Abstract
Objectives
The potential diagnostic value of dual-energy computed tomography (DE-CT) compared to dynamic contrast-enhanced CT (DCE-CT) and conventional contrast-enhanced CT (CE-CT) in the assessment of early regorafenib treatment effects was evaluated in a preclinical setting.
Methods
A rat GS9L glioma model was examined with contrast-enhanced dynamic DE-CT measurements (80 kV/140 kV) for 4 min before and on days 1 and 4 after the start of daily regorafenib or placebo treatment. Tumour time-density curves (0-240 s, 80 kV), DE-CT (60 s) derived iodine maps and the DCE-CT (0-30 s, 80 kV) based parameters blood flow (BF), blood volume (BV) and permeability (PMB) were calculated and compared to conventional CE-CT (60 s, 80 kV).
Results
The regorafenib group showed a marked decrease in the tumour time-density curve, a significantly lower iodine concentration and a significantly lower PMB on day 1 and 4 compared to baseline, which was not observed for the placebo group. CE-CT showed a significant decrease in tumour density on day 4 but not on day 1. The DE-CT-derived iodine concentrations correlated with PMB and BV but not with BF.
Conclusions
DE-CT allows early treatment monitoring, which correlates with DCE-CT. Superior performance was observed compared to single-energy CE-CT.
Key Points
• Regorafenib treatment response was evaluated by CT in a rat tumour model.
• Dual-energy contrast-enhanced CT allows early treatment monitoring of targeted anti-tumour therapies.
• Dual-energy CT showed higher diagnostic potential than conventional contrast enhanced single-energy CT.
• Dual-energy CT showed diagnostic potential comparable to dynamic contrast-enhanced CT.
• Dual-energy CT is a promising method for efficient clinical treatment response evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in the field of novel anti-tumour drug therapies have resulted in an increasing need for diagnostic tests that allow early, accurate and objective evaluation of treatment responses. The classic method of measuring the diameter of solid tumours according to the Response Evaluation Criteria in Solid Tumors (RECIST) [1, 2] has recently been shown to have poor sensitivity in estimating tumour response to anti-angiogenic drugs or tyrosine kinase inhibitors [3–7] because these therapies primarily induce changes in the microvasculature of the tumour rather than a decrease in tumour size.
As an alternative, Choi et al. demonstrated that combined measurements of tumour attenuation and tumour size, using conventional portal-venous phase contrast-enhanced CT (CE-CT) during follow-up of metastatic gastrointestinal stromal tumours (GIST) undergoing targeted treatment, are significantly better predictors of treatment response than RECIST [5]. Decreased tumour attenuation correlates pathohistologically with the development of tumour necrosis and cystic or myxoid degeneration as a result of the therapy targeting anti-angiogenesis. However, in case of intratumoral haemorrhage during targeted treatment, the resulting increase in tumour attenuation may cause misleading treatment response evaluation based on the Choi criteria [8].
Dynamic contrast-enhanced computed tomography (DCE-CT) is used to characterise the tumour microvascularisation by monitoring the kinetics of contrast agent (CA) passage in the tumour. It has been shown to be a sensitive diagnostic tool for the assessment of early treatment response by detecting changes in vascularisation, tissue perfusion and vascular permeability [9–14]. This is especially relevant for anti-angiogenic treatments, as the inhibition of angiogenic signalling pathways is accompanied by a decrease in the elevated vascular tumour permeability [15]. Despite numerous advances in dose-saving imaging techniques [16, 17], the clinical use is still limited by relatively high radiation doses and complex image post-processing [18].
Contrast-enhanced dual-energy CT (DE-CT) allows selective detection and a fairly straightforward quantification of the iodine content in tumours [19] with comparable radiation doses to CE-CT at 120 kV [20–23]. Using DE-CT, an iodine map encoding the iodine content in each voxel and a virtual non-contrast image were calculated. As the amount of iodine-containing CA within a tissue varies with its vascularisation, perfusion and vascular permeability, vascular tissue properties can be directly deduced from the tumour iodine concentration. The DE-CT based quantification of the iodine content permits the differentiation of hypervascularised tissue from haemorrhage [24]. Hence, this method of tumour response evaluation is potentially more accurate than CE-CT or the Choi criteria.
The aim of this preclinical study was to systematically evaluate the diagnostic potential of DE-CT in direct comparison to DCE-CT and CE-CT in the monitoring of intraindividual early treatment response to regorafenib, a new oral multikinase inhibitor that has recently been approved by the US Food and Drug Administration (FDA) for the treatment of metastatic colorectal cancer [25]. Regorafenib inhibits both angiogenic kinases, such as VEGF receptors, which play an important role in tumour neoangiogenesis, and several oncogenic and stromal receptor tyrosine kinases [26].
Material and methods
Animals
Sixteen healthy Fischer rats (males; mean weight 300 g) were purchased from Charles River (Sulzfeld, Germany). The animals were kept under standard laboratory conditions at a temperature of 22 °C with standard food and water ad libitum. The animals were handled in compliance with German animal welfare legislation and with the approval of the state animal welfare committee. The animals were inoculated with 3 × 106 GS9L cells intramuscularly into the left foreleg.
Experimental setup
Eight days after inoculation of the tumour cells, the animals were randomly assigned to one of two groups: the regorafenib group (n = 8) or the placebo group (n = 8). Then DE-CT examinations were performed to obtain baseline (BL) levels. The CT imaging was repeated on day 1 and day 4 after the start of treatment. Oral treatment with either regorafenib (Stivarga, Bayer Pharma AG, Berlin, Germany) or placebo (vehicle without therapeutic agent [26] at a dose of 10 mg/kg body weight) was started immediately after the baseline CT. Daily treatment was continued for 3 days.
The rats were anesthetised with 4 % isoflurane (Baxter Deutschland GmbH, Unterschleißheim, Germany) for all CT examinations, and anaesthesia was maintained throughout the examination with 1.5 % isoflurane. CT images were acquired with the rats positioned prone and head first. A peripheral intravenous line (24 gauge) was inserted in the tail vein and connected to a dedicated small-animal injector. Two seconds after the start of the CT, iopromide (Ultravist 300, Bayer Vital GmbH, Leverkusen, Germany) at a dosage of 0.5 g iodine/kg body weight was injected into the tail vein with a flow rate of 0.8 ml/s followed by 0.9 ml saline administered at the same rate.
CT imaging protocol
The study was performed using a clinical second-generation dual-source scanner (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany). The measurement range was adjusted to cover the tumour in the left foreleg and the thoracic region. DE-CT was performed in sequential, dynamic mode without table feed using a detector collimation of 32 × 0.6 mm and a rotation time of 0.5 s. The settings were 80 kV, 100 mAs for tube A and 140 kV with tin filtration, 39 mAs for tube B. DE-CT was acquired over a total period of 4 min in two imaging blocks:
-
1st scan (0-30 s): 1 acquisition every second (n = 30 acquisitions);
-
2nd scan (35-240 s): 1 acquisition every 5 s (n = 42 acquisitions).
Images were reconstructed with a slice thickness and increment of 2 mm using a kernel of moderate softness in the abdominal window (kernel B31 or D30f for dual-energy analysis).
Post-processing and data analysis
The images were transferred to a workstation for post-processing (MMWP, Siemens Healthcare, Erlangen, Germany). The animals were numbered consecutively and group affiliations were blinded to the reader for evaluation.
Time-density curves
Data were analysed using the CT system software DynEva (Siemens Healthcare, Erlangen, Germany). The two 80-kV data sets acquired per animal at BL, day 1 and day 4 (kernel B31, 0-30 s and kernel B31, 35-240 s) were combined and stored as one series (80 kV, 0-240 s). In this new data set and within each rat, regions of interest (ROIs) were drawn manually to enclose the tumour, excluding bones, in three contiguous and representative slices at each of the three examinations. The resulting three curves per animal and measurement were averaged over the whole group of eight animals. In the regorafenib-treated animals, the difference among the three examinations (BL, day 1, day 4) reached a maximum around 60 s after CA injection. Therefore, this time point was chosen for CE-CT and DE-CT image analysis.
DCE-CT
The DCE-CT image analysis was performed using the 80-kV data set from the first DE-CT scan block (0-30 s) and the body perfusion software (VPCT Body, Siemens Healthcare, Erlangen, Germany). The software based on a two-compartment pharmacokinetic model and the voxel time-density curves were fitted by using a deconvolution technique [27]. After automatic motion correction and bone segmentation, the arterial input function was derived from a manually defined ROI in the descending aorta at the mid-level of the heart. The time shift in the CA arrival between the aorta and tumour tissue was set automatically. Functional parameter maps were calculated for the permeability (PMB), blood volume (BV) and blood flow (BF). For the three examinations (BL, day 1, day 4), manual ROIs were drawn around the tumours, excluding bones, in three contiguous and representative slices, corresponding to the slices used in the preceding analysis. Quantitative parameters were calculated for PMB, BV and BF on the basis of the ROIs.
CE-CT
Tumour densities of the CE-CT examinations were measured using the images at 60 s post injection (p.i.) in the same manner as for the preceding analyses by drawing ROIs around the tumour in three contiguous slices of the CE-CT examinations at 80 kV (kernel B31). The relative change in tumour attenuation compared to BL was calculated for day 1 and day 4.
DE-CT
The DE-CT image evaluation was performed using the 80 kV and 140 kV (kernel D30f) data at 60 s p.i. For the analysis, Dual Energy software (Siemens Healthcare, Erlangen, Germany) was used to decompose the images into a pure iodine image and a virtual non-contrast image (VNC) based on the specific absorption characteristics of iodine at 80 kV and 140 kV. The dual-energy analysis was adjusted to the animal model used by applying modified liver VNC parameters (Table 1). As described above, manual ROIs were drawn around the tumour in three representative and contiguous slices within the iodine maps at BL, day 1 and day 4 and the respective iodine concentrations were calculated.
Statistical evaluation
All values are presented as mean ± standard deviation. A statistical comparison within the groups (BL vs. day 1 and day 4) was performed using a one-way repeated-measures analysis of variance test followed by Tukey post-hoc comparison. The comparison among groups for BL, day 1 and day 4 was performed with the one-way analysis of variance test followed by Tukey post-hoc comparison. The calculations were performed with GraphPad Prism (GraphPad Software, La Jolla, CA, USA) using a significance level of 5 %.
Results
All except one CT examination of the 16 rats measured at BL, day 1 and day 4 were technically successful. The unsuccessful examination was due to failure of the CA injection in rat no. 3 (regorafenib group) on day 1. The time point was excluded from analysis for this animal.
Time-density curves
The tumour time-attenuation curves after treatment with regorafenib (day 1 and day 4) showed clearly reduced tumour signal levels compared with the BL curve. In contrast, only minor changes were detected over time in the placebo group (Fig. 1). Thus, the treatment effects of regorafenib can be detected as early as 24 h after the first dose. The signal decrease after treatment was most prominent during the interstitial phase about 40-80 s after injection of the CA (Fig. 1).
Time-attenuation curves of the regorafenib and placebo groups (group mean value ± SD within group) at baseline, day 1 and day 4 showing a marked change in the progression of the curves on day 1 and day 4 after regorafenib treatment. The signal decrease was most prominent about 40-80 s after injection of the contrast agent
DCE-CT
A more detailed and quantitative analysis of the tumour microvasculature was obtained by DCE-CT in combination with pharmacokinetic modelling. The parameters PMB, BV and BF of the tumour were quantified based on the calculated functional parameter maps. A representative example of the three colour-coded maps demonstrating the effect of regorafenib treatment is shown in Fig. 2. A marked decrease in PMB on days 1 and 4 compared with baseline is readily apparent. The quantitative analysis of the regorafenib-treated animals yields a statistically significant decrease in PMB on day 1 (17.38 ± 5.34 ml/100 ml/min) and day 4 (11.73 ± 2.29 ml/100 ml/min) compared to BL (23.37 ± 5.34 ml/100 ml/min) (Fig. 3, Table 2). The differences between days 1 and 4 were also significant. In contrast, in the placebo group no significant changes in PMB were observed between day 1 (24.50 ± 5.55 ml/100 ml/min) and day 4 (22.26 ± 5.44 ml/100 ml/min) compared to BL (22.52 ± 5.52 ml/100 ml/min) (Fig. 3). However, PMB on day 4 was significantly lower than on day 1. The BV and BF did not change significantly over time compared to BL in the regorafenib group. However, in the placebo group a significantly lower BF was observed on day 4 compared to day 1.
Functional parameter maps of DCE-CT images at baseline (left), day 1 (middle) and day 4 (right) after treatment with regorafenib, showing a marked decrease in the tumour PMB (images top right) on day 1 and day 4 compared to baseline. In contrast, no clear changes in tumour BF (images bottom left) or BV (images bottom right) are apparent. The thin white line demarcates the respective ROI
Quantitative analysis of DCE-CT-derived parameters PMB (left), BV (middle) and BF (right) in the regorafenib and placebo group at baseline, day 1 and day 4. There is a significant decrease in PMB between each of the 3 days in the regorafenib group. In contrast, no significant changes in PMB can be observed in the placebo group between day 1 and day 4 compared to baseline. No significant changes over time were observed for BV. The BF also showed no significant changes, with the exception of a reduction in BF between day 4 and day 1 in the placebo group. Statistically significant differences between different time points are marked with an asterisk (*p < 0.05; **p < 0.01)
Statistical comparison between the groups at the three time points (BL, day 1 and day 4) yields significantly lower PMB on day 1 and day 4 for the regorafenib group compared to the placebo group. No differences between the two treatment groups were observed for BV and BF at any time point.
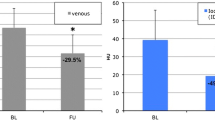
CE-CT
The image analysis based on the 80 kV CE-CT at 60 s p.i. showed tumour attenuations of 97.90 ± 10.16 HU (BL), 89.12 ± 6.54 HU (day 1) and 81.18 ± 7.15 HU (day 4) for the animals treated with regorafenib (Fig. 4). The decrease from BL to day 4 was statistically significant, whereas the attenuation on day 1 showed no difference from BL. In the placebo group no significant decrease was observed between BL (99.43 ± 8.07 HU), day 1 (97.96 ± 9.03 HU) and day 4 (94.98 ± 9.65 HU). The analysis among the groups showed significantly lower tumour attenuations on day 4 but not on BL or day 1.
CE-CT-derived tumour attenuation values show a significant decrease in the regorafenib group from baseline to day 4, whereas no significant decrease can be seen on day 1 compared to baseline. In the placebo group no significant decrease can be observed on either day. Statistically significant differences between different time points are marked with an asterisk (*p < 0.05; **p < 0.01)
In order to compare the tumour response over time using the Choi criteria, the relative change in tumour attenuation was determined for day 1 and day 4. In the regorafenib group, two animals on day 1 and five animals on day 4 showed an HU reduction greater than 15 %. Only one animal in the placebo group showed a change in attenuation greater than 15 % on day 4.
DE-CT
Figure 5 shows an example of DE-CT iodine maps at BL, day 1 and day 4 for a rat from the regorafenib group, showing a clear decrease in iodine concentrations over time. The DE-based quantification of the tumour iodine concentration after regorafenib treatment showed a significant decrease in iodine concentration from BL (1.57 ± 0.27 mg/ml) to day 1 (1.32 ± 0.21 mg/ml) and from BL to day 4 (1.15 ± 0.13 mg/ml). In contrast, no significant changes were observed in the placebo group, with iodine concentrations of 1.64 ± 0.21 mg/ml, 1.54 ± 0.26 mg/ml and 1.61 ± 0.25 mg/ml for BL, day 1 and day 4, respectively. The between-group comparison showed a significantly lower tumour iodine concentration for the regorafenib-treated animals on day 4 but not on day 1 (Fig. 6).
Quantitative DE-CT analysis of iodine concentrations at baseline, day 1 and day 4 in the regorafenib and placebo groups. There is a significant decrease in iodine concentrations after regorafenib treatment from baseline to day 1 and from baseline to day 4. In contrast, no significant changes can be observed in the placebo group. Statistically significant differences between different time points are marked with an asterisk (*p < 0.05; **p < 0.01)
Correlation of DE-CT with CE-CT and DCE-CT
The correlation between all DE-CT-derived tumour iodine concentrations to the DCE-CT-based parameters PMB, BV and BV, which characterise the tumour microvasculature, were analysed (Fig. 7). The iodine concentration showed a significant, moderate positive correlation with the PMB (r2 = 0.61) and BV (r2 = 0.52). No significant correlation was found for BF (r2 = 0.13). Comparison with CE-CT showed a high correlation (r2 = 0.80) between iodine concentration and tumour attenuation. Hence, decreasing iodine concentrations during treatment were associated with decreasing PMB, BV and CE-CT signal intensities.
Correlation analysis of DE-CT-derived tumour iodine concentrations with DCE-CT-based parameters PMB, BV and BF and CE-CT attenuation values shows a correlation between the tumour iodine concentration and PMB (top left), BV (top right) and CE-CT attenuation values (bottom right), whereas no correlation was found with BF (bottom left); r 2 represents the correlation coefficient. Statistically significant correlations are marked with an asterisk (*p < 0.05; **p < 0.01)
Discussion
Study design
In this preclinical study, we compared DE-CT with conventional CE-CT and DCE-CT in the monitoring of early response to targeted antitumour treatment in an experimental rat glioblastoma tumour model. Dynamic DE-CT imaging was performed for each animal before and on days 1 and 4 after treatment with regorafenib or placebo. DCE-CT (80 kV, 0-30s p.i.) parameter analysis (PMB, BV, BF), CE-CT (80 kV, 60s p.i.) image evaluation and a DE-CT (80/140 kV, 60s p.i.) derived analysis of tumour iodine concentrations were performed. In contrast to clinical studies, it was thus possible to compare all three methods under identical experimental conditions in the same animal on the basis of simultaneously acquired images. This way neither morphological tumour changes nor physiological changes affecting the kinetics of the CA, such as cardiac output, nor technical variations, such as slice position, biased the comparison of the three different methods. The differences observed are therefore solely due to the method of image evaluation and post-processing.
Comparison of methods
All three procedures detected therapeutic effects of regorafenib after the 4-day observation period. Moreover, for the parameters PMB (Fig. 3) and tumour iodine concentration (Fig. 6), intraindividual treatment effects were detected as early as 24 h after initiation of regorafenib treatment. No effects were observed at this time point when tumours were analysed by CE-CT (Fig. 4).
Choi et al. defined partial response to targeted therapy with portal-venous phase CE-CT as a decrease in tumour attenuation greater than 15 % from pre- to post-treatment CT or a decrease in tumour diameter greater than 10 % [4, 5]. According to those criteria, only two out of eight animals (day 1) and five out of eight animals (day 4) from the therapy group were classified as partial responders because of their decrease in attenuation. We therefore conclude that in the present study, CE-CT and the Choi criteria are not as sensitive as the PMB and the tumour iodine concentration in monitoring early individual response to regorafenib.
Tumour attenuation and iodine concentration are determined by the accumulation of CA in the tumour. Consequently, both parameters correlate well in direct comparison (Fig. 7). However, CE-CT shows not only the accumulation of iodine but also the constitution of the tumour tissue (e.g. vital tumour, necrosis, haemorrhage), which is assumed to change in response to therapy. In contrast, DE-CT-derived tumour iodine concentrations are determined solely by therapy-induced changes in CA accumulation. Therefore DE-CT possesses a higher intrinsic sensitivity.
However, both DE-CT and CE-CT depend on the accumulation of CA at one time point 60 s after the CA has been injected and represent only a “snapshot” of CA kinetics. In contrast, DCE-CT has the method-related advantage of sampling CA kinetics dynamically. DCE-CT quantification with the two-compartment model results in significantly reduced PMB, not only in the intraindividual follow-up but also in the group-wise comparison of placebo- and regorafenib-treated animals. Here, statistically significant differences were observed on day 1 and day 4, while tumour attenuation and tumour iodine concentration showed a significant difference between the therapy and placebo group only on day 4. Considering the high treatment efficacy of regorafenib that has been shown in clinical [25] and preclinical studies [26], we conclude that DCE-CT is the most sensitive of the three methods investigated.
On the other hand, significant changes in PMB were also observed within the placebo group (day 4 vs. day 1). In contrast to the regorafenib-treated animals, PMB transiently increased on day 1 before decreasing on day 4 back to baseline level. This increase, although not statistically significant, was also observed for BV and BF. As these effects were not observed in the therapy group they can most likely be attributed to changes in the tumour tissue constitution within the analysed central slices of the tumours. This observation also demonstrates the limitations and potential pitfalls of this method when comparing different time points.
In the present study PMB was the most sensitive marker for early regorafenib response. This is in agreement with a previous preclinical DCE-CT study in the same animal model comparing two contrast agents with different pharmacokinetics [28] and the results of a dynamic macromolecular-enhanced MRI study [26]. In a recently published study, investigating a rat colon cancer model with DCE-CT, a significantly reduced tumour vascularity was observed after daily treatment with regorafenib over 7 days [14]. Although the averaged PMB was reduced by about 50 %, no significant changes were observed as the reduction was inconsistent within the group. Possible reasons for these different findings might be the longer therapy cycle, the different tumour model or the method of image analysis. In contrast to our study, they analysed only the viable tumour tissue and used a different two-compartment uptake model. These differences in data post-processing underline the importance of standardisation in the evaluation of DCE-CT data to make results comparable.
In contrast, DE-CT-derived tumour iodine quantification does not depend on a specific vascular parameter. In our study we observed a correlation between tumour iodine concentration, PMB and BV, but not with BF (Fig. 7). This demonstrates that DE-CT tumour iodine quantification can detect early treatment-related changes in vessel permeability and shows the potential of DE-CT in the evaluation of early therapy effects.
The results of the present animal study confirm pervious clinical observations comparing CE-CT/Choi criteria and DE-CT-based iodine attenuation or quantification. A study in metastatic GIST patients found a good correlation between portal-venous CT density values and tumour iodine-related attenuation [29]. The authors conclude that DE-CT-based iodine quantification is a more robust parameter for the evaluation of treatment response. This was also the conclusion of a study in HCC patients treated with sorafenib [30]. They introduced the parameter of “volumetric iodine uptake” to quantify the iodine uptake of the entire tumour. This might be a promising approach that takes the tumour volume into account.
Limitations
Imaging protocols for DCE-CT and CE-CT differ from clinical protocols because of the chosen study design and the small animal model: The setup was designed to evaluate regorafenib treatment effects systematically. Therefore CA kinetics in the tumour tissue was monitored over a relatively long examination duration of 4 min.
The high temporal resolution of DCE-CT was chosen to ensure a high sampling rate for the two-compartment modelling, not taking into account radiation dose issues. In contrast to the criteria suggested by Choi et al. [5], the evaluation of CE-CT was performed at 80 kV instead of 120 kV because of the small animal model and as iodine attenuation is higher at lower tube voltages. Hence, no meaningful conclusions can be drawn regarding radiation doses as each CT examination technique was specifically adapted to this study and differs from clinical applications.
However, previous studies specifically focusing on this issue reported that DE-CT is feasible with similar radiation doses and image noise and similar or even better contrast-to-noise ratios when compared to single-phase 120-kV CE-CT [20–22]. The 72 dynamic images for each CT examination result in a dose length product of 514 mGy*cm. Although this considerable radiation dose is significantly below the doses used in radiation therapy, this might have influenced our results, especially the comparison between regorafenib and placebo treatment. Moreover, the method of image evaluation had some limitations. We determined the time point p.i. for the CE-CT and DE-CT measurements on the basis of the time-density curves before and after treatment with regorafenib. This is in contrast to clinical settings, where imaging is usually performed during portal-venous phase. The image analysis was based on manually drawn ROIs, which were defined separately for each of the three methods and investigated time points. Although we used standardised criteria for ROI definition, this may have biased our results. Furthermore, in our study, therapy-related changes in the tumour microvasculature were observed during a relatively short period of 4 days and potential changes in tumour size have not been considered.
Conclusion
In conclusion, tumour iodine concentration measurements by DE-CT can be a useful marker to assess early regorafenib treatment effects. The results of this preclinical study provide a basis for interpreting clinical observations and may help to optimise early treatment monitoring.
References
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247
Motzer RJ, Hutson TE, Tomczak P et al (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356(2):115–124
Benjamin RS, Choi H, Macapinlac HA et al (2007) We should desist using RECIST, at least in GIST. J Clin Oncol : Off J Am Soc Clin Oncol 25(13):1760–1764
Choi H, Charnsangavej C, Faria SC et al (2007) Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol : Off J Am Soc Clin Oncol 25(13):1753–1759
Ratain MJ, Eisen T, Stadler WM et al (2006) Phase II placebo-controlled randomized discontinuation trial of sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol Off J Am Soc Clin Oncol 24(16):2505–2512
Faivre S, Delbaldo C, Vera K et al (2006) Safety, pharmacokinetic, and antitumor activity of SU11248, a novel oral multitarget tyrosine kinase inhibitor, in patients with cancer. J Clin Oncol Off J Am Soc Clin Oncol 24(1):25–35
Choi H (2005) Critical issues in response evaluation on computed tomography: lessons from the gastrointestinal stromal tumor model. Curr Oncol Rep 7(4):307–311
Goh V, Halligan S, Daley F, Wellsted DM, Guenther T, Bartram CI (2008) Colorectal tumor vascularity: quantitative assessment with multidetector CT–do tumor perfusion measurements reflect angiogenesis? Radiology 249(2):510–517
d’Assignies G, Couvelard A, Bahrami S et al (2009) Pancreatic endocrine tumors: tumor blood flow assessed with perfusion CT reflects angiogenesis and correlates with prognostic factors. Radiology 250(2):407–416
Kan ZX, Phongkitkarun S, Kobayashi S et al (2005) Functional CT for quantifying tumor perfusion in antiangiogenic therapy in a rat model. Radiology 237(1):151–158
Lee TY, Purdie TG, Stewart E (2003) CT imaging of angiogenesis. Q J Nucl Med 47(3):171–187
Lind JS, Meijerink MR, Dingemans AM et al (2010) Dynamic contrast-enhanced CT in patients treated with sorafenib and erlotinib for non-small cell lung cancer: a new method of monitoring treatment? Eur Radiol 20(12):2890–2898
Cyran CC, Kazmierczak PM, Hirner H et al (2013) Regorafenib effects on human colon carcinoma xenografts monitored by dynamic contrast-enhanced computed tomography with immunohistochemical validation. PLoS ONE 8(9):e76009
Yuan F, Chen Y, Dellian M, Safabakhsh N, Ferrara N, Jain RK (1996) Time-dependent vascular regression and permeability changes in established human tumor xenografts induced by an anti-vascular endothelial growth factor/vascular permeability factor antibody. Proc Natl Acad Sci U S A 93(25):14765–14770
Winklehner A, Goetti R, Baumueller S et al (2011) Automated attenuation-based tube potential selection for thoracoabdominal computed tomography angiography: improved dose effectiveness. Invest Radiol 46(12):767–773
Pontana F, Duhamel A, Pagniez J et al (2011) Chest computed tomography using iterative reconstruction vs filtered back projection (Part 2): image quality of low-dose CT examinations in 80 patients. Eur Radiol 21(3):636–643
Brix G, Griebel J, Kiessling F, Wenz F (2010) Tracer kinetic modelling of tumour angiogenesis based on dynamic contrast-enhanced CT and MRI measurements. Eur J Nucl Med Mol Imaging 37(Suppl 1):S30–S51
Johnson TRC, Krauss B, Sedlmair M et al (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17(6):1510–1517
Henzler T, Fink C, Schoenberg SO, Schoepf UJ (2012) Dual-Energy CT: Radiation Dose Aspects. Am J Roentgenol 199(5):S16–S25
Schenzle JC, Sommer WH, Neumaier K et al (2010) Dual Energy CT of the Chest: How About the Dose? Invest Radiol 45(6):347–353
Kerl JM, Bauer R, Maurer T et al (2011) Dose levels at coronary CT angiography—a comparison of dual energy-, dual source- and 16-slice CT. Eur Radiol 21(3):530–537
Zordo T, Lutterotti K, Dejaco C et al (2012) Comparison of image quality and radiation dose of different pulmonary CTA protocols on a 128-slice CT: high-pitch dual source CT, dual energy CT and conventional spiral CT. Eur Radiol 22(2):279–286
Simons D, Kachelriess M, Schlemmer HP (2014) Recent developments of dual-energy CT in oncology. Eur Radiol 24(4):930–939
Eisen T, Joensuu H, Nathan PD et al (2012) Regorafenib for patients with previously untreated metastatic or unresectable renal-cell carcinoma: a single-group phase 2 trial. Lancet Oncol 13(10):1055–1062
Wilhelm SM, Dumas J, Adnane L et al (2011) Regorafenib (BAY 73-4506): a new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int J Cancer 129(1):245–255
Mahnken AH, Klotz E, Pietsch H et al (2010) Quantitative whole heart stress perfusion CT imaging as noninvasive assessment of hemodynamics in coronary artery stenosis: preliminary animal experience. Invest Radiol 45(6):298–305
Jost G, Pietsch H, Grenacher L (2013) Dynamic contrast-enhanced computed tomography to assess antitumor treatment effects: comparison of two contrast agents with different pharmacokinetics. Invest Radiol 48(10):715–721
Apfaltrer P, Meyer M, Meier C et al (2012) Contrast-enhanced dual-energy CT of gastrointestinal stromal tumors: is iodine-related attenuation a potential indicator of tumor response? Invest Radiol 47(1):65–70
Dai X, Schlemmer HP, Schmidt B et al (2013) Quantitative therapy response assessment by volumetric iodine-uptake measurement: initial experience in patients with advanced hepatocellular carcinoma treated with sorafenib. Eur J Radiol 82(2):327–334
Acknowledgements
The scientific guarantors of this publication are Gesine Knobloch and Gregor Jost, and both contributed equally to this study. The authors of this manuscript declare relationships with the following companies: Jost and Pietsch (Employee Bayer AG) and Huppertz (Employee Siemens AG).
The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Approval from the institutional animal care committee was obtained. Methodology: prospective, randomised controlled trial, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knobloch, G., Jost, G., Huppertz, A. et al. Dual-energy computed tomography for the assessment of early treatment effects of regorafenib in a preclinical tumor model: comparison with dynamic contrast-enhanced CT and conventional contrast-enhanced single-energy CT. Eur Radiol 24, 1896–1905 (2014). https://doi.org/10.1007/s00330-014-3193-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3193-y