Abstract
Objectives
To evaluate the usefulness of diffusion-weighted (DW) magnetic resonance images for distinguishing non-neoplastic cysts from solid masses of indeterminate internal characteristics on computed tomography (CT) in the mediastinum.
Methods
We enrolled 25 patients with pathologically proved mediastinal masses who underwent both thoracic CT and magnetic resonance imaging (MRI) including diffusion-weighted imaging (DWI). MRI was performed in patients with mediastinal masses of indeterminate internal characteristics on CT. Two thoracic radiologists evaluated the morphological features and quantitatively measured the net enhancement of the masses at CT. They also reviewed MR images including unenhanced T1- and T2-weighted images, gadolinium-enhanced images and DW images.
Results
The enrolled patients had 15 solid masses and ten non-neoplastic cysts. Although the morphological features and the extent of enhancement on CT did not differ significantly between solid and cystic masses in the mediastinum (P > 0.05), non-neoplastic cysts were distinguishable from solid masses by showing signal suppression on high-b-value DW images or high apparent diffusion coefficient (ADC) values of more than 2.5 × 10-3 mm2/s (P < 0.001). ADC values of non-neoplastic cysts (3.67 ± 0.87 × 10-3 mm2/s) were significantly higher than that of solid masses (1.46 ± 0.50 × 10-3 mm2/s) (P < 0.001).
Conclusions
DWI can help differentiate solid and cystic masses in the mediastinum, even when CT findings are questionable.
Key Points
• Non-invasive diagnosis of non-neoplastic cysts can save surgical biopsy or excision.
• Conventional CT or MRI findings cannot always provide a confident diagnosis.
• Mediastinal masses can be well-characterised with DWI.
• Non-neoplastic mediastinal cysts show significantly higher ADC values than cystic tumours.
• DWI is useful to determine treatment strategy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mediastinal masses comprise a heterogeneous group of lesions ranging from non-neoplastic cysts to malignant solid masses. Masses with a solid component include thymic epithelial tumour, lymphoma or germ cell tumour, which necessitate pathological confirmation through biopsy or surgery. On the other hand, non-neoplastic mediastinal cysts, such as bronchogenic or pericardial cysts, are considered benign lesions, and surgery is reserved only for complications such as haemorrhage or infection, if pre-surgical diagnostic measures can confirm its cystic nature [1]. The internal characteristics of solid or cystic nature and the location of the mass can help to make a differential diagnosis of the mass in the mediastinum [2]. Therefore, both the anatomical information and internal characteristics are essential in determining therapeutic options.
Contrast-enhanced computed tomography (CT) has been the most commonly used imaging modality for the evaluation of mediastinal masses. The presence of significant enhancement on CT images was considered indicative of a solid internal nature of mediastinal tumours. However, solid masses may sometimes show no visible enhancement after the injection of contrast media and even cystic masses can show high attenuation on unenhanced CT images due to internal haemorrhage or infection, mimicking solid tumours [3, 4]. Therefore, CT may be limited in differentiating some solid or cystic masses in the mediastinum [3–5]. We focused on the evaluation of a non-invasive diagnostic method for the further characterisation of masses with complex appearance and density on CT in this study. This may help to guide treatment options of surgical biopsy versus observation.
With on-going technical improvements, magnetic resonance imaging (MRI) is useful for chest imaging in clinical practice. Conventional MR images can provide detailed anatomic information about the location, margin and contour of mediastinal mass. Diffusion-weighted MRI (DWI) can also characterise internal cellular density and mobility of water [6]. The degree of water diffusion is more restricted in tissues with higher cellular density because of numerous intact cell membranes [7–9]. Although DWI in chest imaging has been technically challenging, as the images are sensitive to motion from cardiac pulsation and respiration [10], recent advances in MR systems with stronger field gradients, parallel imaging technique, multichannel coil and echo-planar MRI [10–12] broadened its application for the lung and mediastinal lesions.
The purpose of this work was to evaluate the usefulness of DWI for the differentiation of mediastinal solid masses and non-neoplastic cysts which were indeterminate internal characteristics on CT.
Material and methods
The Institutional Review Board approved this retrospective study with a waiver of informed consent. (IRB file number 2012-07-035).
Patients
Between 2009 and 2011, 274 patients with a mediastinal mass were identified on CT by review of the medical records at our institution. This study included 61 consecutive patients who underwent both thoracic CT and MRI including DWI. DWI was usually recommended for further characterisation of mediastinal masses of indeterminate internal characteristics on CT in clinical practice. Excluding 36 patients where histology was not available, imaging findings were analysed in 25 patients (9 men, 16 women; mean age, 49 ± 14 years). The mediastinal masses were pathologically confirmed by surgical excision (n = 23) or percutaneous biopsy (n = 2). The 36 patients lacking pathological diagnosis were followed only after being considered to have non-neoplastic cysts on DWI (n = 27) or could not undergo surgery due to refusal of an operation (n = 5) or combined other malignancy (n = 2) or lost to follow-up (n = 2).
Image acquisition
Chest CT and MRI were performed within a 1-month period (average time interval, 14 days). Chest CT was obtained with the helical technique by using multidetector CT (LightSpeed Qxi, Light speed Ultra, or LightSpeed 16, LightSpeed VCT; GE Healthcare; Waukesha, WI, USA). Unenhanced CT images were obtained with the following parameters: 120 kVp; automated milliampere selection (range, 50-200 mAs) at fixed noise index of 15.86 HU; section thickness, 2.5 mm for transverse images. Thereafter, enhanced CT images were obtained 40 s after initiation of contrast medium injection (3 ml/s, total of 100 ml iomeprol, Iomeron 300; Bracco, Milan, Italy) with a power injector (OP 100; Medrad, Warrendale, PA, USA) with the same parameters used for the unenhanced series.
All MRI studies were performed with a 3.0 T unit (Achieva; Philips Medical Systems, Best, The Netherlands) and obtained unenhanced and enhanced T1-weighted images, T2-weighted images and DWI. The MR imaging parameters were described in Table 1. The DW images were obtained at b values of 0, 100 and 900 s/mm2. The apparent diffusion coefficient (ADC) map was calculated by the MR system with a linear regression analysis of the natural log of the signal intensity with all three b values (0, 100 and 900 s/mm2). Enhanced T1-weighted images were obtained after intravenous injection of contrast media at a dose of 0.2 mM/kg paramagnetic contrast agent (DotaremR; Guerbet, Charles de Gaulle Cedex, France).
Image evaluation
Two chest radiologists (C.A.Y. and K.E.S, with 10 and 2 years of experience in thoracic image interpretation, respectively) reviewed the CT and MR images in consensus, blinded to the clinical and pathological results. MR evaluation was performed at least three months apart from CT evaluation to minimise recall bias.
On the analysis of CT images, mediastinal masses were reviewed for size, location (anterior, middle, posterior mediastinum), and morphological features. The morphological features were documented for shape (round, oval, elongated) and margin (sharp, ill-defined) of the mass. Net enhancement was quantitatively measured by placing the region of interest (ROI).
MR analysis was performed qualitatively by means of visual assessment and quantitatively by means of ADC measurements. T1- and T2-weighted MR images were evaluated for the signal intensity of each mass in comparison with that of cerebrospinal fluid (CSF) in the same image. The presence of enhancement within the mass was visually assessed by comparing unenhanced and enhanced T1-weighted MR images. DW images were visually evaluated for the presence of signal intensity suppression by reviewing low- and high-b-value (b = 0, 900 s/mm2) DW images and their corresponding ADC maps. Non-neoplastic cysts were considered when they show signal intensity suppression at a b value of 900 and corresponding high ADC values on ADC maps. Then they were quantitatively measured of its ADC values by placing a ROI within the mass. The average of two measurements of both reviewers was recorded as the final ADC value. With the use of ADC value, the mediastinal masses satisfying ADC values of more than 2.5 × 10-3 mm2/s were considered non-neoplastic cysts, and the others were considered masses with solid components.
Taking just the conventional MR findings on T1 and T2-weighted images and enhanced T1-weighted images into account, solid masses were considered to be present if lesions showed heterogeneous or homogeneous enhancement within the mass while non-neoplastic cysts were considered when lesions showed signal intensities (SIs) equal to or less than CSF on T1-weighted images, and SIs equal to or greater than CSF on T2-weighted images, and showed no enhancement or only rim-enhancement. However, using information from DW images and the ADC map, solid masses were considered to be present if lesions showed persistently high signal intensity at both low- and high-b-value images (0 and 900 s/mm2) and ADC value of less than 2.5 × 10-3 mm2/s, while non-neoplastic cysts were considered when lesions showed high and low signal intensity at low- and high-b-value images and ADC value of greater than 2.5 × 10-3 mm2/s. A confident diagnosis was only made when the above conventional MRI or DWI criteria were satisfied. Diagnostic accuracies for the correct decision on solid or cystic nature of mediastinal masses were compared when using conventional MRI and when using DWI.
Statistical analysis
Mann-Whitney test was used to analyse the differences of quantitative parameters between solid and cystic masses. The morphological differences between solid and cystic masses on CT and MR images were tested by the Fisher’s exact test. Diagnostic accuracies of conventional MR and DWI were compared with the McNemar test. Significance was accepted at P < 0.05 for all tests. All statistical analyses were performed with statistical software (SPSS, version 20.0 for Windows; SPSS, Chicago, IL, USA).
Results
Histopathology
Mediastinal masses were pathologically confirmed as non-neoplastic cysts in ten patients and as solid masses in 15 patients. The pathological subtypes of the mediastinal masses were summarised in Table 2.
CT features of mediastinal masses
The CT features of mediastinal masses are summarised in Table 3. The mean diameter of solid masses is longer than that of non-neoplastic cysts, but the difference is not statistically significant (P = 0.157). Morphological features of solid and non-neoplastic cysts do not differ significantly by CT findings such as size, location, shape and margins (P > 0.05). The Hounsfield units (HU) of masses were not significantly different on unenhanced and enhanced CT. Net enhancement of solid masses is higher than that of non-neoplastic cystic masses, but the difference is not statistically significant (P = 0.089).
MR features for tissue characterisation
The MR features of mediastinal masses are summarised in Table 4. Nine out of ten non-neoplastic mediastinal cysts (90 %) showed higher signal intensity than that of CSF on T1-weighted images and seven out of 15 solid masses (47 %) have higher signal intensity than the CSF on T2-weighted images. The signal intensity did not differ significantly between solid masses and non-neoplastic mediastinal cysts in comparisons with those of CSF on T1- and T2-weighted images (P > 0.05). Although no non-neoplastic cysts showed any enhancement after intravenous injection of contrast media, ten out of 15 solid masses (67 %) also did not show visible enhancement, failing to confirm the solid nature of the masses. Among the ten non-enhancing solid masses, four solid masses showed only rim enhancement mimicking the thin wall of cystic lesions. These lesions were confirmed as teratoma, extralobar pulmonary sequestration, schwannoma and thymic carcinoma. The presence or absence of enhancement at T1-weighted images were not significantly different between solid masses and non-neoplastic cysts (P = 0.061).
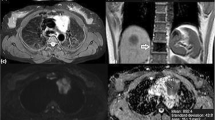
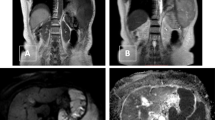
Most non-neoplastic mediastinal cysts (90 %) showed signal suppression on DW images at a high b value of 900 s/mm2. One non-neoplastic mediastinal cyst showed persistent high signal intensity on high-b-value DWI, but of which the ADC value was more than 2.5 × 10-3 mm2/s, representing a cystic internal nature (Fig. 1). Twelve (80 %) out of 15 solid masses show no or slight signal decrease on high-b-value DWIs. The presence of signal suppression on high-b-value DW images was significantly different between solid masses and non-neoplastic cysts (P = 0.001). ADC values of non-neoplastic cysts were significantly higher than those of solid masses (Table 5). The mean ADC value of non-neoplastic cysts is greater than that of solid masses in the mediastinum (3.67 ± 0.87 × 10-3 mm2/s vs 1.46 ± 0.50 × 10-3 mm2/s; P = 0.000). The range of ADC values for solid masses and non-neoplastic cysts did not overlap with each other (Fig. 2). Using a cut-off ADC value of 2.5 × 10-3 mm2/s, all non-neoplastic mediastinal cysts had ADC values more than 2.5 × 10-3 mm2/s and all solid masses had lower ADC value of less than 2.5 × 10-3 mm2/s (P < 0.001). The mean ADC value of malignant solid masses (n = 3) (Fig. 3) was lower than that of benign solid masses (n = 12) (Fig. 4), but not significantly lower (1.21 ± 0.34 × 10-3 mm2/s vs 1.53 ± 0.48 × 10-3 mm2/s, respectively; P = 0.386) (Table 5).
Bronchogenic cyst in a 54-year-old woman. a Unenhanced CT shows a well-defined oval mass (arrowheads) in the posterior mediastinum. The attenuation of the mass measured more than 50 HU, higher than that of water. b The corresponding enhanced CT does not show significant enhancement within the mass, but the cystic nature remains uncertain on CT. c Axial diffusion weighted MR images obtained with b values of 0 and 900 s/mm2 and ADC map. Although the mass (arrowheads) remains hyperintense at high-b-value DWI, the corresponding ADC map demonstrated high ADC value 2.93 × 10 -3 mm2/s (more than 2.5 × 10 -3 mm2/s), suggesting a cystic nature of the mass. The mass was pathologically confirmed as a bronchogenic cyst
Synovial sarcoma in a 38-year-old man. a Unenhanced chest CT shows a well-defined low-attenuated mass (arrows) in the right posterior mediastinum. b The corresponding enhanced CT shows no obvious enhancement of more than 20 HU. CT features of attenuation or enhancement of the mass do not fully support that it is solid in nature. c Axial DWIs obtained with b values of 0 and 900 s/mm2, and ADC map. Although the mass (arrowheads) shows heterogeneous signal suppression at b-value 900 DWI, the corresponding ADC value was 1.59 × 10-3 mm2/s, suggesting a solid nature of the mass. The mass was pathologically confirmed as a synovial sarcoma from the pleura
Mature cystic teratoma in a 52-year-old woman. a Unenhanced chest CT shows a homogeneous oval mass (arrowheads) in the anterior mediastinum with the attenuation value of 40 HU, which is higher than that of water. b The corresponding enhanced CT shows only rim enhancement of the wall suggesting cystic nature of the mass. c Axial diffusion weighted images obtained with b values of 0 and 900 s/mm2, and ADC map. The mass (arrows) shows large area of hyperintensity suggesting diffusion restriction at b-value 900 DWI. The corresponding ADC value is 1.58 × 10 -3 mm2/s, suggesting a “sticky” or viscous nature of the keratinoid substance in the teratoma
Diagnostic accuracy using DWI (84 %, 21/25) was significantly better than that using conventional MRI (40 %, 10/25) for the confident characterisation of solid or cystic nature of the mediastinum (P = 0.002) (Table 6).
Discussion
Non-neoplastic cysts need to be differentiated from solid masses in the mediastinum. If imaging features identify the pure cystic nature of non-neoplastic cysts, these patients can be spared surgery by ruling out the possibility of neoplasm. Many neoplastic masses in the mediastinum demonstrate CT features of the enhancing solid component and radiologists can suggest the possibility of solid or neoplastic masses considering the patient’s age, sex and lesion location. Sometimes, though, it is difficult to be confident in characterising internal nature of mediastinal masses using CT. In our series, 61 patients (22 %) out of 274 with a mediastinal mass underwent MRI for further characterisation of mediastinal masses of indeterminate internal characteristics on CT. In our patients who underwent both MRI and CT, CT features were not helpful in the differentiation of non-neoplastic cysts from solid masses, as their morphological features and net enhancement were not significantly different (P > 0.05).
The overlapping features on CT may arise from the following reasons. The attenuation values of cystic masses can be higher than that of water when an internal component such as haemorrhage, proteinous mucus or calcium increases attenuation values on unenhanced CT images [13–17]. On the other hand, solid masses may look like non-neoplastic cysts when they accompany extensive necrotic or cystic degeneration [14, 18, 19]. McAdams et al. [15] reported that 34 % of histopathologically proved bronchogenic cysts in the mediastinum were considered solid or indeterminate soft-tissue lesions on CT because of lack of internal enhancement, high attenuation at unenhanced CT, atypical location or streak artefacts. They suggested the usefulness of T2-weighted MR images in characterising the cystic nature of mediastinal masses by showing markedly increased signal intensity in true cysts.
We found that 80 % (8/10) of cysts showed higher signal intensity than that of CSF on T2-weighted MR images, suggesting true cysts. However, 47 % (7/15) solid masses also showed higher signal intensity on T2-weighted MR images than that of water and it was difficult to differentiate solid and cystic masses using conventional T2-weighted MR images. Because we analysed cysts with complex appearance and density on CT, an internal component such as proteinous mucus might increase signal intensity of cysts higher than that of CSF due to partly remained T1 weighting at our T2-weighted turbo spin echo sequence with rather short TR of 2,000 ms and cysts with subacute or chronic haemorrhage might show low signal intensity on T2-weighted MR images. Conventionally, it is well known that enhanced MR can differentiate cystic and solid lesions. However, in our study, solid mass showed no significant enhancement within the mass in 67 % (10/15), because our cases started from lesions with equivocal or no enhancement at enhanced CT in the first place and then MR was performed as a problem-solving method. Solid masses can be seen as high-signal-intensity lesions on T2-weighted images and as non-enhancing lesions when extensive cystic degeneration or necrosis was seen on pathological correlation [20, 21].
DWI characterises the mobility of water in the tissue, which can be less restricted in the true cysts than any other solid masses with or without cystic degeneration. The diffusion property of mediastinal masses can be visually assessed on DWI and quantitatively measured with ADC values. Most non-neoplastic cysts (90 %) showed marked suppression of signal intensity on high-b-value DWI, suggesting freely diffusible internal characteristics of the masses. In one case, a bronchogenic cyst showed persistent high signal intensity on high-b-value DWI, raising a possibility of diffusion restriction. However, the ADC value was more than 2.5 × 10-3 mm2/s and confirmed freely diffusible internal characteristics of the cyst. The hyperintensity on high-b-value DWI of the bronchogenic cyst can be caused by a long T2-relaxation time rather than a limited mobility of water, referring as T2-shine through effect. A different case of three solid masses (two schwannomas and one parathyroid adenoma) showed signal suppression on high-b-value DWI indicating free diffusion. However, they showed low ADC values of less than 2.5 × 10-3 mm2/s, suggesting less chance of being true cysts on the ADC map. This can be explained by hypocellularity of the tumour and loose integrity of the cellular membrane. With a cut-off ADC value of 2.5 × 10-3 mm2/s, we were able to characterise the internal component of mediastinal lesions with high confidence level than using CT or conventional MRI. The ADC is a quantitative tool which can provide cut-off values, not only for differentiation between solid and cystic internal characteristics, but also for differentiation between malignant and benign mediastinal lesion [22, 23]. Gümüştaş et al. [22] reported the cut-off value of ≤1.39 × 10−3 mm2/s indicated a malignant lesion with a sensitivity of 95 % and specificity of 87 %.
When strict criteria were applied to make a confident characterisation of the internal nature of mediastinal masses, the diagnostic accuracy of DWI (84 %) was significantly better than that of conventional MRI (40 %) using T1- and T2-weighted images and enhanced T1-weighted images in our patients. In the case of mediastinal masses that are indeterminate on CT, DWI seems to be a better option in providing additional information to radiologists when evaluating patients who have solid or cystic lesions of the mediastinum. With the use of DWI, we may decrease unnecessary follow-up CT referrals or unnecessary surgery.
Our study had some limitations. The first limitation was the relatively small number of patients. We limited our study population only to patients with histopathologically confirmed lesions in order to obtain undebatable reference standards. Besides these enrolled patients, there were patients who were found to have non-neoplastic cysts (n = 27) after being considered true cysts at DWI. These mediastinal lesions showed typical cystic characteristics on DW images and ADC map, and thus only followed-up. Secondly, the cut-off value of 2.5 × 10-3 mm2/s needs to be validated in another group of patients with mediastinal lesions. The threshold of the ADC value for the differentiation of the solid and non-neoplastic cyst lesions was based on a phantom study by Matoba et al. [11]. In vivo imaging gave wide ranges of ADC values for the cysts depending on the lesion location, the MR system used, the choice of b values and the fluid content of the lesion of interest [24–27].
In conclusion, DWI can help evaluate tissue composition in mediastinal masses and thus reduce unnecessary thoracic surgery for non-neoplastic benign cystic lesions.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- CSF:
-
Cerebrospinal fluid
- DWI:
-
Diffusion-weighted MR imaging
- HU:
-
Hounsfield units
- ROI:
-
Region of interest
References
Zambudio AR, Lanzas JT, Calvo MJ, Fernandez PJ, Paricio PP (2002) Non-neoplastic mediastinal cysts. Eur J Cardiothorac Surg 22:712–716
Duwe BV, Sterman DH, Musani AI (2005) Tumors of the mediastinum. Chest 128:2893–2909
Kim JH, Goo JM, Lee HJ et al (2003) Cystic tumors in the anterior mediastinum. Radiologic-pathological correlation. J Comput Assist Tomogr 27:714–723
Jeung MY, Gasser B, Gangi A et al (2002) Imaging of cystic masses of the mediastinum. Radiographics 22:S79–S93
Tomiyama N, Honda O, Tsubamoto M et al (2009) Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol 69:280–288
Padhani AR, Liu G, Koh DM et al (2009) Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia 11:102–125
Lang P, Wendland MF, Saeed M et al (1998) Osteogenic sarcoma: noninvasive in vivo assessment of tumor necrosis with diffusion-weighted MR imaging. Radiology 206:227–235
Sugahara T, Korogi Y, Kochi M et al (1999) Usefulness of diffusion-weighted MRI with echo-planar technique in the evaluation of cellularity in gliomas. J Magn Reson Imaging 9:53–60
Gauvain KM, McKinstry RC, Mukherjee P et al (2001) Evaluating pediatric brain tumor cellularity with diffusion-tensor imaging. AJR Am J Roentgenol 177:449–454
Yi CA, Jeon TY, Lee KS et al (2007) 3-T MRI: usefulness for evaluating primary lung cancer and small nodules in lobes not containing primary tumors. AJR Am J Roentgenol 189:386–392
Matoba M, Tonami H, Kondou T et al (2007) Lung carcinoma: diffusion-weighted MR imaging—preliminary evaluation with apparent diffusion coefficient. Radiology 243:570–577
Henzler T, Schmid-Bindert G, Schoenberg SO, Fink C (2010) Diffusion and perfusion MRI of the lung and mediastinum. Eur J Radiol 76:329–336
Yernault JC, Kuhn G, Dumortier P, Rocmans P, Ketelbant P, De Vuyst P (1986) “Solid” mediastinal bronchogenic cyst: mineralogic analysis. AJR Am J Roentgenol 146:73–74
Glazer HS, Siegel MJ, Sagel SS (1989) Low-attenuation mediastinal masses on CT. AJR Am J Roentgenol 152:1173–1177
McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S (2000) Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 217:441–446
Glazer HS, Molina PL, Siegel MJ, Sagel SS (1991) High-attenuation mediastinal masses on unenhanced CT. AJR Am J Roentgenol 156:45–50
Fischbach R, Benz-Bohm G, Berthold F, Eidt S, Schmidt R (1994) Infradiaphragmatic bronchogenic cyst with high CT numbers in a boy with primitive neuroectodermal tumor. Pediatr Radiol 24:504–505
Kumar AJ, Kuhajda FP, Martinez CR, Fishman EK, Jezic DV, Siegelman SS (1983) Computed tomography of extracranial nerve sheath tumors with pathological correlation. J Comput Assist Tomogr 7:857–865
Cohen LM, Schwartz AM, Rockoff SD (1986) Benign schwannomas: pathologic basis for CT inhomogeneities. AJR Am J Roentgenol 147:141–143
Sakai F, Sone S, Kiyono K et al (1992) Intrathoracic neurogenic tumors: MR-pathologic correlation. AJR Am J Roentgenol 159:279–283
Suh JS, Abenoza P, Galloway HR, Everson LI, Griffiths HJ (1992) Peripheral (extracranial) nerve tumors: correlation of MR imaging and histologic findings. Radiology 183:341–346
Gümüştaş S, Inan N, Sarisoy HT et al (2011) Malignant versus benign mediastinal lesions: quantitative assessment with diffusion weighted MR imaging. Eur Radiol 21:2255–2260
Tondo F, Saponaro A, Stecco A et al (2011) Role of diffusion-weighted imaging in the differential diagnosis of benign and malignant lesions of the chest-mediastinum. Radiol Med 116:720–733
Taouli B, Koh DM (2010) Diffusion-weighted MR imaging of the liver. Radiology 254:47–66
Razek AA, Elmorsy A, Elshafey M, Elhadedy T, Hamza O (2009) Assessment of mediastinal tumors with diffusion-weighted single-shot echo-planar MRI. J Magn Reson Imaging 30:535–540
Inan N, Arslan A, Akansel G et al (2007) Diffusion-weighted imaging in the differential diagnosis of simple and hydatid cysts of the liver. AJR Am J Roentgenol 189:1031–1036
Tsuruda JS, Chew WM, Moseley ME, Norman D (1990) Diffusion-weighted MR imaging of the brain: value of differentiating between extraaxial cysts and epidermoid tumors. AJR Am J Roentgenol 155:1059–1065, discussion 1066-1058
Acknowledgments
C.A. Yi was a guarantor of entire study. C.A. Yi and K.E. Shin developed the design and the organisation of this study, participated in all stages of the study, made the initial interpretation of the study findings, and prepared the first draft of the manuscript. C.A. Yi was responsible for the MRI scanning and had overall responsibility for all MRI features of the study. T.S. Kim and H.Y. Lee researched on references and contributed to manuscript writing. Y.S. Choi, H.K. Kim and J. Kim were responsible for patient enrolment and the management of the clinical data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shin, K.E., Yi, C.A., Kim, T.S. et al. Diffusion-weighted MRI for distinguishing non-neoplastic cysts from solid masses in the mediastinum: problem-solving in mediastinal masses of indeterminate internal characteristics on CT. Eur Radiol 24, 677–684 (2014). https://doi.org/10.1007/s00330-013-3054-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-3054-0