Abstract
Objectives
To determine the potential of novel gradient echo parameters, “Black Bone” MRI as an alternative to CT in the identification of normal and prematurely fused cranial sutures both in 2D and 3D imaging.
Methods
Thirteen children with a clinical diagnosis of craniosynostosis underwent “Black Bone” MRI in addition to routine cranial CT. “Black Bone” datasets were compared to CT and clinical findings. “Black Bone” imaging was subsequently used to develop 3D reformats of the craniofacial skeleton to enhance further visualisation of the cranial sutures.
Results
Patent cranial sutures were consistently identified on “Black Bone” MRI as areas of increased signal intensity. In children with craniosynostosis the affected suture was absent, whilst the remaining patent sutures could be visualised, consistent with CT and clinical findings. Segmentation of the “Black Bone” MRI datasets was successful with both threshold and volume rendering techniques. The cranial sutures, where patent, could be visualised throughout their path.
Conclusions
Patent cranial sutures appear as areas of increased signal intensity on “Black Bone” MRI distinct from the cranial bone, demonstrating considerable clinical potential as a non-ionising alternative to CT in the diagnosis of craniosynostosis.
Key Points
• Patent cranial sutures appear hyperintense on “Black Bone” MRI
• Prematurely fused cranial sutures are distinct from patent sutures
• Minimal soft tissue contrast permits 3D-rendered imaging of the craniofacial skeleton
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Craniosynostosis, the premature fusion of one or more of the cranial sutures, occurs in approximately 1 in 2,100 to 1 in 2,500 infants, and results in characteristic skull shape deformities. Such deformity usually requires surgical intervention to prevent progressive distortion and raised intracranial pressure (ICP) [1–3]. Whilst certain skull shapes are often suggestive of the underlying synostosis, diagnostic imaging is justified to confirm patency of the remaining sutures, assess for intracranial pathology, and evidence of raised intracranial pressure.
The literature is currently replete with concern regarding repeated CT examination particularly in young patients with benign conditions [4–8]. Infants with craniosynostosis make up one such patient group where repeated imaging throughout childhood is often required. Whilst some authors have argued that the risks of ionising radiation have been overestimated due to flaws associated with dose calculation, others have suggested that CT examination is not justified in craniosynostosis [9–11]. However, in view of the significant morbidity and mortality associated with surgery, confirmatory diagnostic imaging remains justified and is standard practice at the majority of craniofacial units worldwide. Since CT examination is undertaken during infancy and childhood, any potential adverse effects of ionising radiation are more likely to be encountered due to the prolonged time period over which these can be expressed.
MRI offers a potential non-ionising alternative to CT, but routine sequences have been shown to be unreliable in the identification of the cranial sutures in infants [12]. Surgeons have become accustomed to 3D-reconstructed CT images of the craniofacial skeleton facilitated by technical advances in post-processing, which has permitted surface and volume rendering with minimal effort and expertise, enhancing diagnostic and surgical planning capabilities. Whilst MRI is increasingly used for 3D reconstruction of soft tissue structures, particularly the brain, attempts at segmentation of bone of the craniofacial skeleton have been limited. The simple rendering methods employed for CT data are frequently inadequate for MRI due to overlapping pixel values of adjacent tissues. Whilst not an essential facet for diagnosis, an MRI technique unable to provide comparable 3D reconstruction of the craniofacial skeleton to CT, irrespective of the ionising radiation benefits, is unlikely to be accepted by clinicians. As a result, CT has largely remained the investigation of choice for craniofacial imaging, albeit with attempts made to minimise radiation dose, including very low-dose techniques combined with MRI [13, 14]. The ability to use an additional short acquisition time MRI sequence to provide both diagnostic information and 3D-reconstructed bone anatomy would have a profound impact upon craniofacial imaging worldwide.
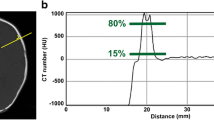
“Black Bone” MRI utilises novel gradient echo parameters optimised to minimise soft tissue contrast to enhance the bone-soft tissue boundary. This is achieved by using 3D volume acquisition, a short TE, TR, and low flip angle (Table 1, Fig. 1) [15, 16]. As a result, imaging times are short, with the average time to acquire “Black Bone” images of the craniofacial skeleton being 4 min. The technique has been demonstrated to be of value in the investigation of a range of pathologies affecting the head and neck region [15–17].
The objectives of this study were to determine the potential of “Black Bone” MRI in the identification of normal and prematurely fused cranial sutures and the feasibility of the sequence in 3D reconstructions of the craniofacial skeleton.
Materials and methods
Ethical approval was granted from the Oxfordshire Research Ethics Committee, and written informed consent was obtained from all participants and/or their parents for recruitment to the “Black Bone” MRI study. In collaboration with the Oxford Craniofacial Unit, children with a clinical diagnosis of craniosynostosis were identified. The Oxford Craniofacial Unit is one of four designated specialist craniofacial units in the UK seeing approximately 70 new cases of craniosynostosis per year. Standard local practice includes CT examination with 3D reconstruction in all clinical cases of craniosynostosis; general anaesthesia is used for any child unable to remain still for the examination.
Between December 2011 and May 2012 patients were recruited in four cohorts: (1) infants where CT examination under general anaesthesia was required (n = 9); (2) infants where CT and MRI could be acquired without general anaesthesia (n = 1); and (3) children in whom synostosis had previously been confirmed on CT and in whom general anaesthesia would not be required for MRI examination (arbitrarily set as any child over 8 years of age) (n = 3). The final cohort (4) acted as the control group and consisted of children in whom the cranial sutures were normal, undergoing MRI examination of the head and neck without CT examination (n = 4). This resulted in a total of 17 “Black Bone” datasets.
“Black Bone” MRI examination in 16 of the 17 children was completed on a 1.5 T magnet, and in the final child on a 3 T magnet (GE Medical Systems, Milwaukee, IL, USA or Philips Healthcare, Andover, MA, USA). An 8-channel head coil (GE Medical Systems, Milwaukee, IL, USA or Philips Healthcare, Andover, MA, USA) was used in all cases. Imaging was acquired in the axial plane from above the skull vertex to below the mandible, with post-processing in the coronal and sagittal planes. In view of the potential for intracranial pathology in children with craniosynostosis, axial T2 imaging was acquired of the brain. In cohort (1) MRI examination was completed prior to transfer of the child to the adjacent CT scanner, whilst still under general anaesthesia.
The “Black Bone” images were reviewed on an Advantage Windows Workstation (GE Medical Systems, Milwaukee, IL, USA) to determine the characteristics of the patent and prematurely fused cranial sutures. Comparison was made to the clinical diagnosis and CT findings. This initial review was undertaken in an unblinded manner by the first author.
To provide preliminary information on the potential diagnostic benefits of the technique, blinded review of imaging was undertaken by a consultant neuroradiologist with a specialist interest in craniofacial anomalies. Of the 17 “Black Bone” datasets, five were excluded from review in view of significant movement artefact (n = 1), extensive tumour obscuring visualisation of the cranial sutures (n = 1), and a combination of chemical shift artefact and non-optimised parameters (n = 3) (Table 2). The datasets were imported into Clear Canvas (Version 2.0 [open source], Clear Canvas Inc, Toronto, Canada) for anonymisation with assignment of a random unique identifier before export to Efilm (Version 1.8.3, Merge Healthcare, Chicago, IL, USA). All identifying information, including the series descriptors, was removed. The assessor was asked to grade each cranial suture (sagittal, metopic, left and right coronal, and left and right lambdoid sutures) on a 3-point scale for its identification and to conclude whether there was evidence of synostosis for any of the sutures. A score of 0 was assigned where the suture could not be identified, 1 where it was partially identifiable, and 2 where it was clearly identifiable and the assessor confident of its presence. The assessor was informed that the 12 datasets had all been obtained from children with either normal sutures or craniosynostosis and was asked to disregard any co-existent pathology, thus concentrating only on the cranial sutures. Review of imaging was undertaken on Efilm, with the assessor free to manipulate images on screen. The process was repeated after a period of 6 months, and the intra-observer variability calculated using Kappa co-efficient.
To assess further the results in clinical context, blinded review was undertaken by a consultant radiologist specialising in head and neck pathology, but not neuroradiology, and a consultant head and neck surgeon. Both assessors are highly experienced in their field, but “non-expert” in the evaluation of cranial sutures, thus representing the average level of experience among clinicians and radiologists at referring non-craniofacial specialist units. Assessment was conducted using the same 3-point scale.
Investigation was completed using two main techniques of 3D reconstruction – thresholding (Mimics Version 14.01, Materialise, Leuven, Belgium ), and volume rendering (Fovia High Definition Volume Rendering software, Fovia Inc, Palo Alto, CA, USA) using all of the available “Black Bone” datasets. Comparison was made to the corresponding 3D CT images with further assessment of the appearance of the cranial sutures in a non-blinded manner by the first author.
Results
In the four children with normal cranial sutures, the sutures were identified as areas of increased signal intensity, easily distinguished from the signal void of the cranial bone. The sutures could be followed throughout their course in most cases. Where still present, the anterior fontanelle was of the same signal intensity as the cranial sutures (Fig. 2). The bone was distinct from the surrounding soft tissues, albeit being slightly less well defined when compared to imaging obtained from adults (Fig. 1) [15].
In the 13 children with a clinical diagnosis of craniosynostosis, the patent cranial sutures were again visualised as areas of increased signal intensity, but the suture absent at the site of synostosis. The findings were consistent with CT (Fig. 3a-c). Imaging was acquired in all but one child on a 1.5 T magnet. Patient 12 was imaged without general anaesthesia on a 3 T magnet. There was significant movement artefact, which in combination with the particularly thin cranial bone in this child with Apert syndrome, made distinction of the cranial sutures challenging.
Axial and coronal CT (a), axial and coronal “Black Bone” MRI (b), 3D CT (c), and 3D “Black Bone” imaging using Mimics (d) and Fovia (e). The sutures are indicated by arrows (Sagittal suture = green; Coronal suture = yellow; Lambdoid suture = blue; Metopic suture = red) and the site of synostosis indicated with a black arrow A) Images from a child with metopic synostosis (Patient 13). B) Images from a child with right unicoronal synostosis (Patient 11). C) Images from a child with sagittal synostosis (Patient 5). Row E (centre and second from right) demonstrates visualisation of the cranial sutures without the need for segmentation of the soft tissues with Fovia
With increasing age (>10 years), the bone surrounding the cranial sutures demonstrated decreased intensity beyond the expected cranial suture width. Central to this there was usually an area of increased signal representing the suture per se (Fig. 4).
Axial and coronal CT (A) and axial and coronal “Black Bone” imaging (B) from a 12 year old child with sagittal synostosis (Patient 7). Note the increased intensity surrounding the cranial sutures. The coronal (yellow arrows) and lambdoid (blue arrows) sutures can be seen, but there is absence of the sagittal suture (black arrow)
The diagnoses assigned on blinded review by the expert assessor are shown in Table 3. The correct diagnosis was made in all 12 cases on both occasions (Kappa co-efficient =1; Perfect agreement). In the absence of synostosis, a score of 2 was assigned for all sutures, apart from the metopic suture, which could only be seen in two cases, consistent with CT imaging.
The results for the two non-expert reviewers are also shown in Table 3. The inter-rater reliability for diagnosis was found to be Kappa = 0.70. The mean scores assigned by the reviewers for each of the cranial sutures on the “Black Bone” datasets are shown in Table 4. Synostosed sutures received the lowest mean scores, consistent with an inability to visualise the suture, despite this not always being identified by the non-expert reviewers as a diagnosis of craniosynostosis.
The 3D reconstructed images of the craniofacial skeleton created from “Black Bone” datasets of three children with craniosynostosis are shown in Fig. 3a-c. To produce these reformats within Mimics, a threshold mask was selected so that the bone was contained within the upper and lower threshold limits. Since this threshold limit also included the surrounding air, the mask was edited using a combination of multiple-slice edit and 3D edit functions. These editing processes resulted in this technique being time intensive. In Fovia, the transfer function and segmentation tools were used in combination. A transfer function was initially applied, thereby assigning a colour and opacity to each pixel, and the soft tissues were removed from the underlying bone using the surface layer removal tool. This process was less intensive than with Mimics. It was noted that clear visualisation of the cranial sutures could be achieved without the need for segmentation and images could be created using a transfer function preset very rapidly (Fig. 3c). Three-dimensional reconstruction of the craniofacial skeleton was possible in the 12 optimal “Black Bone” datasets. In the remaining five cases, in view of non-optimised parameters, movement artefact, and distortion from tumour, unaffected regions of the craniofacial skeleton were successfully reconstructed.
Discussion
Children with craniosynostosis are of concern in terms of radiation exposure from CT due to their young age at investigation, the benign nature of craniosynostosis, and inevitable exposure of the radiosensitive lens and thyroid during imaging. In this study, we have shown that “Black Bone” MRI offers a potential alternative to ionising radiation in this patient group.
On “Black Bone” MRI the cranial sutures were seen as areas of increased signal intensity, making them distinct from the surrounding signal void of the bone. The sutures were confirmed by their characteristic tortuosity, and in younger patients, the convergence of the coronal and sagittal sutures at the anterior fontanelle. In children with craniosynostosis, the patent sutures were seen as areas of increased signal intensity, with these features being absent at the site of synostosis. The findings on “Black Bone” MRI were consistent with both the clinical diagnosis and the CT findings.
With increasing age, it was noted that the bone surrounding the cranial suture often appeared as areas of decreased signal intensity compared to the remaining cranial bone on the “Black Bone” datasets. Whilst in children the increased intensity of the patent intervening suture could be identified, it was noted that in adolescents and adults this increased intensity was usually absent. This appears to represent the normal progression of cranial suture appearance on “Black Bone” MRI with advancing age. It should be noted that since the diagnosis of craniosynostosis is usually made in infancy, this variability in suture appearance is of limited significance in this patient cohort.
Independent blinded review demonstrated that “Black Bone” MRI was accurate in the distinction between normal and prematurely fused sutures. The metopic suture was the least frequently identified suture consistent with the age of the patients studied; the metopic suture being the only cranial suture to close physiologically before 9 months of age [18]. A score of 2 (suture fully identified and confident of its presence) was often selected for the remaining sutures. This was in contrast to the results of a similar study exploring the use of routine MRI sequences for the identification of cranial sutures, where the cranial sutures were infrequently identified [12].
Of the sutures reviewed, the sagittal suture was most problematic in view of its close proximity to the superior sagittal sinus. This resulted in some difficulty for the non-expert reviewers when this suture was synostosed since both the cranial suture and superior sagittal sinus are seen as areas of signal void on routine MRI sequences. In most cases, the diagnosis assigned was correct and the cranial sutures identified with confidence. Of the 12 datasets reviewed, those with synostosis (n = 9) were consistently assigned the lowest scores. This confirms that the absence of these sutures was distinguished from normal sutures, thus raising suspicion of synostosis. Since the “non-experts” involved in the study are not regularly involved in the reporting of imaging from infants with a diagnosis of craniosynostosis, they were unlikely to have used other subtle findings such as head shape to aid their diagnostic capabilities. It is assumed, however, that the correct diagnosis would have been assigned by the reviewers on blinded review of the CT datasets, since the reviewers are familiar with bone imaging on CT.
The main limitation of this study is the small number of recruited patients. Wherever possible CT examination is completed without general anaesthesia, and anesthetising a child solely for research could not be ethically justified. The combination of a wide geographical referral base and a necessity to complete the study outside of routine NHS working hours made recruitment of suitable patients challenging. This was compounded by some initial difficulty when transferring “Black Bone” MRI from scanners of one manufacturer to another, to obtain consistent comparable results. As a result, some of the initial datasets were not fully optimised or were degraded by chemical shift artefact. These datasets and those with significant movement artefact or intracranial pathology encroaching upon the cranial sutures were excluded from independent review, further reducing the number of datasets available. Since the cohort of children recruited to this study were the first patients with craniosynostosis to undergo “Black Bone” imaging, it was not possible for assessors to be provided with datasets to become familiar with cranial suture identification on “Black Bone” MRI outside of the blinded study. As with any new technique, there is an inevitable learning curve potentially impacting the results of the independent review.
Whilst MRI eliminates the risks of ionising radiation, consideration needs to be given to other potential risks associated with MRI. This includes the requirement for general anaesthesia or sedation in young children, both with their own inherent risks within the MRI environment. One of the main limitations of “Black Bone” MRI compared to CT is that imaging in regions of an air-bone interface such as the mastoid region and paranasal sinuses is inferior to that on CT since the pixel values cannot be distinguished. This is rarely problematic in craniosynostosis, as this is not in an area of interest, and is offset by improved brain imaging.
Three-dimensional imaging is particularly useful in surgical planning, and Tartaro et al [19] reported the improvement in cranial sutures seen on 3D CT with results of 90.7 – 100 % compared to 83.7 – 95.5 % on axial CT imaging. Whilst not an essential facet for diagnosis, an MRI technique unable to provide comparable 3D reconstruction to CT irrespective of the ionising radiation benefits is unlikely to be accepted by clinicians. The initial results obtained from segmentation/volume rendering of the craniofacial skeleton from “Black Bone” datasets demonstrate considerable potential. The techniques used are very basic image processing methods providing considerable scope for further refinement and advancement.
Since the 3D reconstruction techniques had not been fully standardised across the datasets, these were not included in the blinded study to avoid any potential bias due to subtleties in results. This provides scope for further evaluation following further validation of 3D techniques in a range of craniosynostosis cases including syndromic patients.
The fundamental difficulty in the majority of hospitals in attempting to replace CT with MRI in this patient group is the increased demands which would be placed upon MRI imaging time particularly when additional time for sedation or anaesthesia is required. In those children requiring MRI examination of the brain, the addition of “Black Bone” MRI to the imaging protocol negates the need for an additional CT. It is this sub-set of patients where “Black Bone” MRI offers improved cost-effectiveness and where it is most likely to find its place. However, the reason for this study was to provide a viable non-ionising alternative of imaging, and the sequence should be considered as an alternative to CT particularly when it is likely that multiple examinations will be required throughout childhood.
In conclusion, “Black Bone” MRI appears useful and accurate in the identification of cranial sutures and diagnosis of craniosynostosis demonstrating considerable clinical potential as a non-ionising alternative to CT.
References
Lajeunie E, Le Merrer M, Bonaiti-Pellie C, Marchac D, Renier D (1995) Genetic study of nonsyndromic coronal craniosynostosis. Am J Med Genet 55:500–4
Wilkie AO, Byren JC, Hurst JA, Jayamohan J, Johnson D, Knight SJ, Lester T, Richards PG, Twigg SR, Wall SA (2010) Prevalence and complications of single-gene and chromosomal disorders in craniosynostosis. Pediatrics 126:e391–400
Boulet SL, Rasmussen SA, Honein MA (2008) A population-based study of craniosynostosis in metropolitan Atlanta, 1989-2003. Am J Med Genet A 146A:984–91
Domeshek LF, Mukundan S Jr, Yoshizumi T, Marcus JR (2009) Increasing concern regarding computed tomography irradiation in craniofacial surgery. Plast Reconstr Surg 123:1313–20
Brenner DJ, Hall EJ (2012) Cancer risks from CT scans: now we have data, what next? Radiology 265:330–1
Journy N, Ancelet S, Rehel JL, Mezzarobba M, Aubert B, Laurier D, Bernier MO (2014) Predicted cancer risks induced by computed tomography examinations during childhood, by a quantitative risk assessment approach. Radiat Environ Biophys 53:39–54
Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW, Parker L (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505
Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, Giles GG, Wallace AB, Anderson PR, Guiver TA, McGale P, Cain TM, Dowty JG, Bickerstaffe AC, Darby SC (2013) Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360
Engel M, Castrillon-Oberndorfer G, Hoffmann J, Freudlsperger C (2012) Value of preoperative imaging in the diagnostics of isolated metopic suture synostosis: a risk-benefit analysis. J Plast Reconstr Aesthet Surg 65:1246–51
Engel M, Hoffmann J, Muhling J, Castrillon-Oberndorfer G, Seeberger R, Freudlsperger C (2012) Magnetic resonance imaging in isolated sagittal synostosis. J Craniofac Surg 23:e366–9
Fearon JA, Singh DJ, Beals SP, Yu JC (2007) The diagnosis and treatment of single-sutural synostoses: Are computed tomographic scans necessary? Plast Reconstr Surg 120:1327–31
Eley KA, Sheerin F, Taylor N, Watt-Smith SR, Golding SJ (2013) Identification of normal cranial sutures in infants on routine magnetic resonance imaging. J Craniofac Surg 24(1):317–20
Harshbarger R, Kelley P, Leake D, George T (2010) Low dose craniofacial CT/Rapid access MRI protocol in craniosynostosis patients: decreased radiation exposure and cost savings. Plast Reconstr Surg 126:4–5
Morton RP, Reynolds RM, Ramakrishna R, Levitt MR, Hopper RA, Lee A, Browd SR (2013) Low-dose head computed tomography in children: a single institutional experience in pediatric radiation risk reduction. J Neurosurg Pediatr 12:406–10
Eley KA, McIntyre A, Watt-Smith SR, Golding SJ (2012) “Black Bone” MRI: A partial flip angle technique for radiation reduction in craniofacial imaging. Br J Radiol 85:272–8
Eley KA, Watt-Smith SR, Golding SJ (2012) “Black bone” MRI: a potential alternative to CTwhen imaging the head and neck: report of eight clinical cases and review of the Oxford experience. Br J Radiol 85:1457–64
Eley KA, Watt-Smith SR, Golding SJ (2013) “Black Bone” MRI: a potential non-ionizing method for threedimensional cephalometric analysis--a preliminary feasibility study. Dentomaxillofac Radiol. 42(10):20130236
Vu HL, Panchal J, Parker EE, Levine NS, Francel P (2001) The timing of physiologic closure of the metopic suture: a review of 159 patients using reconstructed 3D CT scans of the craniofacial region. J Craniofac Surg 12:527–32
Tartaro A, Larici AR, Antonucci D, Merlino B, Colosimo C, Bonomo L (1998) Optimization and diagnostic accuracy of computerized tomography with tridimensional spiral technique in the study of craniosynostosis. Radiol Med 96:10–17
Acknowledgements
The authors would like to thank Dr. Russ Evans, Mr. Steven Wall, Mr. David Johnson, and Dr. Jo Byren, at the Oxford Craniofacial Unit, and the radiographers at the John Radcliffe Hospital, for their assistance with this study.
This study was presented at RSNA, Chicago, November 2013 & in part at ESHNR Leipzig, September 2012.
The scientific guarantor of this publication is KA Eley. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by AO Foundation (Project no. C-09-01W) & Newlife Foundation for Disabled Children. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. No study subjects or cohorts have been previously reported. Methodology: prospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eley, K.A., Watt-Smith, S.R., Sheerin, F. et al. “Black Bone” MRI: a potential alternative to CT with three-dimensional reconstruction of the craniofacial skeleton in the diagnosis of craniosynostosis. Eur Radiol 24, 2417–2426 (2014). https://doi.org/10.1007/s00330-014-3286-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3286-7