Abstract
Objective
To investigate the role of perfusion defect (PD) size on dual energy CT pulmonary blood volume assessment as predictor of right heart strain and patient outcome and its correlation with d-dimer levels in acute pulmonary embolism (PE).
Methods
53 patients with acute PE who underwent DECT pulmonary angiography were retrospectively analyzed. Pulmonary PD size caused by PE was measured on DE iodine maps and quantified absolutely (VolPD) and relatively to the total lung volume (RelPD). Signs of right heart strain (RHS) on CT were determined. Information on d-dimer levels and readmission for recurrent onset of PE and death was collected.
Results
D-dimer level was mildly (r = 0.43–0.47) correlated with PD size. Patients with RHS had significantly higher VolPD (215 vs. 73 ml) and RelPD (9.9 vs. 2.9%) than patients without RHS (p < 0.003). There were 2 deaths and 1 readmission due of PE in 18 patients with >5% RelPD, while no such events were found for patients with <5% RelPD.
Conclusion
Pulmonary blood volume on DECT in acute PE correlates with RHS and appears to be a predictor of patient outcome in this pilot study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary embolism (PE) may cause pulmonary vascular obstruction and consecutive perfusion defects (PD) of the lung parenchyma. In severe cases, extensive vascular obstruction leads to right heart strain (RHS) with dysfunction and finally death [1]. Several studies on ventilation/perfusion scintigraphy reported that patients with RHS had larger perfusion defects and a worse clinical outcome than patients with normal right ventricular function after PE [2].
These days, pulmonary CT angiography (CTPA) with thin-collimation multi-slice CT systems has been accepted as the frontline imaging technique for the diagnosis of PE [3–6] by visualizing the thrombus, measuring vascular obstruction score and right ventricular–to–left ventricular (RV/LV) diameter ratio as a CT marker of RHS. Correlation between the severity of PE and the incidence of fatal outcome has been demonstrated in several studies [7–11]. However, so far only static, morphological parameters have been used for determining PE severity on CT imaging, whereas the degree of functional obstruction of lung perfusion has been recognized [2, 12–14] as an important clinical predictor of patient outcome.
With the recent introduction of dual source dual energy CT (DECT) in 2006, evaluation of PE with CT has entered a new age. By making use of the unique spectral behaviour of iodine at higher and lower photon energies [15, 16], DECT allows both, the display of iodine distribution maps as a measure of the pulmonary microcirculation for the assessment of pulmonary blood volume, and the evaluation of standard thin-section CTA images. Several studies have proven the feasibility of this new technique to display areas of reduced pulmonary blood volume referred to as “perfusion defects” due to occlusive PE and have shown a good correlation between DECT and scintigraphic findings [17–22], and between CTA obstruction/perfusion defect score and RV/LV diameter ratio [23, 24]. To our knowledge no data about the clinical impact of absolute PD size as measured on dual energy iodine distribution maps is available.
Thus, the purpose of this study was to retrospectively investigate the role of perfusion defect size on dual energy CT pulmonary blood volume assessment as predictor of right heart strain and patient outcome and its correlation with d-dimer levels in acute pulmonary embolism.
Materials & methods
Patient population
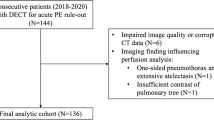
The data of this study was retrospectively acquired from patients that underwent dual source dual energy pulmonary CT angiography (CTPA) in our department (Somatom Definition and Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany), because of clinical suspicion of acute PE between May 2008 and June 2010. Patients were identified by a search in the RIS/PACS system of our department. Acute PE was diagnosed in 53 of totally 353 referred patients (34 on the Definition and 19 on the Flash). Information on CT signs of right heart strain, d-dimer levels and patient outcome was collected in these patients as well as in a control group of 53 patients who were randomly selected from the cohort of 300 patients in whom PE was excluded by CTPA. The ethics committee of our hospital approved this study. Informed patient consent was not required.
CT protocol
Dual energy CTPA was performed according to the protocols shown in Table 1. By technical restrictions, the field of view of the B detector was limited to 26 cm with the Definition and to 32 cm with the Flash with a field of view of 50 cm on the A detector. Contrast enhancement was achieved with 60 ml of contrast material (Imeron 400 mg/ml, Bracco, Konstanz, Germany) followed by a 100 ml saline chaser bolus injected at 4 ml/s. Bolus tracking was used for automated examination start with a delay of 7 s when a trigger threshold of 100 HU in the pulmonary trunk was reached. Three CTPA images series are routinely reconstructed from the dual energy data: One series each for 80 kV, 140 kV, and one weighted average series combining data from the high and low kV series in a way to create the image impression of a regular 120 kV CT examination (Definition: 70% of the 140 kV and 30% of the 80 kV data; Flash: 60% of the 140 kV + SN filter and 40% of the 80 kV data). Diagnosis of PE was made on the virtual 120 kV images during clinical routine read out on a PACS workstation. Re-assessment of CTPA data for this study did not reveal one single case of missed PE.
Perfusion analysis and data collection
Both, the high and low kV data set were loaded simultaneously into dedicated postprocessing software (LungPBV, Syngo Dual Energy, Siemens Healthcare). Pulmonary blood volume was evaluated with the help of colour-coded iodine distribution maps of the lung parenchyma as previously described [17–22, 24]. Perfusion defects caused by PE typically appear as wedge-shaped marginal areas with reduced iodine content compared to surrounding lung tissue [22] (Fig. 1). To exclude other causes for PD related to pathologies of the lung parenchyma, e.g. infiltration or emphysema, blood volume maps were not only compared to CTPA findings but also to the lung anatomy as assessed in lung window (width: 1,200 HU, centre: −500 HU). PD size was quantified absolutely (VolPD in ml) and relatively to the total lung volume (RelPD in%). The total lung volume was calculated automatically with dedicated software (Lung Parenchyma Analysis, Syngo InSpace, Siemens Healthcare). PD volume was measured by manual slice segmentation by one radiologist with 4 years of experience in chest CT and 3 years of experience in DECT imaging (Fig. 1). Further, the diameter ratio of the right and left ventricle (RV/LV) was determined in multiplanar reformations (MPR) in cardiac 4-chamber view (Syngo 3D, Siemens) by a second independent radiologist with 5 years of experience in chest and cardiac CT who was unaware of the pulmonary blood volume status. A ratio of RV:LV >1 indicated the presence of right heart strain. Electronic patient files of our hospital were searched for echocardiography reports, d-dimer levels taken at the time of admission for acute PE and information on readmission for recurrent onset of PE, death and underlying diseases. Further, patients or their family practitioners, respectively, were contacted by telephone to see if the patients were still alive, to ask if another event of PE had occurred after initial diagnosis and treatment of PE in our hospital, and to ask for the cause of death if the patient had deceased. All data was collected in September 2010 to ensure at least a follow-up period of 3 months since inclusion of the last patient in June 2010.
Pulmonary blood volume assessment. (a) displays a regular grey scale CT pulmonary angiographic image fused with the dual energy pulmonary iodine distribution map. The white arrows are pointing to extensive bilateral pulmonary emboli leading to a reduced blood volume (also referred to as perfusion defects) further distally in their supply territory marked with white stars. Lung window assessment (b) does not show any segmental parenchymal pathology that may mimic a wedge-shaped perfusion defect. (c) Perfusion defect size was measured by manual slice segmentation using a free-hand region of interest tool
Statistical analysis
Statistical analysis was performed using dedicated software (BiAS 9.06 for Windows, Epsilon Verlag, Frankfurt, Germany). Correlations between perfusion defect size (VolPD and RelPD) and d-dimer levels was evaluated using Pearson’s correlation. The Wilcoxon-Mann-Whitney-U-test was used to analyse difference in perfusion defect size between patients with and without right heart strain. Survival time in months was calculated using the Kaplan-Meier method, and relative hazard ratios for death with 95% confidence intervals were determined. Comparisons between patient cohorts were made using the log-rank test. Survival data from patients who were alive at the time of follow-up (i.e. September 2010) were censored. In all tests a p-value of less than 0.05 was considered to indicate statistically significant differences.
Results
CT examinations and calculation of perfusion images were performed successfully for all 53 subjects with PE. Forty patients had 100% coverage of the lung volume within the dual energy FOV. While no coverage loss was observed in the Flash group, in 12 patients who underwent CTPA on the Somatom Definition small peripheral lung areas were not fully covered within the dual energy FOV (n = 8 with <5% and n = 5 with 5–10% of the total lung volume). No volume corrections were applied in these cases. Absolute PD size (VolPD) ranged between 5.8 and 748.4 ml (median: 97.2 ml), relative PD size (RelPD) between 0.2 and 22.9% (median: 3.1%).
D-dimer levels were weakly correlated with VolPD (r = 0.47, p = 0.001) and RelPD (r = 0.43, p = 0.003). Patients with RHS (n = 17) had significantly greater VolPD (median 215.4 ml vs. 73.3 ml; p = 0.003) and RelPD (median 9.9% vs. 2.9%; p < 0.001) than patients without RHS (n = 36) (Table 2). CT findings of RHS were consistent with echocardiographic findings in 100% of the cases. In the following, patients were further divided according to their relative perfusion defect size in three subgroups (Table 3):
-
a)
Eighteen patients showed a RelPD of more than 5%. The following risk factors for PE were found: malignant neoplasm (n = 9 patients), surgery (n = 3), coagulopathy (n = 2), oral contraception with long distance flight (n = 2), no identifiable risk factors (n = 2). One patient was readmitted to our hospital because of recurrent PE due to surgery 10 months after diagnosis of the first PE with a RelPD size of 8.9%. The patient was still alive 4 months after this second event. Seven patients died of this group, of whom four showed RHS. Two patients died because of PE: one patient 4 days after diagnosis of PE with a RelPD size of 11.1% and signs of RHS. The other patient died two 2 months after the first PE event with a RelPD size of 14.3% and no signs of RHS due to recurrent PE in another hospital. Both patients suffered from cancer as their underlying disease (neuroendocrine carcinoma and NSCLC). Six patients were lost to follow-up at the time of data collection for this study. Based on information from our electronic patient file system, survival could be assured until 1, 1, 2.5, 3, 4, and 7 months after initial diagnosis of PE and was censored at these time points.
-
b)
Sixteen patients showed a RelPD between 2.5 and 5%. The following risk factors for PE were found: malignant neoplasm (n = 5 patients), surgery (n = 2), oral contraception combined with long distance flight (n = 4), no identifiable risk factors (n = 5). None of these patients was readmitted or died due to recurrent PE. However, one patient died due to his underlying end-stage cancer disease. Two patients were lost to follow-up. Survival could be assured until 4 and 8.5 months after initial diagnosis of PE and was censored at that time point.
-
c)
Nineteen patients showed a RelPD of less than 2.5%. The following risk factors for PE were found: surgery (n = 4 patients), coagulopathy (n = 2), long distance flight (n = 1), malignant neoplasm (n = 1), no identifiable risk factors (n = 11). Four patients died from this group, one showed RHS. However, no patient was readmitted or died due to recurrent PE. Patients died because of their underlying diseases (n = end-stage cancer, n = 1 multi-organ failure after coronary bypass surgery, n = 1 end-stage COPD). For one patient, no follow-up data could be generated after discharge from our hospital, thus survival time was censored at 1 month after initial diagnosis of PE.
Log-rank testing revealed a significantly shorter survival time for group 1 compared to group 2 (p = 0.008) while no such difference was observed comparing group 1 and 3 (p = 0.17) and group 2 and 3 (p = 0.18) (Table 3). The relative hazard ratio for death was increased by factor 10.0 (95% CI: 1.8–54.5) between group 1 and 2 and by factor 2.3 (95% CI: 0.7–7.6) between group 1 and 3. If data from group 2 and 3 is pooled, a relative hazard ratio of 3.7 (95% CI: 1.3–10.9) for group 1 is calculated. Comparing patients with right heart strain to those without, there was no significant difference in survival (p = 0.15) (Table 2). The relative hazard ratio for death was increased by the factor 2.3 (95% CI: 0.7–6.8) in patients with RHS. In a Cox regression model, RelPD size was the strongest predictor of survival time followed by RHS, VolPD size and d-dimer level.
When we look at the control group, we did not observe significant differences in age (median: 58, range: 26–88 years vs. median: 66, range 21–97 years; p = 0.3) and gender distribution compared to the study group (29 vs. 23 male; p = 0.33 with Fisher’s test). The following risk factors for PE were found: immobilisation (n = 13), cancer (n = 12 patients), acute infections (n = 7), deep vein thrombosis of the lower leg (n = 3), surgery (n = 2), no identifiable risk factors (n = 16). Four patients were lost to follow-up; survival could be ensured up to 0.5, 0.5, 1 and 2.5 months and was censored at that time. Another four patients died due to their underlying disease (n = 3 due to cancer, n = 1 after heart transplantation). No patient died of PE or had a recurrent event of suspected PE. Two patients had CT signs of RHS which were confirmed on echocardiography. D-dimer levels were significantly lower in the control group compared to patients with PE (median: 1.5, range: 0.22–10 μg/ml vs. median: 6.5, range: 0.28–20 μg/ml; p < 0.001). The median survival time was >3 months (mean: 22.9, range: 0.5–25 months) and therewith significantly longer (p = 0.037) than pooled data of all patients with PE (median: >7 months, mean: 17.8 months, range: 0–24 months) (Fig. 2). It was further significantly longer than the survival time of patients with >5% RelPD (p = 0.0006) but with no difference compared to patients with <5% RelPD (median: >4, mean: 20.3, range: 1–24 months, p = 0.77) (Fig. 2). The relative hazard ratio for death was increased by factor 6.5 (95% CI: 2.3–18.2) in patients with >5% RelPD and by factor 3.1 (95% CI: 1.1–9.1) in patients with PE regardless of PD size compared to the control group.
Survival analysis. (a) displays a Kaplan-Meier curve comparing survival data from patients with pulmonary embolism (PE) and >5% RelPD size (1), <5% RelPD size (2) and patients from the control group without PE (3). Median survival was significantly (p = 0.0006) longer in group 2 (>4 months) and 3 (>3 months) compared to group 1 (4.6 months), but without such a difference between group 2 and 3 (p = 0.77). (b) compares survival data of patients without (2) and patients with (1) PE. Survival in group 2 (>3 months) was significantly (p = 0.037) longer than in group 1 (>7 months)
Discussion
The feasibility of DECT to display perfusion defects in the pulmonary blood volume caused by PE has been proven in several studies [17–22]. With DECT information on intravascular thrombi, right heart strain and pulmonary blood volume is available from one single CT acquisition with superior spatial resolution compared to planar or SPECT ventilation/perfusion scintigraphy. From studies on ventilation/perfusion scintigraphy in acute PE a certain impact of PD size on restoration of pulmonary flow [12, 14], early death [13] and right heart strain [2] is known. However, in all nuclear medicine studies known to the authors PD was quantified by a reference chart only and the exact volume of PD was not actually measured objectively and absolutely.
We found a wide range of absolute (VolPD) and relative PD size (RelPD) ranging between 5.8 and 748.4 ml and 0.2–22.9%, respectively. There was a weak but significant positive correlation between d-dimer levels and PD size, revealing an increase in PD size with an increase in d-dimers as a surrogate parameter of PE severity. The level of d-dimers has been shown to correlate with right heart dysfunction and clot burden as well as to be a negative outcome predictor, since short and long term survival after acute PE is limited with increasing d-dimer levels [25–30]. However, keeping in mind the low specificity of this test, the mean d-dimer level was also slightly elevated in the control group without PE, but it was significantly lower than in patients with PE.
Further, acute cor pulmonale is known as a negative outcome predictor for PE, as right ventricular dysfunction may progress to its failure and circulatory collapse. Patients who died of PE had a significant higher RV/LV diameter ratio [11, 31, 32], which is an accurate CT sign for the presence of RHS. Chae et al. [23] and Zhang et al. [24] reported good correlation between RV/LV diameter ratio with a novel self-defined dual energy perfusion score or the number of pulmonary segments with perfusion defects, respectively. Our results acknowledge their findings, as RHS in our cohort went along with a significantly greater PD size. In contradiction to Kjaergard et al. [33], who reported a correlation between right heart strain and a minimum of 25% loss of lung perfusion on perfusion scintigraphy, we assessed RHS at an average loss of 215.4 ml VolPD and 9.9% RelPD, thus indicating that even relatively small reductions of pulmonary blood volume may lead to RHS and put the patient at risk.
Chae et al. suggested DECT perfusion maps to be a possible surrogate marker for RHS. Together with the results of our study we can confirm that PD size can be seen as marker for RHS and it might even be an additional instrument for prognostic evaluation in PE itself. When we look at the incidence of readmission and death due to PE, we found these major hard endpoints only in patients with a relative PD size of >5% of the total lung volume, whereas no such event was recorded for patients with <5% RelPD. Only one of these patients who died showed signs of RHS, and we did not observe a significant difference in overall survival time between patients with and without RHS. Median survival time, however, was significantly lower for patients with >5% RelPD at an increased relative hazard ratio for death compared to patients with less than 5% RelPD or the control group without PE. Further, after Cox regression analysis RelPD was the most important predictor of survival time followed by RHS. These findings may underline the importance of the integrity of pulmonary microvasculature on patient outcome, factors that have been described as outcome predictors years ago for ventilation/perfusion scintigraphy [12–14]. However, meanwhile they have been largely forgotten, as morphologic imaging with MDCT has taken over the leading role in the diagnosis of PE from functional imaging with scintigraphy. By displaying the morphologic proof of PE and RHS combined with functional information on pulmonary blood volume status, DECT may be able to close the gap between these two philosophies and provide the best of both modalities.
We acknowledge the following study limitations, which may limit the generalization of our results: First, because of the smaller B detector and therefore limitation of the dual energy FOV to 26 cm, the very peripheral areas of some patients’ lungs were not fully covered. Therefore, absolute and relative PD measurements may not reflect the whole extent of PD. Second, we did not compare our results to scintigraphy which is currently referred as the gold standard method for lung perfusion analysis. Third, and most important, the data collection was retrospective in nature. The patient population was small, very heterogeneous in terms of underlying risk factors and diseases, and there was the very small number of only one case of readmission and two cases of death due to PE. As for totally nine patients no long-term follow-up data after discharge from our hospital could be completed, patients with recurrent PE or PE-related death may have been missed. Especially the very small number of PE-related deaths with a relatively large number of deaths due to other reasons may cut down the clinical significance of our observations.
Acknowledging the above mentioned limitations, our initial data suggest that pulmonary blood volume as assessed on DECT may be considered as a negative outcome predictor in acute PE. Prospective trials are mandatory to further elucidate the role of that finding and to show, if it has even incremental value over right heart strain.
References
Lualdi JC, Goldhaber SZ (1995) Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. Am Heart J 130:1276–1282
Wolfe MW, Lee RT, Feldstein ML, Parker JA, Come PC, Goldhaber SZ (1994) Prognostic significance of right ventricular hypokinesis and perfusion lung scan defects in pulmonary embolism. Am Heart J 127:1371–1375
Remy-Jardin M, Pistolesi M, Goodman LR, Gefter WB, Gottschalk A, Mayo JR, Sostman HD (2007) Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology 245:315–329
Schoepf UJ, Costello P (2004) CT angiography for diagnosis of pulmonary embolism: state of the art. Radiology 230:329–337
Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV, Popovich J, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK (2006) Multidetector computed tomography for acute pulmonary embolism. N Engl J Med 354:2317–2327
Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galie N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Zamorano JL, Andreotti F, Ascherman M, Athanassopoulos G, De Sutter J, Fitzmaurice D, Forster T, Heras M, Jondeau G, Kjeldsen K, Knuuti J, Lang I, Lenzen M, Lopez-Sendon J, Nihoyannopoulos P, Perez Isla L, Schwehr U, Torraca L, Vachiery JL (2008) Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J 29:2276–2315
Araoz PA, Gotway MB, Trowbridge RL, Bailey RA, Auerbach AD, Reddy GP, Dawn SK, Webb WR, Higgins CB (2003) Helical CT pulmonary angiography predictors of in-hospital morbidity and mortality in patients with acute pulmonary embolism. J Thorac Imaging 18:207–216
Collomb D, Paramelle PJ, Calaque O, Bosson JL, Vanzetto G, Barnoud D, Pison C, Coulomb C, Ferettis G (2003) Severity assessment of acute pulmonary embolism: evaluation using helical CT. Eur Radiol 13:1508–1514
Ghaye B, Ghuysen A, Bruyere PJ, D’Orio V, Dondelinger RF (2006) Can CT pulmonary angiography allow assessment of severity and prognosis in patients presenting with pulmonary embolism? What the radiologist needs to know. Radiographics 26:23–39, discussion 39–40
Ghaye B, Ghuysen A, Willems V, Lambermont B, Gerard P, D’Orio V, Gevenois PA, Dondelinger RF (2006) Severe pulmonary embolism: pulmonary artery clot load scores and cardiovascular parameters as predictors of mortality. Radiology 239:884–891
van der Meer RW, Pattynama PM, van Strijen MJ, van den Berg-Huijsmans AA, Hartmann IJ, Putter H, de Roos A, Husiman MV (2005) Right ventricular dysfunction and pulmonary obstruction index at helical CT: prediction of clinical outcome during 3-month follow-up in patients with acute pulmonary embolism. Radiology 235:798–803
Menendez R, Nauffal D, Cremades MJ (1998) Prognostic factors in restoration of pulmonary flow after submassive pulmonary embolism: a multiple regression analysis. Eur Respir J 11:560–564
Nauffal Manzur D, Menendez Villanueva R, Cremades Romero MJ (1997) The prognostic factors for early mortality and for total or partial gammagraphic resolution in venous thromboembolic disease. Arch Bronconeumol 33:220–224
Prediletto R, Paoletti P, Fornai E, Perissinotto A, Petruzzelli S, Formichi B, Ruschi S, Palla A, Giannella-Neto A, Giuntini C (1990) Natural course of treated pulmonary embolism. Evaluation by perfusion lung scintigraphy, gas exchange, and chest roentgenogram. Chest 97:554–561
Johnson TR, Krauss B, Sedlmair M, Grasruck M, Bruder H, Morhard D, Fink C, Weckbach S, Lenhard M, Schmidt B, Flohr T, Reiser MF, Becker CR (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17:1510–1517
Zatz LM (1976) The effect of the kVp level on EMI values. Selective imaging of various materials with different kVp settings. Radiology 119:683–688
Ferda J, Ferdova E, Mirka H, Baxa J, Bednarova A, Flohr T, Schmidt B, Matejovic M, Kreuzberg B (2009) Pulmonary imaging using dual-energy CT, a role of the assessment of iodine and air distribution. Eur J Radiol. doi:10.1016/j.ejrad.2009.08.005DOI:dx.doi.org
Pontana F, Faivre JB, Remy-Jardin M, Flohr T, Schmidt B, Tacelli N, Pansini V, Remy J (2008) Lung perfusion with dual-energy multidetector-row CT (MDCT): feasibility for the evaluation of acute pulmonary embolism in 117 consecutive patients. Acad Radiol 15:1494–1504
Thieme SF, Becker CR, Hacker M, Nikolaou K, Reiser MF, Johnson TR (2008) Dual energy CT for the assessment of lung perfusion - correlation to scintigraphy. Eur J Radiol 68:369–374
Thieme SF, Johnson TR, Lee C, McWilliams J, Becker CR, Reiser MF, Nikolaou K (2009) Dual-energy CT for the assessment of contrast material distribution in the pulmonary parenchyma. Am J Roentgenol 193:144–149
Zhang LJ, Chai X, Wu SY, Zhao YE, Hu XB, Hu YX, Xue YB, Yang GF, Zhu H, Lu GM (2009) Detection of pulmonary embolism by dual energy CT: correlation with perfusion scintigraphy and histopathological findings in rabbits. Eur Radiol 19:2844–2854
Bauer RW, Kerl JM, Weber E, Weisser P, Korkusuz H, Lehnert T, Jacobi V, Vogl TJ (2010) Lung perfusion analysis with dual energy CT in patients with suspected pulmonary embolism - Influence of window settings on the diagnosis of underlying pathologies of perfusion defects. Eur J Radiol. doi:10.1016/j.ejrad.2010.09.009
Chae EJ, Seo JB, Jang YM, Krauss B, Lee CW, Lee HJ, Song KS (2010) Dual-energy CT for assessment of the severity of acute pulmonary embolism: pulmonary perfusion defect score compared with CT angiographic obstruction score and right ventricular/left ventricular diameter ratio. Am J Roentgenol 194:604–610
Zhang LJ, Yang GF, Zhao YE, Zhou CS, Lu GM (2009) Detection of pulmonary embolism using dual-energy computed tomography and correlation with cardiovascular measurements: a preliminary study. Acta Radiol 50:892–901
Grau E, Tenias JM, Soto MJ, Gutierrez MR, Lecumberri R, Perez JL, Tiberio G (2007) D-dimer levels correlate with mortality in patients with acute pulmonary embolism: Findings from the RIETE registry. Crit Care Med 35:1937–1941
Jeebun V, Doe SJ, Singh L, Worthy SA, Forrest IA (2009) Are clinical parameters and biomarkers predictive of severity of acute pulmonary emboli on CTPA? QJM 103:91–97
Klok FA, Van Der Bijl N, Eikenboom HC, Van Rooden CJ, De Roos A, Kroft LJ, Huisman MV (2010) Comparison of CT assessed right ventricular size and cardiac biomarkers for predicting short-term clinical outcome in normotensive patients suspected of having acute pulmonary embolism. J Thromb Haemost 8:853–856
Laporte S, Mismetti P, Decousus H, Uresandi F, Otero R, Lobo JL, Monreal M (2008) Clinical predictors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: findings from the Registro Informatizado de la Enfermedad TromboEmbolica venosa (RIETE) Registry. Circulation 117:1711–1716
Lobo JL, Zorrilla V, Aizpuru F, Grau E, Jimenez D, Palareti G, Monreal M (2009) D-dimer levels and 15-day outcome in acute pulmonary embolism. Findings from the RIETE Registry. J Thromb Haemost 7:1795–1801
Singanayagam A, Scally C, Al-Khairalla MZ, Leitch L, Hill LE, Chalmers JD, Hill AT (2010) Are biomarkers additive to pulmonary embolism severity index for severity assessment in normotensive patients with acute pulmonary embolism? QJM. doi:10.1093/qjmed/hcq168
Quiroz R, Kucher N, Schoepf UJ, Kipfmueller F, Solomon SD, Costello P, Goldhaber SZ (2004) Right ventricular enlargement on chest computed tomography: prognostic role in acute pulmonary embolism. Circulation 109:2401–2404
Schoepf UJ, Kucher N, Kipfmueller F, Quiroz R, Costello P, Goldhaber SZ (2004) Right ventricular enlargement on chest computed tomography: a predictor of early death in acute pulmonary embolism. Circulation 110:3276–3280
Kjaergaard J, Schaadt BK, Lund JO, Hassager C (2008) Quantification of right ventricular function in acute pulmonary embolism: relation to extent of pulmonary perfusion defects. Eur J Echocardiogr 9:641–645
Acknowledgements
Ralf W. Bauer and J. Matthias Kerl: Research consultants and Speaker’s Bureau Siemens AG
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauer, R.W., Frellesen, C., Renker, M. et al. Dual energy CT pulmonary blood volume assessment in acute pulmonary embolism – correlation with D-dimer level, right heart strain and clinical outcome. Eur Radiol 21, 1914–1921 (2011). https://doi.org/10.1007/s00330-011-2135-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2135-1