Abstract
Objectives
The aim of this prospective study was to compare the painful subacromial gliding limitation of the supraspinatus tendon (SGLS) during dynamic ultrasonography, the features of magnetic resonance arthrography (MRA), and the maximum intra-articular injection volume to predict decreased joint capacity of the shoulder joint.
Methods
Between January 2003 and August 2011, 67 patients prospectively underwent ultrasonography including dynamic examination and MRA. Ultrasonography and ultrasonography-guided injection of contrast medium was performed before MRA, and each SGLSdU was compared with injected contrast volume, which was assumed as the maximum joint capacity and MRA features.
Results
Forty-seven patients (70.1%) were revealed as SGLS-positive, and 20 patients (29.9%) were revealed as SGLS-negative by dynamic ultrasonography. Pearson’s correlation coefficient between SGLS and the injection volume was -0.764 (P < 0.001). The value between SGLS and MRA features was 0.711 (P < 0.001). The mean injected volume of the SGLS-positive (22.0 ml) and negative group (10.7 ml) was significantly different (P < 0.001).
Conclusions
SGLS at ultrasonography correlated well with MRA features and the maximum intra-articular injection volume. This sign could predict the decreased capacity of the shoulder joint, an important feature of adhesive capsulitis, and increase the usefulness of dynamic ultrasonography.
Key Points
• Dynamic ultrasound is increasingly used in the evaluation of the shoulder.
• This can assess subacromial gliding limitation of the supraspinatus tendon (SGLS)
• SGLS appeared inversely proportional to the maximum volume of intra-articular injection.
• Dynamic ultrasonography findings correlated well with MR arthrographic features of adhesive capsulitis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adhesive capsulitis (AC), also known as a frozen shoulder, is a clinical syndrome characterised by the gradual worsening of pain and limitation of both active and passive shoulder joint motion [1–3]. Since the clinical presentation of AC can mimic several other shoulder disorders, various imaging investigations have been used to identify AC, which include magnetic resonance (MR) imaging, ultrasonography, nuclear medicine and arthrography [4–9]. Conventional shoulder arthrography has been considered to be the ‘gold standard’ investigation for adhesive capsulitis. However, in some cases, this method has been shown to be unreliable, invasive, and inordinate to evaluate only AC. Recently, MR arthrography (MRA) and ultrasound have gained increasing popularity, and previous studies suggested several important features of AC [5–9, 11–14]. Ryu et al. [16] reported that the limited supraspinatus tendon (SSP) movement during dynamic scanning was a sensitive and specific sign of AC. We presumed that painful subacromial gliding limitation of the supraspinatus tendon (SGLS) during dynamic ultrasonography is the result of physiological changes such as decreased joint capacity or joint stiffness. To our knowledge, no previous report about the relevance between ultrasonography findings and joint capacity exists. The purpose of this study was to evaluate if assessment of SGLS can predict decreased joint capacity by comparing it with the maximum injection volume of contrast media for MRA, since decreased joint capacity might reflect capsular stiffness. In addition, we compared the results of dynamic ultrasonography with MR arthrographic features to investigate the association of functional impairment with the morphological changes on MR images.
Materials and methods
Patients
Our prospective study was approved by the institutional review board of Kyungpook National University, and the informed consent requirement was waived. Between January 2003 and August 2011, 647 patients underwent MRA using ultrasound-guided intra-articular injections of contrast media. Among them, 95 patients who have non-specific shoulder pain or restricted shoulder motion were included in this study. They had no previous history of trauma or surgery around the shoulder area, and no patient refused passive abduction or injection of contrast agent due to pain. However, we excluded 28 patients who depicted problems other than adhesive capsulitis, such as the superior impingement syndrome, rotator cuff tendinopathy, such as a tear or prominent tenosynovitis, joint capsular rupture, and bony or labral abnormalities indicating joint instability on either ultrasonography or MR imaging. Particularly, we also excluded the patients who depicted subacromial-subdeltoid bursitis, an abnormality of the acromial undersurface, decreased acromio-humeral distance, which could indicate superior impingement syndrome that is often confused with AC in clinical assessment. Finally, we analyzed 67 patients with non-specific pain and restricted motion of the shoulder (32 male; 35 female; mean age 49.7).
Protocols of ultrasonography and contrast media injection
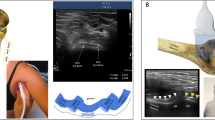
Every ultrasound scan was performed 30 min before MRA and contrast medium was injected under real-time ultrasonography guidance through the posterolateral approach. Two radiologists (J.L., J.H.Y.) with 10 and 5 years of experience in musculoskeletal ultrasound, respectively, performed ultrasonographic examinations using a 12– to 7-MHz linear-array transducer (ATL HDI 5000, Advanced Technologies Laboratory, Bothell, WA, USA). Patients were examined in the supine and decubitus positions according to the standard protocol of our institute, which includes the evaluation of the rotator cuff myotendinous structure, bursal space and rotator cuff interval including the coracohumeral ligament, acromioclavicular joint with the coracoacromial ligament, and a dynamic study of the subacromial gliding limitation of the supraspinatus tendon (SGLS). The dynamic ultrasonographic evaluation was performed on patients in the decubitus position with the arms in pronation position. With the transducer positioned between the greater tuberosity and acromion, an assistant raised the patient’s arm and the SSP was traced in a coronal oblique plane during full-range passive abduction. The degree of SGLS was scored from 0 to 3. A score of 1–3 was defined as limited subacromial gliding, and a score 0 was regarded as normal (Table 1, Fig. 1). However, we just classified positive and negative groups in this study to reduce bias due to ambiguous criteria among the grades. After completion of the standard ultrasonographic examination, contrast media for the subsequent MRA was injected. A syringe with 25 ml diluted gadopentetate dimeglumine (Magnevist; Schering, Berlin, Germany) was prepared at a concentration of 2 mmol/l. With the patient in the prone position, an injection was performed using ultrasound guidance by the posterolateral approach. At first, a 20-gauge needle was advanced into the glenohumeral joint through the infraspinatus muscle, and then an intra-articular injection was performed. The injection process was discontinued when the contrast passage to the joint was impeded by marked resistance or a maximum of 25 ml was injected if there was no resistance. At this time, the volume of injected contrast media was measured from the line scale of the syringe, and we assumed the injected volume as the maximum joint capacity. Generally, the injected volume of contrast medium for MRA of the shoulder joint is 10–15 ml, but we thought the volume would be insufficient to evaluate the maximum joint capacity [15]. Furthermore, a previous study with fresh cadavers described the capacity of the shoulder joint of adults as varying from 28 to 35 ml [19]. Accordingly, we set 25 ml as the maximum injection volume to prevent capsular rupture by excessive contrast media. In addition, we obtained informed consent about a greater potential of capsular rupture and shoulder pain during or after the procedure. During every injection, ultrasonographic inspection was performed to ascertain whether or not capsular rupture occurred. In addition, MR arthrographic image review and further clinical observation were made after examination.
Subacromial gliding limitation of the supraspinatus tendon on dynamic ultrasonography (SGLSdU). a, b Ultrasound scan of the shoulder of a 52-year-old patient showing negative features with a well-defined supraspinatus tendon (SSP) in the neutral position (a), and complete gliding of the SSP beneath the acromion followed by a distinct downward tilting of acromion during passive abduction of the shoulder (b). c Dynamic ultrasound scan of a 52-year-old patient showing a grade 1 limitation with complete gliding of the SSP without downward tilting of the acromion; note the localized joint fluid congestion between the acromion and the SSP tendon. d Dynamic ultrasound scan of a 55-year-old patient showing a grade 2 limitation with incomplete subacromial gliding of the SSP tendon. e Dynamic ultrasound scan of a 53-year-old patient showing a continuously visualized SSP tendon with severe gliding limitation. (A acromion, A supraspinatus tendon, H humeral head)
MR imaging protocol
MR imaging was performed within 30 min after administration of the contrast agent at 3.0 T (Signa Excite; GE Healthcare, Milwaukee, WI), using a phased array surface coil (Shoulder Array; Medrad, Indianola, PA, USA). Patients were placed so that the humerus was in a neutral position. Fat-suppressed T1-weighted sequences (TR range/TE range, 450-800/11-16) were performed in the axial, coronal oblique (parallel to the long axis of the supraspinatus tendon), and sagittal oblique (perpendicular to the long axis of the supraspinatus tendon) planes. Double-echo fast spin-echo pulse sequences were used to obtain coronal oblique intermediate-weighted MR images (3,000-4,500/14-21 ms) and T2-weighted MR images (3,000-4,500/63-112 ms) using an echo train length of 10. MR imaging parameters for all sequences were the following: field of view, 15-16 cm; 1-2 excitations; matrix size, 256 × 256; section thickness, 3 mm; intersection gap, 0.3 mm. We defined the ‘MR arthrographic positive group’ of adhesive capsulitis as follows: (1) thickening of the coracohumeral ligament (CHL) greater than 4 mm on sagittal oblique T1-weighted images, (2) thickness of the joint capsule in the rotator cuff interval greater than 7 mm on sagittal oblique T1-weighted images, (3) thickness of the capsule and synovium greater than 3 mm at the level of the axillary recess on oblique coronal T2-weighted images [9, 12].
Data analysis
The images were interpreted by two experienced musculoskeletal radiologists (J.L., J.H.Y.) by consensus. Pearson’s correlation coefficients were calculated to evaluate relevance (1) between SGLS and the mean injected volume and (2) between SGLS and MRA, respectively. After analysis, Fisher’s exact tests were used to evaluate the relationship. Statistical analysis was performed with a statistical software package (SPSS for Windows, version 18.0, SPSS). A statistically significant difference was defined as P < 0.05.
Results
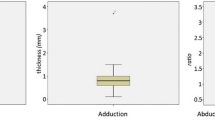
Among the 67 patients, 47 (70.1%; male 17; female 30; mean age 52.5) were revealed as SGLS-positive, and 20 (29.9%; male 15; female 5; mean age 43.2) were revealed as SGLS-negative during the dynamic ultrasonography. After the injections, no patient suffered a ruptured joint capsule. Between the SGLS-positive and SGLS-negative groups, the maximum injection volume and MR arthrographic features were analysed, respectively (Table 2 and Figs. 2, 3). Correlation analyses were also performed to evaluate the relationship and Pearson’s correlation coefficient between SGLS and the maximum intra-articular injection volume was -0.764 (P < 0.001). The value between SGLS and MR arthrographic features was 0.711 (P < 0.001). These results suggested SGLS to be inversely proportional to the maximum injection volume and to be directly proportional to the MR arthrographic features with a strong linear relationship. The difference of the mean injected volume between the SGLS-positive (22.0 ml; range 9–25 ml) and SGLS-negative group (10.7 ml; range 3.5–15 ml) was significant (P < 0.001) (Fig. 4). Nine patients (13.4%; male 3; female 6; mean age 54.1) showed discordant results between MRA and dynamic ultrasonography. Two patients showed SGLS-negative and SGLS-positive features on MRA, and the other seven patients showed SGLS-positive and SGLS-negative features on MRA. The mean injection volume of all nine patients was decreased to 10.5 ml (range 3.5–15 ml).
The dynamic ultrasonography and MR arthrography of a 63-year-old woman showing complete gliding of the supraspinatus tendon (SSP) where the downward tilting of the acromion was not demonstrated and subacromial gliding limitation of the supraspinatus tendon (SGLS) was grade 1 (a), thickened coracohumeral ligament (CHL) in rotator interval (arrow), synovitis-like abnormality around the axillary recess (arrowheads) on sagittal oblique T1-weighted image (b), and discrete capsular thickening of axillary recess (white arrows) measuring 7.2 mm on the humeral aspect on an oblique coronal T2-weighted image (c). The measured maximum injection volume of contrast medium was decreased at 6 ml
The dynamic ultrasonography and MR arthrography of a 52-year-old woman showing incomplete gliding of the SSP, SGLS grade 3 (a), thickened CHL (white arrow) on a sagittal oblique T1-weighted image (b), and thickened capsule of axillary recess (white arrows) measuring 7.5 mm on the humeral aspect on an oblique coronal T2-weighted image (c). The injection volume was 5 ml
A box plot of intra-articular contrast injection volume and subacromial gliding limitation of the supraspinatus tendon (SGLS). The rectangle contains the values of the injection volume of the two central quartiles (50% of the values) being the first and the fourth quartiles represented by the upper and lower limit of the vertical line and the median is the horizontal line in the rectangles
Discussion
Adhesive capsulitis is a common clinical problem with an uncertain pathogenesis that causes gradual restriction of movement and pain. The main pathological change of AC is inflammation combined with a fibrotic reaction leading to thickening, contraction, and subsequent adhesion of the synovium and capsule [2, 3]. The most important factors to diagnose AC are history, clinical signs and symptoms of the patient. However, because of the inaccuracy of the clinical assessments, the patients with clinically suspicious AC often need further image-based evaluation [17]. The conventional shoulder arthrography had been a main imaging modality to investigate AC and the arthrographic features of AC include a small contracted joint capsule with a decreased joint capacity of less than 10-12 ml, a small contracted axillary recess, and reduced filling of the biceps long head tendon sheath with contrast medium [10]. Recently, several imaging investigations have been used to diagnose AC and many investigators have reported on the MR and ultrasonographic features of AC [5–7, 11–14, 20, 21]. MRA features of AC include abnormally enhancing soft tissue lesions in the rotator interval together with enhancement of the joint capsule and periarticular soft tissue in the region of the axillary recess. The additional specific features of AC have been reported to be obliteration of the subcoracoid fat triangle, thickening of the coracohumeral ligament and joint capsule, decreased axillary recess volume, and thickening of the capsule and synovium at the level of the axillary recess. The ultrasonographic features of AC have been described as entrapped fluid within the biceps long head tendon sheath, a combination of increased vasculature and hypoechoic changes around the rotator interval, and thickening of the coracohumeral ligament of more than 3 mm.
However, previous papers have focused on the morphological changes with little attention to the identification of decreased joint capacity, which might be more closely associated with the functional impairment associated with AC. Although the indirect measurement of the axillary recess volume based on the height and width of the axillary recess was suggested as a feature of decreased capacity of less than 10-12 ml in a study using MRA, the results provided limited information about the capacity of the whole joint [9]. In this study, we found a strong linear relationship between SGLS and MR arthrographic features, and SGLS is well correlated with the decreased maximum injection volume. SGLS could predict the decreased capacity of the shoulder joint, which is an important feature of AC, and dynamic ultrasound could be a useful diagnostic technique to evaluate AC. Nine patients showed discordant results between MRA and dynamic ultrasound, but the mean injection volume of all nine patients was decreased to 10.5 ml. According to this result, we could expect the decreased maximum injection volume if the patient showed positive findings on either of the MRA or dynamic ultrasonography. The superiority between MRA and dynamic ultrasonography could not be evaluated because of the small number of patients. However, the seven SLGS-positive patients with a negative result on MRA outnumbered the two SGLS-negative patients with a positive result on MRA; thus, we presumed the SGLSdU represented functional impairment more sensitively than MRA. Compared with MRA, ultrasonography is less costly, non-invasive, and capable of evaluating other common shoulder diseases, and subsequent dynamic study is also useful to verify functional impairment [16]. In this study, the ultrasonography findings correlated well with MR arthrographic features indicating AC and it can predict decreased capacity of the shoulder joint without any invasive measurement. The superior impingement syndrome is also common cause of functional impairment of shoulder movement and it is often confused with AC in clinical assessment. However, it may be present in the midrange of motion during active abduction and resisted movements are painful and may be partially restricted, whereas passive movements are full, albeit painful. However, AC is characterised by global pain, along with restriction of all movements, both active and passive [17, 18]. Therefore, dynamic ultrasonography during passive abduction could also increase reliability to diagnose AC rather than impingement.
There are three major limitations of this study. First, the determination of the maximum injection volume depended on the subjective opinion of US performers. We think that a quantitative method such as intra-articular manometry might give more objective information about the joint capacity in future studies. Second, we excluded patients with combined or secondary AC. In this study, all patients with any other common shoulder problems, which are commonly combined with AC, were excluded to reduce confounding factors, which allowed us to focus on patients who we suspected of possessing only AC. Therefore, in the patients having combined AC, the significance of SGLS could not be determined, and so further studies may be necessary. The final limitation of our study was the large amount of injected contrast medium (25 ml). This is not routine, and we did not perform a long-term follow-up to determine if the patients had any sequelae. However, no patient revealed the rupture of the joint capsule or complained of any immediate discomfort. According to our results, a general dose of 10-12 ml may be the lowest amount needed to evaluate the maximum joint capacity [15]. We suggest setting the maximum injection volume for MRA of the shoulder joint at more than 15 ml in cases of non-specific pain with motion limitation of the shoulder, since there were patients who received 15 ml as the maximum injected volume in the SGLS-positive group.
In conclusion, dynamic ultrasonography to assess SLGS correlated well with the decreased maximum intra-articular injected volume and MR arthrographic features.
References
Revel M, Ghanem N (1999) Adhesive capsulitis of the shoulder. Rev Prat 49(13 Suppl):1406–1408
Neviaser RJ, Neviaser TJ (1987) The frozen shoulder. Diagnosis and management. Clin Orthop Relat Res 223:59–64
Hulstyn MJ, Weiss AP (1993) Adhesive capsulitis of the shoulder. Orthop Rev 22:425–433
Binder AI, Bulgen DY, Hazleman BL, Tudor J, Wraight P (1984) Frozen shoulder: an arthrographic and radionuclear scan assessment. Ann Rheum Dis 43:365–369
Carrillon Y, Noel E, Fantino O, Perrin-Fayolle O, Tran-Minh VA (1999) Magnetic resonance imaging findings in idiopathic adhesive capsulitis of the shoulder. Rev Rhum Engl Ed 66:201–206
Emig EW, Schweitzer ME, Karasick D, Lubowitz J (1995) Adhesive capsulitis of the shoulder: MR diagnosis. AJR Am J Roentgenol 164:1457–1459
Homsi C, Bordalo-Rodrigues M, da Silva JJ, Stump XM (2006) Ultrasound in adhesive capsulitis of the shoulder: is assessment of the coracohumeral ligament a valuable diagnostic tool? Skeletal Radiol 35:673–678
Manton GL, Schweitzer ME, Weishaupt D, Karasick D (2001) Utility of MR arthrography in the diagnosis of adhesive capsulitis. Skeletal Radiol 30:326–330
Mengiardi B, Pfirrmann CW, Gerber C, Hodler J, Zanetti M (2004) Frozen shoulder: MR arthrographic findings. Radiology 233:486–492
Neviaser TJ (1980) Arthrography of the shoulder. Orthop Clin North Am 11:205–217
Connell D, Padmanabhan R, Buchbinder R (2002) Adhesive capsulitis: role of MR imaging in differential diagnosis. Eur Radiol 12:2100–2106
Jung JY, Jee WH, Chun HJ, Kim YS, Chung YG, Kim JM (2006) Adhesive capsulitis of the shoulder: evaluation with MR arthrography. Eur Radiol 16:791–796
Lee JC, Sykes C, Saifuddin A, Connell D (2005) Adhesive capsulitis: sonographic changes in the rotator cuff interval with arthroscopic correlation. Skeletal Radiol 34:522–527
Lefevre-Colau MM, Drape JL, Fayad F et al (2005) Magnetic resonance imaging of shoulders with idiopathic adhesive capsulitis: reliability of measures. Eur Radiol 15:2415–2422
Zubler V, Mamisch-Saupe N, Pfirrmann CW, Jost B, Zanetti M (2011) Detection and quantification of glenohumeral joint effusion: reliability of ultrasound. Eur Radiol 21:1858–64
Ryu KN, Lee SW, Rhee YG, Lim JH (1993) Adhesive capsulitis of the shoulder joint: usefulness of dynamic sonography. J Ultrasound Med 12:445–449
Cools AM, Cambier D, Witvrouw EE (2008) Screening the athlete’s shoulder for impingement symptoms: a clinical reasoning algorithm for early detection of shoulder pathology. Br J Sports Med 42:628–635
Mitchell C, Adebajo A, Hay E, Carr A (2005) Shoulder pain: diagnosis and management in primary care. BMJ 331:1124–1128
Neviaser JS (1962) Arthrography of the shoulder joint: study of the findings in adhesive capsulitis of the shoulder. Study of the findings in adhesive capsulitis of the shoulder. J Bone Joint Surg Am 44-A:1321–1359
Tamai K, Yamato M (1997) Abnormal synovium in the frozen shoulder: a preliminary report with dynamic magnetic resonance imaging. J Shoulder Elbow Surg 6:534–543
Lee MH, Ahn JM, Muhle C et al (2003) Adhesive capsulitis of the shoulder: diagnosis using magnetic resonance arthrography, with arthroscopic findings as the standard. J Comput Assist Tomogr 27:901–906
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, I., Yi, J.H., Lee, J. et al. Limited subacromial gliding of the supraspinatus tendon during dynamic ultrasonography can predict a decrease in capacity and MR arthrographic features of the shoulder joint. Eur Radiol 22, 2365–2370 (2012). https://doi.org/10.1007/s00330-012-2513-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2513-3