Abstract
Objectives
To assess the long-term stability of small (<10 mm) non-calcified pulmonary nodules (NCNs) in high-risk subjects initially screened for lung cancer using low-dose chest computed tomography (LDCCT).
Methods
A total of 449 subjects initially underwent screening with serial LDCCT over a 2-year period. Participants identified as having NCNs ≥10 mm were referred for formal lung cancer workup. NCNs <10 mm diameter were followed in accordance with the study protocol. Seven years after baseline screening, subjects with previously documented NCNs <10 mm, which were unchanged in size after the 2-year follow-up period, were re-imaged using LDCCT to assess for interval nodule growth.
Results
Eighty-three subjects with previously documented stable NCNs <10 mm underwent LDCCT at 7 years. NCNs were unchanged in 78 subjects and had decreased in size in 4 subjects. There was interval growth of an NCN (from 6 mm to 9 mm) in one subject re-imaged at 7 years, but this nodule has remained stable in size over a further 2-year follow-up period.
Conclusions
Non-calcified pulmonary nodules <10 mm in size that are unchanged in size or smaller after 2 years of follow-up with LDCCT are most likely benign.
Key Points
• Computed tomography is increasingly used for screening for lung cancer.
• However CT frequently reveals unsuspected lung nodules.
• Seven-year follow-up of small (<10 mm) non-calcified pulmonary nodules is reassuring.
• Even in high-risk patients most nodules will likely be benign.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer-related death among men and women in developed countries [1]. The cure rate for lung cancer is approximately 12 % and 5-year survival rates across Europe range from 5.5 to 14 % [2, 3]. In Ireland, only 10 % of men and 8.5 % of women survive to 5 years following diagnosis [3]. Outcome in patients diagnosed with lung tumours is strongly related to disease stage at discovery. The 5-year survival rate for CT (computed tomography)-detected stage IA non-small cell malignancies (NSCLC) measuring <20 mm has been reported to be >90 %, suggesting a curability rate for these malignancies of >80 % [4–6]. In Ireland, 80 % of cases are diagnosed at stages II to IV [3].
The benefits of early detection of lung cancer through screening using low-dose chest computed tomography (LDCCT) were recently established with the publication of the findings of the National Lung Screening Trial (NLST) [7]. Conducted by the National Cancer Institute (NCI) in the United States, this study reported reductions in lung cancer deaths (20.3 %) and all-cause mortality (6.9 %) among patients in the LDCCT arm [7]. Unfortunately, the low specificity of LDCCT necessitates the follow-up of a large number of small (<10 mm) pulmonary nodules that ultimately turn out to be benign, and there are few data regarding the benefit of long-term follow-up (>2 years) of sub-centimetre non-calcified pulmonary nodules (NCNs). Data pertaining to the natural history of these nodules will have important implications for cost benefit analysis in any future LDCCT screening programmes. Here we report on the long-term follow-up of small (<10 mm) NCNs, detected while screening for lung cancer using LDCCT, which were stable in terms of size after an initial 2-year follow-up period. Subjects were re-examined by LDCCT 7 years after baseline screening to assess the longer-term stability of NCNs and to identify indolent lung cancers in our high-risk cohort.
Materials and methods
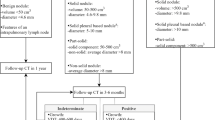
Institutional ethics committee approval was obtained. Our hospital is a national tertiary referral centre that serves a heterogeneous, multi-racial, inner city population of approximately 300,000 people in Dublin, Ireland, where the socio-economic status of patients ranges from social deprivation to upper class. Residents of this community aged 50 years or over, with a history of at least 10 pack years smoking and still smoking at the age of 45, with no prior history of cancer and who were medically fit for thoracic surgery were offered lung cancer screening by local media advertising [8]. All subjects provided written informed consent before enrolment. All subjects underwent initial baseline or prevalence CT, and the results of the prevalence CT study determined intervention or repeat screening as previously described [8]. Briefly, NCNs <10 mm in diameter were followed with LDCCT at 6, 12 and 24 months, larger nodules or those showing interval growth were referred for fine-needle aspiration biopsy (FNAB) and annual repeat LDCCT was recommended where no nodule was seen on prevalence imaging. In accordance with our study protocol all subjects with documented NCNs <10 mm in size that demonstrated no growth after a 2-year follow-up period were re-imaged 7 years after baseline screening to identify slow-growing lung cancers (Fig. 1).
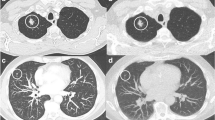
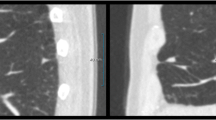
Helical 10-mm, pitch 2, low-dose (50 MA or less) CT images were obtained and reconstructed using a high-resolution algorithm in overlapping 5-mm increments. Images were obtained using a Siemens (Erlangen, Germany) Emotion six-slice helical CT system. Computed tomography examinations were independently evaluated by two radiologists. Previously documented NCNs were identified and a careful search was made for relevant new findings. Pre-defined characteristics for all nodules identified were recorded. These included the nodule size (minimum and maximum diameter), density (solid, part solid or ground-glass opacity), shape (round if maximum to minimum diameter ratio was <2–3, otherwise non-round), location (lobe and distance from pleura, central if more than 2 cm from pleura), margin (smooth, non-smooth), and the presence or absence of benign calcification. Other parenchymal, mediastinal, pleural and extra-thoracic abnormalities were recorded. If the findings of the two radiologists did not concur, the CT examinations were jointly re-evaluated and consensus findings were documented.
Results
Four hundred forty-nine subjects of median age 56.4 years (range 50–74), with a mean smoking history of 53.4 pack years, fulfilling the inclusion criteria were initially enrolled (Table 1) [8]. Between baseline screening and interval imaging over a 2-year period, 1,371 LDCCT examinations were performed.
One hundred fifty-seven NCNs <10 mm were documented in 99 subjects at baseline screening. Nodules measuring <10 mm on prevalence screening were followed without change for 24 months in 97 of these subjects [9]. Two subjects had nodules that were found to have increased in size on the second interval CT and underwent workup in accordance with the study protocol [8]. Eighty-three of the 97 subjects who fulfilled the eligibility criteria for 7-year follow-up LDCCT were re-imaged (9 participants died of causes other than lung cancer, 4 subjects declined follow-up imaging and withdrew from the study, and 1 patient had an interval diagnosis of bronchoalveolar cell carcinoma, discussed below).
Of the 83 subjects re-imaged for this study 68 had been smokers at the time of enrolment and, of those who were non-smokers (n = 15), the mean number of years that had passed since quitting was 3.5 (range 0.4–8.5). Thirty-eight subjects were still smokers when they presented for their 7-year LDCCT examinations. The imaging characteristics of the 141 NCNs evaluated in these 83 subjects are outlined in Table 2.
At 7-year follow-up LDCCT pulmonary nodules were unchanged in size in 78 (94 %) subjects and had decreased in size in 4 (5 %) subjects. One participant was found to have had interval growth of a solid-appearing subpleural NCN from 6 mm to 9 mm. This nodule was subsequently followed in accordance with the study protocol and has demonstrated no further growth after an additional 2 years of follow-up.
In one subject a 3-mm peripheral NCN of ground-glass opacity (GGO) was identified at baseline screening and followed without change for 2 years in accordance with the study protocol. Too small to more accurately characterise, this nodule was felt to possibly represent an area of parenchymal scarring or early fibrosis. The subject defaulted on her first annual repeat LDCCT but subsequently presented to hospital 2 years after her final interval LDCCT (4 years from baseline imaging) with an exacerbation of emphysema, and imaging demonstrated that the previously stable 3 mm NCN had increased in size to 15 mm and appeared more solid. Following positive positron emission tomography (biopsy prohibited by sub-pleural positioning of the nodule immediately deep to a rib) this patient was treated with lobectomy and diagnosed histologically with bronchoalveolar cell carcinoma.
Significant new incidental thoracic lesions were detected in 14 subjects at 7-year follow-up CT [bronchiectasis (n = 6); emphysema (n = 5); coronary artery calcification (n = 3)].
Discussion
One solid-appearing NCN demonstrated interval growth from 6 mm to 9 mm between the 2-year and the 7-year follow-up CT examinations. This nodule was subsequently followed in accordance with the study protocol and has demonstrated no further interval growth after 2 years. It is our experience that solid NCNs unchanged or decreasing in size during follow-up for a minimum of 24 months can be considered benign. Growing nodules that do not resolve with short-term (2-year) follow-up should prompt appropriate further investigation, and part solid and ground-glass density nodules should be followed to resolution, even in the longer term. These findings must of course be interpreted with some caution given the relatively small number of participants ultimately followed to 7 years in this study.
The preliminary findings of the NLST in relation to the significant reductions in lung cancer deaths and all-cause mortality among high-risk patients screened with LDCCT have recently peaked interest internationally in the use of LDCCT as a screening tool for lung cancer. The low specificity of LDCCT necessitates follow-up of a large number of nodules that ultimately turn out to be benign. Current estimates of the prevalence of sub-centimetre NCNs are largely based upon the results of lung cancer screening studies with rates of between 8 % and 51 % reported at baseline screening in high-risk subjects [10]. It is likely that with widespread use of the latest generation of MDCT systems, and the probable widespread implementation of lung cancer screening programmes, an increasing number of smaller pulmonary nodules will be detected [11]. Following larger numbers of benign NCNs in greater numbers of patients would undoubtedly impact negatively on the cost-effectiveness of any future LDCCT screening programmes as well as increasing the number of non-invasive and invasive diagnostic tests that the discovery of a NCN inevitably triggers [11]. The ever-growing challenge facing radiologists is non-invasively distinguishing between benign and malignant NCNs.
The concept that temporal stability of small solid NCNs over a 2-year period implies benignity, central to recommendations published by the Fleischner Society [12] and advocated by both the American College of Radiology and the American College of Chest Physicians [13, 14], can be traced to an article by Good and Wilson published in 1958 [15], which was an extension of three articles published in 1953 that Good also co-authored [16–18]. Yankelevitz and Henschke, upon review of these original publications, found no data to support the statement made by Good and Wilson in 1958; in fact, contradictory conclusions were drawn. Using data from the original articles by Good et al., Yankelevitz and Henschke calculated the predictive value (taking no growth as the predictor for benignity) as 65 %, with estimated sensitivity and specificity values of only 40 % and 72 % respectively [19]. Although supported by decades of clinical experience and a small number of anecdotal reports, to our knowledge, no high-quality published data are available on the long-term (>5 years) natural history of NCNs to validate the conclusions drawn by Good and Wilson [15].
In the assessment of sub-centimetre NCNs an accurate estimation of size is critical to the detection of nodule growth as even the smallest detectable increase in nodule diameter could represent a doubling in nodule volume, known as the volume-doubling time (VDT). To extrapolate from this, if we assume that the smallest resolvable increase in size in a pulmonary nodule can be accurately measured using CT, 2-year stability in an NCN implies a doubling time of at least 730 days [20]. Doubling times can be expressed as direct volume measurements, as 2D area estimates or, as in the case of this study, as a 2D estimation of nodule diameter. The majority of malignant pulmonary nodules take, on average, between 30 and 400 days to double in volume [11, 21–24]. Lesions that double more rapidly are usually infectious (VDT of less than one month), whereas benign lesions (e.g. granulomas or hamartomas) typically have very long doubling times. These of course are only generalisations, and exceptions to this rule are not uncommon as tumour growth rates are variable, determined by histopathological type and vascular supply.
Malignancies that manifest as ground-glass opacities on CT imaging on the other hand tend to exhibit much longer VDTs, with mean doubling times in excess of 800 days reported [25]. As a general rule, ground-glass opacities tend to have longer VDTs than partly solid NCNs, which in turn tend to have longer VDTs than solid nodules [25]. As a result the “rule” that 2-year nodule stability implies benignity does not apply to GGOs or lesions whose morphology may be partly GGO. Such lesions should always be followed to resolution, as was the protocol in this study. The danger of not adhering to this principle was highlighted by the diagnosis of bronchoalveolar cell carcinoma from a 3-mm area of GGO, unchanged in either size or appearance after 2 years of surveillance, in one subject who defaulted on subsequent annual follow-up LDCCT.
A role for low-dose CT in screening for lung cancer is no longer contentious. Concerns remain however regarding the high false-positive and benign intervention rates that may result in unacceptable morbidity and reduce the cost-effectiveness of future screening programmes. Advancements in CT technology and the increasing number of smaller pulmonary nodules now detectable will compound these issues. A limitation of this study is the relatively small size of the cohort evaluated. Larger studies will be required to definitively determine optimal guidelines for the follow-up of sub-centimetre NCNs and to assess the cost-effectiveness of any proposed LDCCT screening programmes for lung cancer. This study suggests that LDCCT follow-up to 2 years is sufficient to determine benignity in solid NCNs and supports current guidelines and recommendations for the follow-up of sub-centimetre pulmonary nodules.
References
Shibuya K, Mathers CD, Boschi-Pinto C, Lopez AD, Murray CJ (2002) Global and regional estimates of cancer mortality and incidence by site: II. Results for the global burden of disease 2000. BMC Cancer 2:37
Henschke CI, McCauley DI, Yankelevitz DF et al (1999) Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet 354:99–105
Byrne AL, Logan PM (2006) Screening for lung cancer. Radiol Updat 5:85–91
Sobue T, Moriyama N, Kaneko M et al (2002) Screening for lung cancer with low-dose helical computed tomography: anti-lung cancer association project. J Clin Oncol 20:911–920
Henschke CI, Naidich DP, Yankelevitz DF et al (2001) Early lung cancer action project: initial findings on repeat screenings. Cancer 92:153–159
Noguchi M, Morikawa A, Kawasaki M et al (1995) Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer 75:2844–2852
Aberle DR, Adams AM, Berg CD et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409
Macredmond R, Logan PM, Lee MJ, Kenny D, Foley C, Costello RW (2004) Screening for lung cancer using low dose CT scanning. Thorax 59:237–241
Macredmond R, McVey G, Lee MJ et al (2006) Screening for lung cancer using low dose CT scanning: results of 2 year follow up. Thorax 61:54–56
Wahidi MM, Govert JA, Goudar RK, Gould MK, McCrory DC (2007) Evidence for the treatment of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132:94S–107S
Edey AJ, Hansell DM (2009) Incidentally detected small pulmonary nodules on CT. Clin Radiol 64:872–884
MacMahon H, Austin JH, Gamsu G et al (2005) Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 237:395–400
Khan A (2007) ACR Appropriateness Criteria on solitary pulmonary nodule. J Am Coll Radiol 4:152–155
Gould MK, Fletcher J, Iannettoni MD et al (2007) Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132:108S–130S
Good CA, Wilson TW (1958) The solitary circumscribed pulmonary nodule; study of seven hundred five cases encountered roentgenologically in a period of three and one-half years. J Am Med Assoc 166:210–215
Good CA (1953) Management of patient with solitary mass in lung. Chic Med Soc Bull 55:893–896
Good CA, Hood RT Jr, Mc DJ (1953) Significance of a solitary mass in the lung. Am J Roentgenol Radium Ther Nucl Med 70:543–554
Hood RT Jr, Good CA, Clagett OT, McDonald JR (1953) Solitary circumscribed lesions of the lung; study of 156 cases in which resection was performed. J Am Med Assoc 152:1185–1191
Yankelevitz DF, Henschke CI (1997) Does 2-year stability imply that pulmonary nodules are benign? AJR Am J Roentgenol 168:325–328
Lillington GA (1991) Management of solitary pulmonary nodules. Dis Mon 37:271–318
Winer-Muram HT, Jennings SG, Tarver RD et al (2002) Volumetric growth rate of stage I lung cancer prior to treatment: serial CT scanning. Radiology 223:798–805
Revel MP, Merlin A, Peyrard S et al (2006) Software volumetric evaluation of doubling times for differentiating benign versus malignant pulmonary nodules. AJR Am J Roentgenol 187:135–142
Yankelevitz DF, Reeves AP, Kostis WJ, Zhao B, Henschke CI (2000) Small pulmonary nodules: volumetrically determined growth rates based on CT evaluation. Radiology 217:251–256
Quint LE, Cheng J, Schipper M, Chang AC, Kalemkerian G (2008) Lung lesion doubling times: values and variability based on method of volume determination. Clin Radiol 63:41–48
Hasegawa M, Sone S, Takashima S et al (2000) Growth rate of small lung cancers detected on mass CT screening. Br J Radiol 73:1252–1259
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Slattery, M.M., Foley, C., Kenny, D. et al. Long-term follow-up of non-calcified pulmonary nodules (<10 mm) identified during low-dose CT screening for lung cancer. Eur Radiol 22, 1923–1928 (2012). https://doi.org/10.1007/s00330-012-2443-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2443-0