Abstract
Objectives
To investigate the safety of transarterial chemoembolisation (TACE) in combination with sorafenib in patients with hepatocellular carcinoma (HCC).
Methods
Patients with Child–Pugh A/B liver function, ECOG performance status 0–2 and HCC treatable with TACE received continuous sorafenib 800 mg/day, and TACE with doxorubicin (75, 50 and 25 mg/m2 according to serum bilirubin: <1.5, 1.5–3, and >3 mg/dL) and lipiodol 2 weeks after sorafenib initiation and repeated every 4 weeks.
Results
Fifteen patients were included (Child–Pugh A/B, n = 12/3; Barcelona Clinic Liver Cancer-A/B/C, n = 1/9/5; ECOG 0/2, n = 14/1). Median time on sorafenib was 5.2 months (2.6–7.4 months); median number of TACE sessions was 3. Common adverse events were abdominal pain (n = 14), weight loss (n = 13), alopecia (n = 12), fatigue (n = 12) and hyperbilirubinaemia (n = 11). There were 32 serious adverse events (grade ≥3); 9/10-unscheduled hospital admissions and 4/5 deaths were considered TACE-related. The study was stopped prematurely because of safety concerns. At 6 months, 2 and 5 patients had complete or partial responses; 1 had stable disease. Median overall survival was 10.6 months (95% CI: 5.2–16 months).
Conclusion
These findings do not support use of an intensive, high-dose doxorubicin-based TACE regimen in combination with sorafenib in this study population.
Key Points
• Transarterial chemoembolisation (TACE) is widely used in patients with hepatocellular carcinoma (HCC)
• Various antiangiogenic and other agents have been used to augment this treatment
• We tested lipiodol-TACE with bilirubin-adjusted doxorubicin dosing in combination with sorafenib
• This trial was stopped prematurely because of safety reasons
• Our safety results do not support the combination of sorafenib with this TACE regimen
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most common primary liver cancer worldwide [1] and prevalent among patients with liver cirrhosis. Hepatitis B or C virus infections, or chronic alcoholism are the most common underlying causes of the disease [2]. The management of HCC depends on tumour stage and the degree of liver dysfunction. Patients with intermediate-stage HCC are defined by moderately preserved liver function [Child–Pugh stage A or B], good Eastern Cooperative Oncology Group performance status [ECOG PS 0] and absence of macrovascular invasion or extrahepatic spread [EHS]. These patients are ineligible for surgical or local ablative treatments [3] and current treatment guidelines [3–5], including the Barcelona Clinic Liver Cancer (BCLC) group [6], recommend treatment with transarterial chemoembolisation (TACE).
Conventional TACE (TACE), is performed by embolising the tumour-feeding vessels with a mixture of lipiodol and doxorubicin or cisplatin, followed by vascular occlusion with gelatine particles or other embolising agents [7]. This leads to fairly selective hypoxic tissue damage within the tumours, while preserving the integrity of the surrounding liver tissue. Despite an improvement in survival of 4 months with TACE compared with symptomatic management in two clinical studies [8, 9] and in a meta-analysis [10], tumour recurrence after TACE is universal and the survival benefit is relatively small. Hence, new strategies are needed to improve the outcome of HCC patients undergoing TACE.
Sorafenib has been approved for the treatment of HCC after two successful phase III studies [11, 12]. Recently, the combination of sorafenib with systemically administered doxorubicin has shown promising overall survival in advanced HCC patients [13].
Sorafenib is a multityrosine kinase inhibitor with activity against RAF kinase, vascular endothelial growth factor (VEGF) receptors -1, -2, and -3, platelet-derived growth factor receptor-β, c-kit and RET [14]. The anti-angiogenic effects of sorafenib [15, 16] warrant its use in combination with TACE as VEGF-induced angiogenesis is implicated in tumour progression and post-TACE-survival [17, 18].
Various studies investigate sorafenib in combination with TACE, including a Phase I trial [19], three Phase II trials [20–23] and two Phase III trials (ECOG 1208 [ClinicalTrials.gov: NCT01004978] and TACE-2 [EudraCT: 2008-005073-36]). A Phase I study of sorafenib plus TACE [19], an interim analyses of two Phase II studies with TACE [20, 21] and one Phase II study with DEB-TACE [22, 23] all suggest a similar safety profile of this combination to that of each individual treatment, but final analyses of these studies are pending.
Although sorafenib in combination with TACE may be a promising strategy, further data are needed. There are questions regarding the optimal scheduling of anti-angiogenic therapies with TACE (continuous/interrupted/sequential schedules [24]), the optimal TACE schedule and doxorubicin dose to be used in combination with sorafenib [25], which require prospective studies.
The aim of this study was to evaluate the safety and efficacy of a fixed schedule of TACE with bilirubin-adjusted doxorubicin doses in combination with continuous sorafenib treatment in patients with HCC.
Materials and methods
Patient selection
Patients aged ≥18 years with cirrhosis of any aetiology and HCC confirmed by histology or European Association for the Study of the Liver (EASL) criteria [4] and not suitable for surgery were eligible for inclusion. Additional inclusion criteria were liver function at Child–Pugh stage A or B [26], ECOG-PS 0–2, ANC >1 × 109/L, platelet count >40 × 109/L, haemoglobin >9 g/dL, INR < 2.3, total bilirubin ≤3 mg/dL, serum creatinine <2.0 mg/dL and a life expectancy of >3 months.
Patients had to give written informed consent before any study-specific procedures were performed. Patients were excluded if they had complete portal vein thrombosis (PVT) or Child–Pugh stage C. Peripheral PVT was not an exclusion criterion. Additional exclusion criteria were previous TACE, history of variceal bleeding within the last 2 weeks, large oesophageal varices without prophylactic band ligation, any malignancies except for HCC and clinical findings reasonably contraindicating the use of sorafenib or TACE [25].
This study was approved by the local ethics committee of the Medical University of Vienna. This study was registered at ClinicalTrials.gov (Identifier: NCT00768937).
Study design
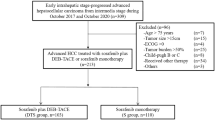
This was an open-label, single-arm, 6-month pilot study to evaluate the safety of TACE in combination with continuous sorafenib administration in up to 22 eligible patients with HCC. The study design is shown in Fig. 1.
Patients received sorafenib 400 mg twice daily (BID) p.o. starting 2 weeks before the first TACE session and every day thereafter until the patient withdrew consent, adverse events precluded continuation, or patient death. In the event of significant adverse events, sorafenib dose was reduced to 200 mg BID (if National Cancer Institute Common Toxicity Criteria [NCI-CTC] adverse event grade 3), interrupted or discontinued (if NCI-CTCAE grade ≥4). Dose reduction was also performed in cases of NCI-CTCAE grade 2 adverse events if intolerable for the patient. Dose re-escalation or restart of sorafenib was allowed after recovery to NCI-CTCAE grade <2 within 30 days, while otherwise the patient was permanently discontinued from sorafenib.
The first TACE session was performed 2 weeks after sorafenib administration started and repeated twice at 4-week intervals if both clinically feasible and contrast-enhanced tumour tissue on control CT was present. Additional TACE sessions were permitted if indicated (through consensus at the tumour board) and clinically feasible. No TACE was performed in the presence of complete radiological response.
Contraindications for TACE cycles were defined as clinical features obviating further TACE applications (occurrence of extrahepatic lesions, complete PVT, diffuse tumour growth and total bilirubin >5 mg/dL, deterioration to ECOG-PS ≥3 or to Child–Pugh-stage C).
After catheterisation of a femoral artery with a 5-french sidewinder catheter (Cordis©, Waterloo, Belgium) superselective embolisation of the hepatic artery branches feeding the tumour was performed. A microcatheter (Renegade HiFlo Kit 3Fr™ or Tracker, Boston Scientific, Nanterre, France or Progreat, Terumo, Somerset, NJ, USA) could be used to select the branch feeding the tumour depending on the anatomy of the individual patient.
TACE was done with doxorubicin (Pfizer Corporation©, Vienna, Austria) using 75, 50 and 25 mg/m2 according to serum bilirubin levels (<1.5, 1.5–3, and >3 mg/dL) and lipiodol (Guerbet©, Sulzbach, Germany) in a 1:1 ratio in a total volume of 20 mL as published [8]. Thereafter, embolisation was performed with beadblock microspheres (Beadblock™, Biocompatibles©, Farnham, UK) of 100–500 μm in size until stasis in the second- or third-order branches of the right or left hepatic artery occurred. For safety reasons only one liver lobe per session was treated in the case of bilobular tumour nodules.
Assessments
The primary endpoint was the safety of TACE in combination with sorafenib in patients with HCC.
Safety was assessed by documenting all adverse events from the start of treatment for at least 6 months of sorafenib therapy or until 12 weeks after the third TACE cycle. All adverse events were coded following the system organ class (SOC) and terminology of the Medical Dictionary for Regulatory Activities (MedDRA), and were graded using NCI-CTCAE version 3.0.
Patients visited the outpatient clinic at baseline, at week 2, 4 weeks after each TACE cycle (before the next TACE), and every 4 weeks thereafter during non-TACE cycles. Blood was drawn at all time points mentioned above and whenever clinically indicated. For TACE, patients were admitted to hospital and observed for at least 48 h after TACE, with daily adverse event assessments. All sorafenib dose interruptions, reductions or discontinuations, unscheduled hospital admissions and the median length of post-TACE hospital stays were recorded.
Secondary endpoint was treatment response 6 months after sorafenib initiation and overall survival.
Computed tomography (CT) was performed at baseline, before each TACE cycle, and 6 months after sorafenib initiation as recommended by Lencioni and Llovet [27]. Thereafter, routine CT was performed every 3 months. Response evaluation was performed according to modified response evaluation criteria in solid tumours (mRECIST) [27, 28]. Complete response (CR) reflected the disappearance of any intratumoral arterial enhancement of all target lesions. Partial response (PR) was at least 30% decrease in the sum of diameters of viable (enhancement in the arterial phase) target lesions, taking as a reference the baseline sum of the diameters of target lesions. Stable disease (SD) was defined as any cases not qualifying for either PR or progressive disease (PD). PD was an increase of at least 20% in the sum of the diameters of viable target lesions recorded since treatment started.
Statistics
All patients who received at least one dose of sorafenib were included in the safety assessments. Adverse events and serious adverse events were summarised by NCI-CTC severity and relationship to study treatment for each baseline bilirubin level subgroup (<1.5 versus ≥1.5 mg/dL) using descriptive statistics.
All patients who completed the 6-month study were included in the response analysis. Survival curves were calculated for all patients using Kaplan–Meier methods. The median overall survival was calculated together with the 95% confidence interval (CI), with survival defined as the time from sorafenib initiation until death from any cause. Median overall survival and 1-year survival were calculated for certain patient subgroups (BCLC stage, Child–Pugh liver function, baseline bilirubin levels) in post hoc analyses. Differences in overall survival between subgroups were evaluated using a log rank test.
Results
Demographics
Between October 2008 and June 2010, 17 patients were screened and 15 patients were included. Reasons for exclusion were impossibility of TACE due to intrahepatic arteriovenous shunts (n = 1) or massive bilobular tumour load (n = 1).
All 15 patients received sorafenib at the standard dose (400 mg bid), and remained on therapy for a median of 5.2 months (95% CI: 2.6–7.4 months). Seven patients continued sorafenib treatment after the 6-month study period. All patients received at least one TACE session and, overall, 37 TACE sessions were performed. The median number of TACE sessions was 3 (range 1–4), with a median cumulative doxorubicin dose of 183 mg (range 59–395 mg) per patient. The median doxorubicin dose (mg) of the TACE sessions 1/2/3/4 (n = 15/13/8/1) was 75 (range 13–153)/72 (range 18–122)/74 (range 18–107)/137.
The baseline characteristics and a treatment overview are provided in Tables 1 and 2.
Safety
Laboratory values of all patients during the 6 months study period are given in Fig. 2a–e. Adverse events reported during the study are shown in Table 3. All patients experienced at least one adverse event. The most common adverse events (any grade) were abdominal pain (n = 14), weight loss (n = 13), alopecia (n = 12), fatigue (n = 12) and hyperbilirubinaemia (n = 11). A total of 32 serious adverse events (grade ≥3) were reported, most commonly leukopaenia, thrombocytopaenia, anorexia, abdominal pain and ascites (all n = 3). Grade 4/5 adverse events occurred more frequently in patients with baseline bilirubin levels <1.5 mg/dL versus those with baseline bilirubin levels ≥1.5 mg/dL (9 versus 2, respectively).
The most common sorafenib-related adverse events were weight loss (n = 13), fatigue (n = 12), anorexia (n = 10), diarrhoea (n = 7) and hand–foot–skin reaction (HFSR, n = 4). Twelve patients (80%) underwent sorafenib dose reduction to 200 mg bid due to sorafenib-related adverse events (HFSR, n = 2; rash, n = 2; diarrhoea, n = 2; anorexia, n = 2; dizziness, n = 1; neutropaenic fever, n = 1; abdominal pain, n = 1; deterioration of general condition to ECOG PS ≥3, n = 1), and in 5 patients (33%) sorafenib was discontinued permanently owing to clinical deterioration (ECOG PS ≥3).
Abdominal pain was the most common TACE-related adverse event. Serious adverse events clearly related to synergistic effects of combination treatment included alopecia and grade 4 febrile neutropaenia, which occurred in 3 of the first 8 patients included in this study.
Febrile neutropaenia presented 2–4 weeks after TACE following the first TACE session (n = 2) or the second TACE session (n = 1). These patients received 99, 153 and 141 mg of doxorubicin (depending on serum bilirubin levels), respectively, during the TACE session preceding the event. Consequently, doxorubicin doses were reduced by 25% for each bilirubin-adjusted dose level in all subsequent patients. Thereafter, no further febrile neutropaenia was observed.
Six patients experienced a total of 10 unscheduled hospital admissions because of serious adverse events: 1 was associated with sorafenib (dehydration), whereas 9 admissions in 6 patients were considered TACE-related. These serious adverse events included acute renal failure (n = 1), hepatic decompensation (n = 4), febrile neutropaenia (n = 2) (the third event of febrile neutropaenia occurred during a hospital admission), cholangitis (n = 1) and severe liver dysfunction with hypoglycaemia (n = 1). Three unscheduled admissions resulted in the patient’s death, while improvement with consequent discharge from hospital was observed in 7 cases.
Overall, 10 patients died, 5 during the 6-month study period (cholangitis, n = 1; liver failure, n = 2; variceal bleeding, n = 1; rapid deterioration to ECOG-PS 4, n = 1). All but one death (variceal bleeding) were considered TACE-related. At baseline, the 5 patients who died during the first 6 months had an ECOG-PS of 0, were in Child–Pugh stage A (n = 3) or B (n = 2), and had BCLC-B (n = 4) or -C (n = 1) stage disease.
In June 2010, after the death of the 15th included subject, we performed an unplanned interim safety analysis. Owing to the adverse events observed and significantly shorter survival in our study compared with published data [10], we stopped the study for ethical reasons.
Response and survival
Ten patients (67%) were alive 6 months after the start of sorafenib treatment and eligible for response analysis (Table 4). Two patients achieved CR, 5 had a PR, and 1 patient had SD for 6 months after sorafenib initiation. Two patients had PD.
Median overall survival was 10.6 months (95% CI: 5.2–16 months) for all patients (n = 15, Fig. 3). The median overall survival for patients with BCLC stage A/B who also had Child–Pugh stage A cirrhosis (n = 7) was 17.6 months, 95% CI 3.8–31.4 months. Interestingly, patients with baseline bilirubin levels ≥1.5 mg/dL (n = 6) lived almost twice as long as those with baseline bilirubin levels <1.5 mg/dL (n = 9; median overall survival: 20.5 vs. 10.4 months, respectively, P = 0.086).
Discussion
This is the first pilot study to evaluate the safety of TACE with bilirubin-adjusted doxorubicin doses in combination with sorafenib in patients with HCC. This study was terminated prematurely because of safety concerns.
The incidence of some adverse events observed in our study (Table 3), such as HFSR (27%), rash (20%), and diarrhoea (47%) were similar to those reported with sorafenib as monotherapy [11, 29], and in a Phase I study of TACE in combination with sorafenib [19]. However, we observed more anorexia (67% vs. 29%), weight loss (87% vs. 30%), alopecia (80% vs. 14%), fatigue (80% vs. 46%) and abdominal pain (93% vs. 31%) than reported with sorafenib monotherapy in the Phase III SHARP study [11] indicating a negative synergism with TACE in this study. With the exception of weight loss (71%), the incidence of these adverse events was also reported to be lower by Dufour et al [19].
Of even more concern, we observed a 47% incidence of neutropaenia and three cases (20%) of febrile neutropaenia. Febrile neutropaenia was not reported by Dufour et al [19] who used a similar TACE schedule but lower doxorubicin doses and has not been observed in any sorafenib monotherapy [11, 12, 29] or TACE study [25]. Furthermore, our findings of neutropaenia are contrary to those from the second interim analysis of START, an ongoing Phase II study evaluating TACE (doxorubicin: 30–60 mg) in combination with continuous sorafenib with interruptions 4 days before and after TACE in patients with intermediate stage HCC, where only 8 cases of neutropaenia have been reported [20].
Therefore, the adverse events observed here could happen because of the high doxorubicin dose used. The concomitant administration of doxorubicin and sorafenib affects the pharmacokinetics of doxorubicin, with an approximately 21% increase in the area under the curve reported for doxorubicin [30]. An increase in adverse events, particularly (febrile) neutropaenia, has also been reported in studies combining systemic doxorubicin at 60 mg/m2 with sorafenib [13, 30]. In a randomised Phase II study of systemic doxorubicin (60 mg/m2) in combination with sorafenib or placebo in patients with advanced HCC and Child–Pugh stage A cirrhosis, neutropaenia was reported in 38% of patients in the sorafenib group compared with 31% in the placebo group [13].
The better tolerability observed in the Phase I study by Dufour et al [19] and in the START trial [20] may, at least in part, be attributable to the lower dose of doxorubicin used.
In our study, following a 25% reduction in doxorubicin dose at each bilirubin-adjusted dose level, no more febrile neutropaenia was observed, although the synergism between doxorubicin and sorafenib with regard to other adverse events remained unchanged.
Overall, 9 out of 10 unscheduled hospital admissions, mostly due to liver-related adverse events, and 4 of the 5 deaths within the 6-month study period were considered TACE-related. These findings are thought to be mainly attributed to the bilirubin-adjusted doxorubicin dosing used, as patients with bilirubin levels <1.5 mg/dL at baseline received a 1.5-fold higher cumulative doxorubicin dose than those with baseline bilirubin levels ≥1.5 mg/dL (mean doxorubicin dose: 219 mg vs. 147 mg, respectively). This could explain the somewhat surprising and paradoxical survival results, as there was a clear trend towards shorter median overall survival among patients with baseline bilirubin levels <1.5 mg/dL compared with those with bilirubin levels ≥1.5 mg/dL.
Given the significant systemic toxicity of doxorubicin in our study, one can assume that conventional TACE with lipiodol and bilirubin adjusted doxorubicin dosing is not the optimal choice for combination with sorafenib. Recently, TACE performed with drug eluting beads (DEB-TACE) showed a better safety profile than conventional TACE with lipiodol and doxorubicin [31]. This observation can primarily be attributed to lower systemic doxorubicin concentrations after the procedure [32]. Thus, future trials combining TACE and sorafenib should be rather performed with DEB-TACE than with lipiodol-TACE.
Additionally, there is considerable heterogeneity between TACE regimens in terms of intervals between sessions (between 1 and 6 months) [33–36]. The high rate of serious adverse events in this study may therefore also be explained by the intensive TACE schedule we employed [7].
Taken together, the study regimens of those trials reporting better safety outcomes than our study differ from the regimen of our study to such an extent that our regimen cannot be favoured for future clinical trials.
Finally, it is clear that TACE is most effective in a highly selected patient population [10]. Indeed, the median overall survival of BCLC-B patients with Child–Pugh stage A cirrhosis and ECOG-PS of 0 was 17.6 months in our study. However, the median overall survival for our overall population (10.6 months) was similar to that of the SHARP study (10.7 months) [11], which included patients with advanced disease (BCLC-C), suggesting that the combination of an aggressive TACE regimen with sorafenib was detrimental to some patients in this study. Two of the five deaths during the 6-month study period had Child–Pugh B cirrhosis at baseline, which also indicates that these patients were suboptimal candidates for TACE in combination with sorafenib.
The small number of patients, especially in some subgroups is the main limitation of this study. Additionally, radiologic tumour response determined by CT in this trial has to be interpreted with caution as a recent study [37] demonstrated superiority of MRI to CT for the detection of viable tumour residuals after lipiodol based TACE.
In summary, the safety results of our study do not support the use of this intensive, high-dose doxorubicin-based TACE regimen in combination with sorafenib in the population studied. However, in a carefully selected, intermediate-stage patient population (BCLC-B), the combination of sorafenib with TACE may result in improved clinical outcomes. Especially the use of DEB-TACE may be associated with less systemic doxorubicin absorption [32] and therefore a better toxicity profile in combination with sorafenib. These strategies are currently being investigated in Phase II and III studies [20, 22] and final efficacy and safety findings from these studies are eagerly awaited.
References
Parkin DM, Bray F, Ferlay J et al (2005) Global cancer statistics 2002. CA Cancer J Clin 55:74–108
Hucke F, Sieghart W, Schöniger-Hekele M, Peck-Radosavljevic M, Müller CC (2011) Clinical characteristics of patients with hepatocellular carcinoma in Austria—is there a need for a structured screening program? Wien Klin Wochenschr 123:542–551
Peck-Radosavljevic M, Sieghart W, Kölblinger C et al (2011) Austrian Joint ÖGGH-ÖGIR-ÖGHO-ASSO position statement on the use of transarterial chemoembolization (TACE) in hepatocellular carcinoma. Wien Klin Wochenschr. doi:10.1007/s00508-011-0056-2
Bruix J, Sherman M, Llovet JM et al (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 35:421–430
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Llovet JM, Brú C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19:329–438
Raoul JL, Sangro B, Forner A et al (2011) Evolving strategies for the management of intermediate-stage hepatocellular carcinoma: available evidence and expert opinion on the use of transarterial chemoembolization. Cancer Treat Rev 37:212–220
Llovet JM, Real MI, Montaña X et al (2002) Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 359:1734–1739
Lo CM, Ngan H, Tso WK et al (2002) Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35:1164–1171
Llovet JM, Bruix J (2003) Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 37:429–442
Llovet JM, Ricci S, Mazzaferro V et al (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359:378–390
Cheng AL, Kang YK, Chen Z et al (2009) Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 10:25–34
Abou-Alfa GK, Johnson P, Knox JJ et al (2010) Doxorubicin plus sorafenib vs doxorubicin alone in patients with advanced hepatocellular carcinoma: a randomized trial. JAMA 304:2154–2160
Wilhelm S, Carter C, Lynch M et al (2006) Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Nat Rev Drug Discov 5:835–844
Wilhelm SM, Adnane L, Newell P et al (2008) Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol Cancer Ther 7:3129–3140
Liu L, Cao Y, Chen C et al (2006) Sorafenib blocks the RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer Res 66:11851–11858
Sergio A, Cristofori C, Cardin R et al (2008) Transcatheter arterial chemoembolization (TACE) in hepatocellular carcinoma (HCC): the role of angiogenesis and invasiveness. Am J Gastroenterol 103:914–921
Li X, Feng GS, Zheng CS et al (2004) Expression of plasma vascular endothelial growth factor in patients with hepatocellular carcinoma and effect of transcatheter arterial chemoembolization therapy on plasma vascular endothelial growth factor level. World J Gastroenterol 10:2878–2882
Dufour JF, Hoppe H, Heim MH et al (2010) Continuous administration of sorafenib in combination with transarterial chemoembolization in patients with hepatocellular carcinoma: results of a phase I study. Oncologist 15:1198–1204
Chung Y, Kim B, Chen C et al (2010) Study in Asia of the combination of transcatheter arterial chemoembolization (TACE) with sorafenib in patients with hepatocellular carcinoma (HCC) trial (START): second interim safety and efficacy analysis. J Clin Oncol 28:Abstract 4026.
Erhardt A, Kolligs FT, Dollinger MM et al (2009) First-in-men demonstration of sorafenib plus TACE for the treatment of advanced hepatocellular carcinoma (SOCRATES trial). Hepatology 50:Abstract 1675.
Reyes D, Azad N, Koteish A et al (2010) Phase II trial of sorafenib combined with doxorubicin eluting bead-transarterial chemoembolization for patients with unresectable hepatocellular carcinoma: Interim safety analysis. SIR S56:Abstract 141.
Reyes DK, Azad NS, Koteich A et al (2010) Phase II trial of sorafenib combined with doxorubicin-eluting bead transarterial chemoembolization (DEB-TACE) for patients with unresectable hepatocellular carcinoma (HCC): interim safety and efficacy analysis. Presented at American Society of Clinical Oncology Gastrointestinal Cancers Symposium: Abstract 254.
Strebel BM, Dufour JF (2008) Combined approach to hepatocellular carcinoma: a new treatment concept for nonresectable disease. Expert Rev Anticancer Ther 8:1743–1749
Marelli L, Stigliano R, Triantos C et al (2007) Transarterial therapy for hepatocellular carcinoma: which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc Intervent Radiol 30:6–25
Peck-Radosavljevic M, Greten TF, Lammer J et al (2010) Consensus on the current use of sorafenib for the treatment of hepatocellular carcinoma. Eur J Gastroenterol Hepatol 22:391–398
Llovet JM, Di Bisceglie AM, Bruix J et al (2008) Design and endpoints of clinical trials in hepatocellular carcinoma. J Natl Cancer Inst 100:698–711
Lencioni R, Llovet JM (2010) Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 30:52–60
Abou-Alfa GK, Schwartz L, Ricci S et al (2006) Phase II study of sorafenib in patients with advanced hepatocellular carcinoma. J Clin Oncol 24:4293–4300
Richly H, Schultheis B, Adamietz IA et al (2009) Combination of sorafenib and doxorubicin in patients with advanced hepatocellular carcinoma: results from a phase I extension trial. Eur J Cancer 45:579–587
Lammer J, Malagari K, Vogl T et al (2009) Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc Intervent Radiol 33:41–52
Varela M, Real MI, Burrel M et al (2007) Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J Hepatol 46:474–481
Vogl TJ, Trapp M, Schroeder H et al (2000) Transarterial chemoembolization for hepatocellular carcinoma: volumetric and morphologic CT criteria for assessment of prognosis and therapeutic success-results from a liver transplantation center. Radiology 214:349–357
Saccheri S, Lovaria A, Sangiovanni A et al (2002) Segmental transcatheter arterial chemoembolization treatment in patients with cirrhosis and inoperable hepatocellular carcinomas. J Vasc Interv Radiol 13:995–999
Grieco A, Marcoccia S, Miele L et al (2003) Transarterial chemoembolization (TACE) for unresectable hepatocellular carcinoma in cirrhotics: functional hepatic reserve and survival. Hepatogastroenterology 50:207–212
Farinati F, De Maria N, Marafin C et al (1996) Unresectable hepatocellular carcinoma in cirrhosis: survival, prognostic factors, and unexpected side effects after transcatheter arterial chemoembolization. Dig Dis Sci 41:2332–2339
Kloeckner R, Otto G, Biesterfeld S, Oberholzer K, Dueber C, Pitton MB (2010) MDCT versus MRI assessment of tumor response after transarterial chemoembolization for the treatment of hepatocellular carcinoma. Cardiovasc Intervent Radiol 33:532–540
Acknowledgements
Dr M. Peck-Radosavljevic is an investigator, advisor and speaker for Bayer Schering Pharma. This publication was supported by Bayer Schering Pharma AG through the funding of editorial assistance during the finalisation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sieghart, W., Pinter, M., Reisegger, M. et al. Conventional transarterial chemoembolisation in combination with sorafenib for patients with hepatocellular carcinoma: a pilot study. Eur Radiol 22, 1214–1223 (2012). https://doi.org/10.1007/s00330-011-2368-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2368-z