Abstract
Objective:
To retrospectively evaluate the magnetic resonance (MR) imaging findings of breast cancer before neoadjuvant chemotherapy (NAC) and to compare findings of chemosensitive breast cancer with those of chemoresistant breast cancer.
Methods:
The MR imaging findings before NAC in 120 women undergoing NAC were reviewed. The MR imaging findings were compared with the pathological findings and responses.
Results:
A complete response (pCR) and marked response were achieved in 12 and 35% of 120 breast cancers in 120 women respectively. Breast cancers with a pCR or marked response were classified as chemosensitive breast cancer. The remaining 64 breast cancers (53%) were classified as chemoresistant breast cancer. Large tumour size, a lesion without mass effect, and very high intratumoural signal intensity on T2-weighted MR images were significantly associated with chemoresistant breast cancer. Lesions with mass effect and washout enhancement pattern were significantly associated with chemosensitive breast cancer. Areas with very high intratumoural signal intensity on T2-weighted images corresponded pathologically to areas of intratumoural necrosis.
Conclusion:
Several MR imaging features of breast cancer before NAC can help predict the efficacy of NAC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of neoadjuvant chemotherapy (NAC) has become the standard treatment of breast cancer, especially locally advanced breast cancer. Breast imaging techniques are important both for early identification of non-responders and for more accurate assessment of residual tumours at the termination of NAC in determining the surgical course of action. Some reports indicate that magnetic resonance (MR) imaging is the most effective technique for assessing residual disease [1–5] and monitoring tumour response [4–7]. However, the main concern may be a delay between the MR imaging findings and the treatment response of NAC. If it were possible to predict who will respond and who will have a relapse based on the baseline MR imaging characteristics, then the baseline MR imaging findings would yield data that could assist in both the pre-treatment planning and the prognosis, as well as in providing an effective non-invasive imaging technique.
Previous studies have demonstrated correlations between the initial morphological patterns of breast tumours in baseline MR imaging and their likelihood of response to NAC [8–10]. The Breast Imaging Reporting and Data System (BI-RADS) MR imaging lexicon has been developed to standardise breast MR imaging terminology [11]. Nonetheless, no study has addressed the correlations between the MR imaging findings of breast tumours at baseline using the BI-RADS lexicon and their likelihood of response to NAC. This study was undertaken to retrospectively evaluate the MR imaging findings of breast cancer before NAC, using terminology defined in the BI-RADS MR imaging lexicon, and to compare those of chemosensitive breast cancer with those of chemoresistant breast cancer.
Materials and methods
Patients
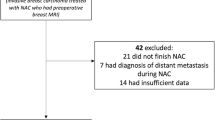
The study protocol was approved by the institutional review boards. All patients provided their written informed consent to undergo the NAC protocol, and separate consent for the review of their medical records, files and images. The eligibility criteria were as follows: patients with histopathologically confirmed breast cancer >3 cm in diameter or with histocytologically confirmed axillary lymph node involvement who underwent NAC from December 2005 to December 2008, who had undergone baseline MR imaging and who underwent surgery after completing NAC. In the analysis, 120 patients (mean age 53 years, range 28–75 years) met the criteria to be included. No data were excluded from the analysis.The patient characteristics, including age, pre-treatment tumour size, histological type, histological tumour grade, receptor status [oestrogen (ER), progesterone (PR) and human epidermal growth factor receptor 2 (HER-2)], intratumoural necrosis positivity, and nodal status are listed in Table 1. One of the four metaplastic carcinomas was determined to be a matrix-producing carcinoma.
All diagnostic interventions were performed after the MR examination to avoid confounding features such as haemorrhage.
Neoadjuvant chemotherapy
Fifty-five patients received a combination of epirubicin and cyclophosphamide followed by docetaxel, 23 patients received a combination of epirubicin and cyclophosphamide followed by paclitaxel and trastuzumab, 18 patents received a combination of 5-fluorouracil, epirubicin and cyclophosphamide followed by docetaxel, 14 patients received a combination of epirubicin and cyclophosphamide followed by paclitaxel, and 10 patients received a combination of epirubicin and cyclophosphamide according to standard protocols in use at the time. Trastuzumab was administered to 23 patients who had HER-2-positive tumours, however, 9 HER-2-positive patients did not receive trastuzumab because they began therapy before trastuzumab was introduced.
MR imaging technique
Magnetic resonance examinations were performed with the patients in the prone position using a 1.5 T Gyroscan Intera (Philips Medical Systems, Best, the Netherlands) with breast-surface coils. A localising sequence was followed by sagittal fast-spin echo T2-weighted imaging (TR/TE 5056/90, ETL 15, matrix 158 × 320) with fat suppression (spectral presaturation inversion recovery, SPIR) of the affected breast. Other parameters were field-of-view 18 cm, section thickness 4 mm, interslice gaps 0.8 mm. This examination was followed by a dynamic study of the affected breast, consisting of serial imaging of a three-dimensional sagittal turbo-field echo T1-weighted sequence (TR/TE 11/5.4, flip angle 20, matrix 143 × 256) with fat suppression (principle of selective excitation technique, ProSet). The parameters were field-of-view 18 cm and section thickness 2-mm slices were interpolated to 1 mm. Gadopentetate dimeglumine (Magnevist; Bayer Healthcare Pharmaceuticals) was administered as a bolus intravenous injection (2 ml/s) at a dose of 0.1 mmol/kg body weight followed by a 20-ml saline solution flush. One pre- and three post-enhancement images were acquired over a period of 6 min after intravenous injection.
Interpretation of MR findings
Magnetic resonance images in 120 patients with 120 breast cancers were randomised and independently reviewed using the BI-RADS MR lexicon (11) by two radiologists (T.U. and S.Y., who have 9 and 13 years of breast MR imaging experience respectively) without knowledge of the clinicopathological findings. If different BI-RADS assessment categories were assigned by the two readers, then a consensus was reached after discussing the findings. The morphology and kinetics at MR imaging were evaluated for all lesions following the BI-RADS MR lexicon. In addition, the intratumoural signal intensity of the tumour was visually evaluated on fat-suppressed T2-weighted MR images. A visual evaluation determined whether the intratumoural signal intensity was stronger and almost the same as water or vessels (very high). The radiologist (T.U.) placed regions of interest to evaluate the enhancement pattern that was demonstrative of the higher visual enhancement on an interactive workstation for the time-signal intensity curves. Time-signal intensity curve patterns were categorised into three types (persistent, plateau, or washout pattern) on the images obtained during the last three phases of contrast-enhanced dynamic imaging according to the BI-RADS MR guidelines [11]. In addition, the tumour size was measured at the longest diameter. The tumour location was also recorded. The disease extent type was classified into the following three types: unifocal type was defined when only one malignant focus was found in the breast, multifocal type was defined when more than one malignant focus was shown in the same quadrant, and multicentric type was defined when more than one malignant focus was shown in more than a single quadrant. A composite measurement of all tumours was taken when multifocal tumours were observed over a large area. When multicentric tumours were observed, the MR imaging findings of the largest tumour were recorded.
Pathological examination
Samples for histopathological examination were prepared by making serial 5-mm slices of breast-conserving surgical specimens and 5- to 10-mm slices of mastectomy specimens according to the technique of Egan [12]. All surgical specimens were sliced perpendicular to an imaginary line from the nipple to the axilla. Histological diagnoses were made by one pathologist (M.K.) with 16 years’ experience in breast histology. The histological therapeutic effects were determined according to the criteria established by the Committee for Production of Histopathological Criteria for Assessment of Therapeutic Response of the Japanese Breast Cancer Society [13]. The histological therapeutic effect was classified in one of four categories: grade 0, no response, almost no change in cancer cells after treatment; grade 1, slight response, mild changes in cancer cells regardless of the extent, and/or marked changes in less than one-third of cancer cells or marked changes in one-third or more but less than two-thirds of cancer cells; grade 2, marked response, marked changes in two-thirds or more of tumour cells with apparent remaining cancer cells or marked changes approaching a complete response with only a few remaining cancer cells; grade 3, complete response, necrosis and/or disappearance of all tumour cells, and/or the replacement of cancer cells by granulation and/or fibrosis [13]. Breast cancer was divided into two types according to the histological therapeutic effects: chemosensitive breast cancer was defined when the histological therapeutic effect was evaluated as grade 2 or 3; and chemoresistant breast cancer was defined when the histological therapeutic effect was evaluated as grade 0 or 1.
Immunohistochemical analyses for ER (1D5, DAKO, Carpinteri, CA, USA), PR (pGR636, DAKO) and HER2 (HercepTest, DAKO) were performed by using the DAKO autostainer (Glostrup, Denmark). The status of each receptor was considered to be negative if the expression was less than 10%, and positive if the expression was 10% or greater. The results for HER2 expression by immunohistochemical analysis were scored as negative, 1+, 2+ or 3+, according to the manufacturer’s recommendations. Specimens with a score of negative or 1+ were considered HER2-negative. HER2/chromosome 17 FISH was performed using Vysis PathVysion (Abbott, Downers Grove, IL, USA) and Histra (JOKOH, Tokyo, Japan) on tumours in which the immunohistochemical analysis score was 2+. The correlation between the histological and the MR findings was examined by the radiologists (T.U. and S.Y.) and pathologist (M.K.) in all cases.
Statistical analysis
The chi-squared, Fisher’s exact and Student’s t-tests were used to compare the MR findings between chemosensitive breast cancer and chemoresistant breast cancer. All analyses were performed using the SPSS 11.0 statistical software package (Chicago, IL, USA), with a value of P < 0.05 considered to be significant.
Results
Histology, hormone receptor status and MR imaging descriptor
Women with invasive ductal carcinoma were more likely to have a lesion with mass effect on MR images than women with invasive lobular carcinoma, although this tendency was not significant (P = 0.192; Table 2).
Histological therapeutic effect
The histological therapeutic effects showed chemosensitive breast cancer and chemoresistant breast cancer in 47% (56/120) and 53% (64/120; Table 3) of patients respectively. The characteristics of patients with chemosensitive breast cancer and chemoresistant breast cancer are listed in Table 4. There was no age-related bias between the groups. There was no association of disease extent type, histological grade, axillary lymph node positivity and triple-negative breast cancer with chemosensitive breast cancer and chemoresistant breast cancer. The mean tumour size in women with chemoresistant breast cancer was significantly larger than that in women with chemosensitive breast cancer.
Lesion type on MR imaging and histological therapeutic effect
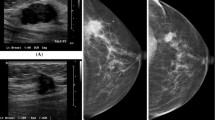
The lesions with mass effect (Fig. 1) on MR images were significantly associated with chemosensitive breast cancer (P = 0.032; Table 5). Most of the chemosensitive breast cancers showed the lesions with mass effect on MR images (80%). The MR images of the remaining 11 lesions without mass effect consisted of nine segmental (16%), one focal (2%) and one ductal (2%) non-mass-like enhancements. The chemoresistant breast cancer group showed 40 lesions with mass effect (63%), 23 (36%) segmental lesions without mass effect (Fig. 2) and 1 (2%) focal lesion without mass effect.
Chemosensitive breast cancer of the left breast in a 46-year-old woman. a Sagittal fat-suppressed T2-weighted MR image (5056/90/15) shows a mass with a smooth border with relatively higher intensity than that of the surrounding breast tissue. Sagittal turbo-field echo T1-weighted image (11/5.4/20) with fat suppression (b) and dynamic breast MR images obtained at 120 s (c) and 360 s (d) after the administration of gadolinium show a rapid, strong, washout, and rim-enhancing mass with a smooth border
Chemoresistant breast cancer of the left breast in a 45-year-old woman. Sagittal fat-suppressed T2-weighted MR image (5056/90/15) shows a mass with an irregular border with equivalent intensity to that of the surrounding breast tissue (a). Note the very high peritumoral (outside the tumour) intensity which might reveal peritumoral oedema. Sagittal turbo-field echo T1-weighted image (11/5.4/20) with fat suppression (b) and dynamic breast MR images obtained at 120 s (c) and 360 s (d) after the administration of gadolinium show a persistent segmental enhancing lesion without mass effect (arrows)
MR findings of lesions with mass effect
A washout enhancement pattern (P = 0.014) was significantly associated with chemosensitive breast cancers (Table 5). Very high intratumoural signal intensity on T2-weighted images (P = 0.003) was significantly associated with chemoresistant breast cancer (Table 5). Three (19%) of the 16 chemoresistant breast cancers with very high intratumoural signal on T2-weighted images were mucinous carcinoma, matrix-producing carcinoma and invasive ductal carcinoma with intratumoural haemorrhage. The remaining 13 (82%) had intratumoural necrosis. In the remaining MR findings of lesions with mass effect, no association was observed with any other MR imaging findings with chemosensitive breast cancer and chemoresistant breast cancer.
MR findings of lesions without mass effect
In addition, no association was seen between MR imaging findings of lesions without mass effect and either chemosensitive breast cancer or chemoresistant breast cancer (Table 5). Furthermore, for the lesions without mass effect, none showed very high intratumoural intensity on T2-weighted images.
Necrosis
Areas with very high intratumoural signal intensity on T2-weighted images corresponded pathologically to areas of intratumoural necrosis (Fig. 3). The rate of intratumoural necrosis in chemoresistant breast cancer was 20%, which was slightly, but not significantly, higher than the 9% rate of chemosensitive breast cancer (Table 4). Thirteen (33%) of the 40 chemoresistant breast cancers that were lesions with mass effect had intratumoural necrosis (Tables 4, 5). Five (11%) chemosensitive breast lesions with mass effect had very high intratumoural signal intensity on T2-weighted images that corresponded pathologically to areas of intratumoural necrosis (Tables 4, 5).
Chemoresistant breast cancer of the right breast in a 35-year-old woman. Sagittal fat-suppressed T2-weighted MR image (5056/90/15) shows a mass with a relatively smooth border with an area of very high intratumoural intensity (a). Note an area with very high intratumoural signal intensity that corresponded pathologically to an area of intratumoural necrosis. Sagittal turbo-field echo T1-weighted image (11/5.4/20) with fat suppression (b) and dynamic breast MR images obtained at 120 s (c) and 360 s (d) after the administration of gadolinium show a slow, washout, and rim-enhancing mass with a relatively smooth border
Discussion
Previous studies have found correlations between the initial morphological patterns of breast tumours on baseline MR imaging and their likelihood of response to NAC [8–10]. However, previous studies did not use the BI-RADS MR imaging lexicon when analysing the MR findings. In recent years, the BI-RADS MR imaging lexicon has been developed to standardise breast MR imaging terminology [11]. This study is the first full study to demonstrate a correlation between the baseline MR imaging and histopathological findings about their likelihood of response to NAC. The current study showed that several MR findings, such as a lesion with mass effect, a washout enhancement pattern, and very high intratumoural signal intensity on T2-weighted MR images are useful in predicting the efficacy of NAC.
Esserman et al. [8] reported that five distinct MR imaging patterns were identified and the morphological pattern was found to be associated with the tumour response, with 77% of circumscribed tumours with mass effect demonstrating a partial or complete response versus 25% of tumours of the septal spread type. The present study showed a statistically significantly higher rate of lesions with mass effect in patients with chemosensitive breast cancer. Forty-five out of 56 (80%) patients with chemosensitive breast cancer and 40 out of 64 (63%) patients with chemoresistant breast cancer had a lesion with mass effect on MR imaging. These results are consistent with those described in previous reports [8, 10].
The current study showed that a washout enhancement pattern was significantly associated with chemosensitive breast cancer. Initially rapid enhancement and a washout pattern are generally regarded to be a malignant pattern on breast MR imaging. Early signal enhancement with rapid washout of intravenous contrast material correlated with high tumour vascularity [14]. In addition, Rieber et al. reported that chemosensitive breast cancer showed a higher average enhancement on baseline MR imaging before NAC and that the phenomenon could be due to greater vascularisation in chemosensitive breast cancer in comparison to chemoresistant breast cancer [15]. A washout enhancement pattern can be a surrogate for the extracellular extravascular space of the tumour, which is considered to be a surrogate measure of the amount of exposure that cells of the tumour have to the initial delivery of primary chemotherapy [16, 17]. Therefore, a washout enhancement pattern can indicate high exposure of tumour cells to chemotherapeutic agents and a more effective initial cycle of primary chemotherapy. However, the frequency of the fast initial phase enhancement kinetic descriptor was shown in both chemosensitive breast cancer and chemoresistant breast cancer, and therefore this study showed that an initially rapid enhancement was not useful in predicting the efficiency of NAC.
A very high intratumoural signal on T2-weighted images, corresponding to necrosis, was significantly more frequent in masses with chemoresistant breast cancer than in masses with chemosensitive breast cancer. Necrosis is a prognostic factor in invasive breast cancer [18, 19]. In addition, Leek et al. suggested that aggressive invasive breast cancers rapidly outgrew their vascular supply in certain areas, leading to areas of prolonged hypoxia within the tumour and, subsequently, to necrosis [20]. The present study showed a correlation of intratumoural necrosis with the very hyperintense area on T2-weighted images consistent with the findings in a previous study of breast tumours [21, 22]. The presence of tumour necrosis, which is assessed using surgical specimens obtained after NAC, is considered to be a pathological complete response because the necrosis is caused by NAC [13]. A recent study reported that it is very important and difficult to determine whether the presence of intratumoural necrosis treated with NAC has truly been produced by NAC or not [23]. The baseline MR imaging findings can easily predict the presence of intratumoural necrosis before NAC. The current study found three chemoresistant breast cancers without necrosis that revealed very high intensity on T2-weighted images, consisting of one mucinous carcinoma, one matrix-producing carcinoma and one invasive ductal carcinoma with haemorrhage. These special types of breast cancers with a long T2 relaxation time may be chemoresistant.
This study showed that women with invasive ductal carcinoma were more likely to have a lesion with mass effect on MR images, which was significantly associated with chemosensitive breast cancer, than women with invasive lobular carcinoma. The result may be a key to the reason why the pathological complete response rates were lower in patients with invasive lobular carcinoma in comparison to those with invasive ductal carcinoma [24, 25]. The present study implies that the lesion type on baseline MR imaging can predict the efficiency of NAC regardless of the histological type.
This study has limitations: First, the number of patients studied was small. Therefore, the statistical significance of these findings may be insufficient. Second, not all patients with HER-2-positive disease in this series were treated according to recent guidelines with the standard agent trastuzumab. However, 23 out of 32 patients (72%) who had HER-2-positive tumours received trastuzumab. The chemosensitive breast cancer incidence was 18 out of 23 (78%). The result is consistent with that described in a previous report [26]. The NAC regimens tend to differ substantially from centre to centre because the inclusion criteria also tend to differ. All these facts might lead to some bias when evaluating any correlations between the baseline MR imaging findings and the pathological responses to NAC. Third, this study was a retrospective analysis with two experienced radiologists, which potentially limits the generalisability of the results to studies of prospectively assessed BI-RADS descriptors across a diverse group of radiologists and patients.
In conclusion, the current study provided clinical data regarding the MR imaging findings of breast cancer before NAC for predicting the efficacy of NAC in the BI-RADS MR imaging lexicon. Furthermore, the results demonstrate that several MR imaging features before NAC can be useful for predicting the efficacy of NAC. A large tumour size (P = 0.029), a lesion without mass effect (P = 0.032) and very high intratumoural signal intensity on T2-weighted MR images (P = 0.003) were all significantly associated with chemoresistant breast cancer. Conversely, a lesion with mass effect (P = 0.032) and a washout enhancement pattern (P = 0.014) were also observed to be significantly associated with chemosensitive breast cancer. The early MR imaging prediction of the efficacy of therapy response before NAC could assist in both the pre-treatment planning and the prognosis, as well as in providing an effective non-invasive imaging technique.
References
Rosen EL, Blackwell KL, Baker JA et al (2003) Accuracy of MRI in the detection of residual breast cancer after neoadjuvant chemotherapy. AJR Am J Roentgenol 181:1275–1282
Partridge SC, Gibbs JE, Lu Y, Esserman LJ, Sudilovsky D, Hylton NM (2002) Accuracy of MR imaging for revealing residual breast cancer in patients who have undergone neoadjuvant chemotherapy. AJR Am J Roentgenol 179:1193–1199
Londero V, Bazzocchi M, Frate CD et al (2004) Locally advanced breast cancer: comparison of mammography, sonography and MR imaging in evaluation of residual disease in women receiving neoadjuvant chemotherapy. Eur Radiol 14:1371–1379
Balu-Maestro C, Chapellier C, Bleuse A, Chanalet I, Chauvel C, Largillier R (2002) Imaging in evaluation of response to neoadjuvant breast cancer treatment benefits of MRI. Breast Cancer Res Treat 72:145–152
Akazawa K, Tamaki Y, Taguchi T et al (2006) Preoperative evaluation of residual tumor extent by three-dimensional magnetic resonance imaging in breast cancer patients treated with neoadjuvant chemotherapy. Breast J 12:130–137
Abraham DC, Jones RC, Jones SE et al (1996) Evaluation of neoadjuvant chemotherapeutic response of locally advanced breast cancer by magnetic resonance imaging. Cancer 78:91–100
Yeh E, Slanetz P, Kopans DB et al (2005) Prospective comparison of mammography, sonography, and MRI in patients undergoing neoadjuvant chemotherapy for palpable breast cancer. AJR Am J Roentgenol 184:868–877
Esserman L, Kaplan E, Partridge S et al (2001) MRI phenotype is associated with response to doxorubicin and cyclophosphamide neoadjuvant chemotherapy in stage 3 breast cancer. Ann Surg Oncol 8:549–559
Martincich L, Montemurro F, Cirillo S et al (2003) Role of magnetic resonance imaging in the prediction of tumor response in patients with locally advanced breast cancer receiving neoadjuvant chemo-therapy. Radiol Med 106:51–56
Murata Y, Ogawa Y, Yoshida S et al (2004) Utility of initial MRI for predicting extent of residual disease after neoadjuvant chemotherapy: analysis of 70 breast cancer patients. Oncol Rep 12:1257–1262
Ikeda DM, Hylton NM, Kuhl CK et al (2003) Breast imaging reporting and data system, BI-RADS: MRI, 4th edn. American College of Radiology, Reston, VA
Egan RL (1982) Multicentric breast carcinomas: clinical-radiographic-pathologic whole organ studies and 10-year survival. Cancer 49:1123–1130
Kurosumi M, Akashi-Tanaka S, Akiyama F et al (2008) Histopathological criteria for assessment of therapeutic response in breast cancer (2007 version). Breast Cancer 15:5–7
Esserman L, Hylton N, George T, Weidner N (1999) Contrast-enhanced magnetic resonance imaging to assess tumor histopathology and angiogenesis in breast carcinoma. Breast J 5:13–21
Rieber A, Zeitler H, Rosenthal H et al (1997) MRI of breast cancer: influence of chemotherapy on sensitivity. Br J Radiol 70:452–458
Craciunescu OI, Blackwell KL, Jones EL et al (2009) DCE-MRI parameters have potential to predict response of locally advanced breast cancer patients to neoadjuvant chemotherapy and hyperthermia: a pilot study. Int J Hyperthermia 25:405–415
Semple SI, Staff RT, Heys SD et al (2006) Baseline MRI delivery characteristics predict change in invasive ductal breast carcinoma PET metabolism as a result of primary chemotherapy administration. Ann Oncol 17:1393–1398
Fisher ER, Anderson S, Redmond C, Fisher B (1993) Pathologic findings from the National Surgical Adjuvant Breast Project B-06. 10-year pathologic and clinical prognostic discriminants. Cancer 71:2507–2514
Jimenez RE, Wallis T, Visscher DW (2001) Centrally necrotizing carcinoma of the breast: a distinct histologic subtype with aggressive clinical behavior. Am J Surg Pathol 25:331–337
Leek RD, Landers RJ, Harris AL, Lewis CE (1999) Necrosis correlates with high vascular density and focal macrophage infiltration in invasive carcinoma of the breast. Br J Cancer 79:991–995
Metz S, Daldrup-Link HE, Richter T et al (2003) Detection and quantification of breast tumor necrosis with MR imaging: value of the necrosis-avid contrast agent gadophrin-3. Acad Radiol 10:484–490
Uematsu T, Kasami M, Yuen S (2009) Triple-negative breast cancer: correlation between MR imaging and pathologic findings. Radiology 250:638–647
Tamura N, Hasebe T, Okada N et al (2009) Tumor histology in lymph vessels and lymph nodes for the accurate prediction of outcome among breast cancer patients treated with neoadjuvant chemotherapy. Cancer Sci 100:1823–1833
Tubiana-Hulin M, Stevens D, Lasry S et al (2006) Response to neoadjuvant chemotherapy in lobular and ductal breast carcinomas: a retrospective study on 860 patients from one institution. Ann Oncol 17:1228–1233
Cristofanilli M, Gonzalez-Angulo A, Sneige N et al (2005) Invasive lobular carcinoma classic type: response to primary chemotherapy and survival outcomes. J Clin Oncol 23:41–48
Chen JH, Feig B, Agrawal G et al (2008) MRI evaluation of pathologically complete response and residual tumors in breast cancer after neoadjuvant chemotherapy. Cancer 112:17–26
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uematsu, T., Kasami, M. & Yuen, S. Neoadjuvant chemotherapy for breast cancer: correlation between the baseline MR imaging findings and responses to therapy. Eur Radiol 20, 2315–2322 (2010). https://doi.org/10.1007/s00330-010-1813-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-010-1813-8