2.1 × 2.1 × 6 mm3; partial Fourier factor, 6/8; number of excitations (NEX), 4; phase encoding direction, left to right; k-spaced parallel imaging technique, GRAPPA with an acceleration factor 2; and acquisition time, 2 minutes 4 seconds to 3 minutes. The kidneys were imaged consecutively with 10 slices in an oblique coronal orientation, slightly tilted, parallel to the long axis of the kidney.
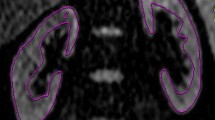
MR data analysis
Images were analysed on an external workstation using Syngo software (Siemens Healthcare) by two readers who were blinded to histopathological and laboratory findings. For DTI analysis, the commercially available Neuro 3D Task Card software (Siemens Healthcare) was used. The diffusion tensor was determined by the orientation and magnitude of diffusion. The degree of diffusion anisotropy was calculated and depicted in parameter maps of FA; apparent diffusion coefficient maps were calculated based on a mono-exponential fitting model. On ADC maps of the same kidney, two authors measured the parenchyma and three regions of interest (ROIs) from the upper, middle, and lower pole of the cortex and medulla. ROIs with a size of 10–50 pixels each were placed into the cortex and medulla of the kidney and were copied to FA maps (Fig. 1). Mean ADC and FA values were determined separately in all patients. The ADC and FA values in parenchyma were also measured.
Histology
Formalin-fixed kidney tissue was embedded in paraffin. Coronal sections (2 μm) were prepared and were subjected to Masson staining to visualize the accumulation of tubulointerstitial fibrosis and tubular damage. Periodic acid-silver methenamine (PASM) staining was used to determine glomerulosclerosis and mesangial expansion within renal glomeruli. For quantification of tubulointerstitial fibrosis and tubular damage, 10 representative images of each patient were evaluated. The percentage of Masson-positive area per total tissue area was used as a measure of tubulointerstitial fibrosis. For the assessment of glomerulosclerosis, 10 representative glomeruli in each patient were evaluated, and the mesangial index was expressed as the percentage of PASM-positive area per total glomerular tuft area. Renal histology was analysed by one author.
Statistical analysis
Statistical analysis was performed using SPSS 13.0. Values are given as mean and standard deviations. P values of 0.05 were considered statistically significant. The consistency of measurements between the two authors was assessed using the Kappa test. Mean values for physiological parameters, histology, ADC, and FA within the groups were calculated. Parameters were compared among groups using one-way analysis of variance (ANOVA), followed by post hoc multiple comparison with the Fisher LSD test. Within the groups, FA and ADC values in the renal cortex and medulla layers were compared using the paired t-test. The correlation between histopathological parameters and FA and ADC values in the anatomical layers was determined by linear regression analysis (r is the regression coefficient).
Results
Trend of renal ADC and FA values among stages
For each patient, the image quality of renal DTI was satisfactory for further evaluation, with no motion artefacts, distortion artefacts, or morphological abnormalities. With regard to the ADC value in renal parenchyma, cortex, and medulla, the consistency of the two authors was high (r = 0.88, 0.90, and 0.91, respectively), similar to that for the FA value (r = 0.84, 0.87, 0.91, respectively). The ADC and FA values were obtained in five different disease stages (Table 1, Fig. 2). The ADC value in the renal parenchyma ranged from 1.86 to 2.33 × 10-3 mm2/s. The FA value in the renal parenchyma ranged from 0.18 to 0.27. The ADC and FA values tended to decrease with increased disease stage (Fig. 3), and significant differences were observed among the five different stages. The ADC and FA values were not statistically different between the control group and stage 1 patients (P = 0.52 and 0.54, respectively). Significant differences between the control group and stage 2–5 patients were observed (P = 0.00), similar to the differences between stage 1 and stage 2–5, stage 2 and stage 3–5, stage 3 and stage 4–5, and stage 4 and stage 5 patients. Significant differences were also found in Scr and eGFR (P = 0.00).
ADC map (A–E) and FA map (F–J) in different disease stages, with A–E and F–J each representing stages 1–5. On ADC maps, low signal area of renal medulla decreased with increased stages. On FA maps, high signal area of renal medulla decreased with increased stages. The difference between cortex and medulla were significantly reduced with increasing disease stage. In stage 1, low signal area of renal medulla on ADC maps and high signal area of renal medulla on FA maps were obvious; in stages 4 and 5, renal cortex and medulla were not differentiated
Corticomedullary gradient of ADC and FA values among stages
Due to a lower difference between the cortex and medulla and lower significance of renal biopsy, patients with stage 4 and 5 CKD were not analysed. The cortex and medulla layers of the kidney were identified on MRI in stage 1–3 patients. In general, the ADC was significantly lower in the medulla than in the cortex in the different stages (P < 0.05). Inversely, FA was significantly higher. ADC and FA were significantly reduced with increasing stage (P < 0.05).
In stage 1–3 patients, ADC values in the cortex and medulla were found to be statistically different, similar to the FA values in the cortex and medulla (Table 2).
Histopathology of chronic glomerulonephritis
From stage 1 to stage 3, the percentage of the PASM-positive area per total glomerular tuft area was 8.21 ± 2.15, 18.27 ± 2.37, and 28.4 0 ± 3.14, respectively, and significant differences among the groups were observed (F = 228.13, P < 0.05). The percentage of the Masson-positive area per total tissue area was 8.58 ± 1.60, 17.73 ± 1.83, and 27.41 ± 2 .77, respectively (F = 228.13, P < 0.05). The comparisons among the groups showed statistical differences, indicating that glomerulosclerosis and tubulointerstitial fibrosis significantly increased with higher disease stage (Fig. 4).
Histology of chronic glomerulonephritis. The degree of magnification is 200. A–D and E–H each represent stages 1–4. (A–D) PASM-stained sections of the renal cortex show progressive glomerular changes, such as glomerulosclerosis (black area within the glomerular tuft). (E–H) Masson-stained section reveals progressive tubulointerstitial fibrosis, i.e., increased Masson-positive (blue) area
Correlation between ADC/FA values and renal histopathology
Significant negative correlations between the percentage of glomerulosclerosis and FA in the renal cortex and medulla were observed (r = -0.74, -0.70, respectively, P < 0.05). Correlations between glomerulosclerosis and ADC in the renal cortex and medulla were also observed (r = -0.65, -0.66, respectively, P < 0.05). The degree of tubulointerstitial fibrosis was negatively correlated with FA in the medulla and renal cortex (r = -0.76, -0.70, respectively, P < 0.05). Correlations were also found between tubulointerstitial fibrosis and ADC in the medulla and renal cortex (r = -0.68, -0.67, respectively, P < 0.05).
Discussion
To date, there are only a few studies investigating the value of DTI in the assessment of renal disease. Measurements of DTI parameters within the kidneys, such as ADC and FA, have shown high repeatability and reproducibility, with low inter- and intra-observer variability, in healthy volunteers [21, 22].
In the present study, we demonstrated that the ADC and FA values reflected the level of renal function and the degree of histopathological changes. There were significant differences in renal ADC and FA values at different disease stages. A possible reason for this is that renal function was assessed using the MDRD formula for Chinese subjects [23], which is more sensitive and more accurate than the original MDRD formula. In the renal parenchyma, the ADC value decreased with higher disease stage, indicating a correlation between chronic kidney disease and ADC value, which is in accordance with previous studies [14–16]. The pathology of chronic glomerulonephritis, such as glomerulosclerosis and tubulointerstitial fibrosis, leads to a reduction in blood flow and blood perfusion, resulting in a decrease in the amount of global diffusivity. The FA value in the parenchyma decreased with higher disease stage. A possible explanation for this is the fact that glomerulosclerosis and tubulointerstitial fibrosis destroy renal anisotropic architecture.
Magnetic resonance DTI demonstrated higher ADC values in the cortex than the medulla, and significantly higher FA values in the medulla than in the cortex. These findings were consistent with renal anatomy in previous studies [11, 20]. It has been shown that cortical and medullary FA is reduced in transplanted kidneys compared with normal kidneys and that medullary FA correlates with eGFR [19]. In a rat model, Cheung et al. observed a reduction in medullary FA five hours after ischemia-reperfusion injury, which was associated with cellular oedema and necrosis at histology. Hueper et al. [24] found a significant negative correlation between the reduction in FA and pathologies in diabetic nephropathy, and concluded that these pathologies impaired diffusion along the radially oriented tubules, which explained the reduction in FA. Lu et al. [25] found that medullary FA was reduced in diabetic patients, with and without impaired renal function, when compared with controls, indicating the value of DTI for the early identification of diabetic nephropathy. To date, the histopathological correlation with chronic glomerulonephritis has not been demonstrated.
In our study, renal biopsies were performed in patients with stage 1 to 3 CKD, as early intervention can reverse chronic nephritis and delay pathological changes, whereas advanced pathological changes are irreversible in patients with stage 4 and 5 CKD. In stages 1 to 3, we were able to demonstrate that histopathological changes of chronic glomerulonephritis such as glomerulosclerosis and interstitial fibrosis were negatively correlated with ADC and diffusion anisotropy (FA) in MR DTI, and therefore three stages of chronic glomerulonephritis were evaluated in the present study. In our study, quantification of diffusion anisotropy revealed that the FA in various anatomical layers was significantly reduced in patients with chronic glomerulonephritis compared to lower disease stages, indicating restriction of directed diffusion.
The mechanisms of renal pathologies that act to decrease diffusion anisotropy, however, remain unclear. One theory is that tubular dilatation in chronic glomerulonephritis removes some of the directionality of diffusivity along the tubules, thereby contributing to FA restriction. Furthermore, tubular dilatation and glomerulosclerosis are associated with cellular damage and renal dysfunction, which may influence diffusion direction. Cellular debris might, for example, congest the tubules and thus impair directed diffusion. Interestingly, FA reflects the pathological changes in the kidney with potentially greater sensitivity than ADC, as different pathologies were correlated with FA in specific anatomical layers. Quantifying diffusion parameters separately for each anatomical layer, as performed in this study, may help to differentiate renal pathologies. Similar to what was demonstrated in the study by Gaudiano et al. [26], FA value appears to be the more useful parameter for assessing renal damage.
The shortcomings of the current study are as follows. Firstly, this study did not include different pathological types of chronic nephritis, which influence disease outcome. Secondly, we did not evaluate the sensitivity of ADC and FA values using statistical methods. The results from the present study will be further used to test renal function and pathology in a study using statistical methods.
In conclusion, MR DTI identified renal pathologies associated with chronic glomerulonephritis by showing reduced ADC and FA values, representing different stages of disease. Diffusion anisotropy was negatively correlated with the degree of glomerulosclerosis and interstitial fibrosis. Therefore, MR DTI may be valuable for non-invasive monitoring of chronic glomerulonephritis.
References
Chen HZ, Zhong NS, Lu ZY (2013) Internal medicine. People’s Medical Publishing House, Beijing
Xie J, Chen N (2013) Primary glomerulonephritis in mainland China: an overview. Contrib Nephrol 181:1–11
Proletov I, Saganova ES, Galkina OV et al (2013) Diagnostic value of cystatin C and neutrophil gelatinase-associated lipocalin in primary glomerulopathies. Ter Arkh 85:10–16
Gilet AG, Kang SK, Kim D, Chandarana H (2012) Advanced renal mass imaging: diffusion and perfusion MRI. Curr Urol Rep 13:93–98
Jost G, Lenhard DC, Sieber MA, Lengsfeld P, Hütter J, Pietsch H (2011) Changes of renal water diffusion coefficient after application of iodinated contrast agents: effect of viscosity. Invest Radiol 46:796–800
Desar IM, Voert EG, Hambrock T et al (2011) Functional MRI techniques demonstrate early vascular changes in renal cell cancer patients treated with sunitinib: a pilot study. Cancer Imaging 11:259–265
Zhang JL, Sigmund EE, Rusinek H, Chandarana H, Storey P, Chen Q (2012) Optimization of b-value sampling for diffusion weighted imaging of the kidney. Magn Reson Med 67:89–97
Ding J, Xing W, Chen J et al (2014) Evaluation of signal noise ratio on analysis of clear cell renal cell carcinoma using DWI with multi-b values. Zhonghua Yi Xue Za Zhi 94:171–173, Article in Chinese
Haneder S, Boda-Heggemann J, Schoenberg SO, Michaely HJ (2012) Functional magnetic resonance imaging for evaluation of radiation-induced renal damage. Radiologe 52:243–251, Article in German
Yu X, Lin M, Ouyang H, Zhou C, Zhang H (2012) Application of ADC measurement in characterization of renal cell carcinomas with different pathological types and grades by 3.0 T diffusion-weighted MRI. Eur J Radiol 81:3061–3066
Notohamiprodjo M, Glaser C, Herrmann KA, Dietrich O, Attenberger UI, Reiser MF et al (2008) Diffusion tensor imaging of the kidney with parallel imaging: initial clinical experience. Invest Radiol 43:677–685
Palmucci S, Mauro LA, Veroux P, Failla G, Milone P, Ettorre GC (2011) Magnetic resonance with diffusion-weighted imaging in the evaluation of transplanted kidneys: preliminary findings. Transplant Proc 43:960–966
Carbone SF, Gaggioli E, Ricci V et al (2007) Diffusion-weighted magnetic resonance imaging in the evaluation of renal function: a preliminary study. Radiol Med 112:1201–1210
Xu X, Fang W, Ling H et al (2010) Diffusion-weighted MR imaging of kidneys in patients with chronic kidney disease: initial study. Eur Radiol 20:978–983
Inoue T, Kozawa E, Okada H et al (2011) Noninvasive evaluation of kidney hypoxia and fibrosis using magnetic resonance imaging. J Am Soc Nephrol 22:1429–1434
Togao O, Doi S, Kuro-o M et al (2010) Assessment of renal fibrosis with diffusion weighted MR imaging: study with murine model of unilateral ureteral obstruction. Radiology 255:772–780
Mannelli L, Valentino M, Laffi G, Lomas DJ, Sigmund EE, Raz E et al (2010) Functional MRI of the kidney. G Ital Nefrol 27:599–608
Ries M, Jones RA, Basseau F, Moonen CT, Grenier N (2001) Diffusion tensor MRI of the human kidney. J Magn Reson Imaging 14:42–49
Hueper K, Gutberlet M, Rodt T et al (2011) Diffusion tensor imaging and tractography for assessment of renal allograft dysfunction-initial results. Eur Radiol 21:2427–2433
Cheung JS, Fan SJ, Chow AM et al (2010) Diffusion tensor imaging of renal ischemia reperfusion injury in an experimental model. NMR Biomed 23:496–502
Notohamiprodjo M, Dietrich O, Horger W et al (2010) Diffusion tensor imaging (DTI) of the kidney at 3 tesla-feasibility, protocol evaluation and comparison to 1.5 Tesla. Invest Radiol 45:245–254
Cutajar M, Clayden JD, Clark CA et al (2011) Test-retest reliability and repeatability of renal diffusion tensor MRI in healthy subjects. Eur J Radiol 80:e263–e268
Chinese eGFR Investigation Collaboration (2006) Modification and evaluation of MDRD estimating equation for Chinese patients with chronic kidney disease. Chin J Nephrol 22:589–595
Hueper K, Hartung D, Gutberlet M et al (2012) Magnetic Resonance Diffusion Tensor Imaging for evaluation of histopathological changes in a rat model of diabetic nephropathy. Investig Radiol 47:430–437
Lu L, Sedor JR, Gulani V et al (2011) Use of diffusion tensor MRI to identify early changes in diabetic nephropathy. Am J Nephrol 34:476–482
Gaudiano C, Clementi V, Busato F (2013) Diffusion tensor imaging and tractography of the kidneys: assessment of chronic parenchymal diseases. Eur Radiol 23:1678–1685
Acknowledgments
The scientific guarantor of this publication is Qiang Feng. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: retrospective randomised controlled trial, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feng, Q., Ma, Z., Wu, J. et al. DTI for the assessment of disease stage in patients with glomerulonephritis - correlation with renal histology. Eur Radiol 25, 92–98 (2015). https://doi.org/10.1007/s00330-014-3336-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3336-1