Abstract
Objective
To assess diastolic function in patients with constrictive pericarditis (CP) by using velocity-encoded flow measurements at the atrioventricular valves and to evaluate whether conclusions regarding increased ventricular pressure can be drawn.
Methods
Twenty-two patients with CP and 20 healthy subjects were examined on a 1.5-T MR system. In addition to evaluation of pericardial thickness, ventricular volumes and septal movement, velocity-encoded flow measurements were performed at the level of the atrioventricular valves for assessment of diastolic function. Amplitudes of the e- and a-waves were measured and e- to a-wave ratios were calculated. The correlation of transtricuspid e- to a-wave ratios and right ventricular end-diastolic pressures (RVEDP) was calculated.
Results
Right ventricular volumes were significantly smaller in patients with CP (p < 0.001). Abnormal septal movement was detected in all patients except one with CP and in none of the healthy subjects. In patients with CP mean transtricuspid e- to a-wave ratios were significantly smaller compared with healthy subjects. Individual transtricuspid e- to a-wave ratios were highly correlated with RVEDP (r = 0.6, p = 0.01).
Conclusions
An elaborate MR examination can identify patients with CP. Velocity-encoded flow measurements with calculation of transtricuspid e- to a-wave ratios are a valuable tool for detection of diastolic dysfunction in patients with CP. The value of e- to a-wave ratios may indicate elevated RVEDP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The characteristic morphological finding of constrictive pericarditis (CP) is a thickened, fibrotic and/ or calcified pericardium, which constricts the heart. This leads to impairment of cardiac compliance resulting in right ventricular or biventricular diastolic dysfunction [1]. Normal pericardial thickness is 2 mm or less; a thickness greater than 4 mm suggests pericardial constriction and thickness greater than 6 mm is highly specific for constriction [1]. However, the presence of pericardial thickening by itself does not indicate constriction [2]. Conversely, normal pericardial thickness does not necessarily exclude a diagnosis of constrictive pericarditis [3]. Additional morphological findings associated with constriction include distorted contours of the ventricles, tubular-shaped ventricles, hepatic venous congestion, ascites, pleural effusions and occasionally pericardial effusion. A dilatation of the atria, the coronary sinus, the inferior vena cava and the hepatic veins are common findings. Evaluation of diastolic function is important for the functional assessment of CP.
Transthoracic and trans-oesophageal Doppler echocardiography have been the non-invasive methods of choice to assess diastolic function by flow measurements across the atrioventricular (AV) valves [4–6]. However, the restricted acoustic window and field of view limit the usefulness of this technique and right ventricular recordings are often not satisfactory [7]. In addition, many patients are difficult to examine by this approach because of the presence of calcifications within the pericardium.
As cardiac MRI is not associated with these limitations and techniques have been validated for assessment of diastolic function, the aim of the present study was to evaluate the feasibility and diagnostic value of velocity-encoded flow measurements at the atrioventricular valves for assessment of diastolic dysfunction in patients with CP. Furthermore the potential to indicate increased ventricular pressure should be evaluated [8–15].
Materials and methods
Study population
The study protocol was approved by our institutional review board, and written informed consent was obtained. The study group included 20 healthy volunteers (15 men, 5 women; mean age 53 years ± 13 [SD], age range 38–72 years) and 22 patients (18 men, 4 women; mean age 52 years ± 12 [SD]; age range 41–70 years) who presented with signs and symptoms of constrictive pericarditis and were referred for magnetic resonance examination between November 2002 and October 2007. All patients had been evaluated previously with electrocardiography, chest radiography and echocardiography, though only a fraction of the echocardiographic examinations allowed for comprehensive diagnostic assessment because of impairment of examination conditions. Eighteen patients had received an intracardiac catheter with measurement of the right ventricular end-diastolic pressure and, if present, registration of a characteristic dip-plateau phenomenon. The diagnosis of CP was made if the patient had objective evidence of impaired cardiac filling, i.e. increased filling pressures or echo-Doppler ultrasound (US) signs of increased ventricular coupling combined with pericardial thickening of 2 mm or more. In addition, surgical confirmation of constrictive pericarditis was obtained after pericardectomy in all patients. The aetiology of constrictive pericarditis was unknown in 6 patients, whereas 11 patients had previous cardiac surgery, 3 had radiation therapy and 2 had a history of an inflammatory disease.
MR imaging
All MRI studies were performed on a 1.5-T unit (Magnetom Avanto; Siemens Medical Solutions, Erlangen, Germany) with a high-performance gradient system (maximum gradient amplitude 45 mT/m; maximum slew rate 200-µs rise time), a 12-element-body phased-array coil system and electrocardiographic triggering.
Morphology and systolic function
The MRI protocol included a T1-weighted fast spin-echo sequence in the cardiac short-axis plane during breath-hold (voxel size 2.5 × 1.5 × 5.0 mm3; TE 30 ms) and a HASTE sequence in axial and coronal planes (voxel size 2.4 × 1.4 × 8.0 mm3; TE 40 ms) for morphological analysis. Right and left ventricular systolic function were assessed by using an ECG-triggered breath-hold segmented steady-state free precession (SSFP) cine sequence (TR/TE 2.8/1.4 ms; flip angle 60°; slice thickness 8 mm; in-plane resolution 2.5 × 1.9 mm2; temporal resolution 48 ms). SSFP cine frames were obtained in a short-axis orientation and additionally in long-axis orientations (two-chamber and four-chamber planes, respectively).
Diastolic function
Diastolic function was assessed by (i) evaluation of septal motion during diastole on short-axis cine frames, which were acquired as described above and by (ii) velocity-encoded flow measurements at the level of the tricuspid and mitral valves. Velocity-encoded phase contrast MR was performed with retrospective gating across the mitral and tricuspid valves by using a two-dimensional flow-sensitive gradient-echo sequence without breath-hold. The flow measurements were performed in order to evaluate left and right ventricular diastolic function. The imaging planes for the mitral valve and tricuspid valve were planned from the end-systolic and end-diastolic four-chamber views and the two-chamber long-axis views. Both the mitral and tricuspid valve angulations were planned midway between the end-systolic and end-diastolic locations of the valves. The direction of velocity encoding was perpendicular to the imaging plane. Velocity sensitivity was set at 100–150 cm/s to avoid aliasing. Other imaging parameters were as follows: TR/TE 40/3 ms; matrix 256 × 256; spatial resolution 1.6 × 1.6 × 5.0; temporal resolution (reconstructed time frames) 20 ms; flip angle 30°; mean acquisition time 3 min 32 s.
MR imaging analysis
Analysis of morphology
The images were analysed in consensus by two experienced readers (A.H. and K.B., with 12 and 5 years of experience in cardiac MRI, respectively). The images were presented to the readers for analysis in a random order. For morphological evaluation of the pericardium spin-echo and HASTE images were employed (Fig. 1) to assess the maximum pericardial thickness and the distribution pattern of the pericardial thickening, similar to that suggested by Rienmüller [16]:
- Type I CP:
-
global pattern
- Type II CP:
-
focal pattern along one or both atria
- Type III CP:
-
left-sided pattern
- Type IV CP:
-
right-sided pattern
- Type V CP:
-
effusive-constrictive pattern
One additional category was added for patients presenting with signs and symptoms of CP and a pericardial thickness of 2–4 mm, as CP can be present without obvious pericardial thickening, as reported by Talreja et al. [17].
A 42-year-old male patient with symptoms of right-sided heart failure. T1-weighted TSE-MRI (voxel size 2.5 × 1.5 × 5.0 mm3; TE 30 ms) axial views (a) and short-axis views (b). The images illustrate a thickened pericardium predominantly at the level of the right atrium but also, to a lesser extent, at the right ventricle (type IV, arrows)
Analysis of cardiac function
Systolic function
For assessment of right and left ventricular systolic function the MR images were transferred to a Leonardo workstation (Siemens Medical Solutions, Erlangen, Germany). Short-axis cine MR imaging data were analysed by using an MR post-processing software system (ARGUS, Siemens Medical Solutions, Erlangen, Germany). Left and right ventricular endocardial and epicardial contours were drawn semi-automatically on end-diastolic and end-systolic images. Left and right ventricular end-diastolic and end-systolic volumes were measured and stroke volumes (SV) and ejection fractions (EF) were calculated as described previously [18].
Diastolic function
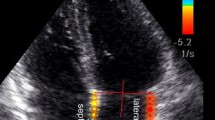
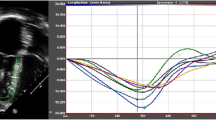
For evaluation of diastolic function septal motion and velocity-encoded flow measurements were assessed (Figs. 2, 3).
A 62-year-old male patient presenting with dyspnoea. Balanced-SSFP cine MRI (TR/TE 2.8/1.4 ms; flip angle 60°; slice thickness 8 mm, in-plane resolution 2.5 × 1.9 mm2; temporal resolution 48 ms) short-axis views (a) and four-chamber long-axis views (b). In systole the interventricular septum has a concave shape in relation to the left ventricle (a, curved black arrow), while during diastole the septum flattens (a, curved white arrow). Abnormal septal motion is also visible in the long chamber views (b, white arrows), as are a right ventricular thickened pericardium (b, arrowheads) and concomitant pleural effusions (*)
a Flow curves of velocity-encoded flow measurements at the mitral and tricuspid valves. Transtricuspid and transmitral flow curves of a 55-year-old male patient are shown with about same heights of the e-wave and the a-wave at both atrioventricular valves resulting in an e- to a-wave ratio of about 1. b Flow curve of a 42-year-old female patient. In contrast to Fig. 3a the amplitudes of the e-waves are higher compared with the a-waves. The e- to a-wave ratio at both the mitral valve and the tricuspid valve are between 1 and 2
Septal motion
Septal motion was evaluated as described by Giorgi et al. on a short-axis cine function view 1 cm beneath the atrioventricular valves by two readers during systole and diastole on a visual basis and described as normal, i.e. concave to the left ventricle, as septal flattening or as septal inversion, i.e. convex to the left ventricle [19].
Velocity-encoded flow measurements
Flow velocity-encoded MR imaging data were analysed by two readers (A.H. and K.B.) in consensus by using the same analytical software package as mentioned above (ARGUS, Siemens Medical Solutions, Erlangen, Germany). Within the mitral and tricuspid valve areas of maximum flow velocity were assigned on a visual basis on every slice (Fig. 4) and a region of interest (ROI) of 1 cm2 was centrally positioned in this area. Flow curves were obtained by automatic measurement of peak flow velocity within these areas. MR imaging-derived recording of diastolic ventricular inflow has, similar to echo-Doppler images, a characteristic biphasic appearance (Fig. 3). Two distinct peaks represent early and late diastolic ventricular filling.
Phase contrast images of flow measurements at the tricuspid (T) and mitral valves (M) in a 62-year-old male patient at different time points during the cardiac cycle. a Diastolic inflow though the atrioventricular valves. The bright areas indicate high flow velocities through the valves. b Image at the end of diastole with almost no flow. c High flow through the pulmonary (P) and aortic valves (A)
Diastolic function parameters derived from the inflow curves were as follows: peak flow velocity during early diastolic filling, represented by the amplitude of the e-wave, peak flow velocity during late diastolic filling by atrial contraction, represented by the amplitude of the a-wave. Hereafter ratios of peak velocity of the e-waves and peak velocity of the a-waves (e- to a-wave ratios) were calculated for the tricuspid and mitral valves. The results of patients with CP were compared with those of healthy volunteers. Additionally, the subgroup of patients with only minor pericardial thickening was compared with patients with pericardial thickening of more than 4 mm. Furthermore, the correlation coefficient of transtricuspid e- to a-wave ratios with right ventricular end-diastolic pressure measurements was assessed and intra-individual correlation coefficients of the mitral and tricuspid e- to a-wave ratios were calculated (Fig. 5).
Statistical analysis
All quantitative results are expressed as means ± standard deviations (SD). Unpaired sample t tests were used to identify significant differences in systolic functional parameters, in peak velocity of the e-wave, and the a-wave and e- to a-wave ratios between patients having CP and healthy subjects. Pearson’s correlation coefficient of transtricuspid versus transmitral e- to a-wave ratios and transtricuspid e- to a-wave ratios versus right ventricular end-diastolic pressures was calculated. Receiver operator characteristics (ROC) curves for identification of constrictive pericarditis were generated for pericardial thickness, right ventricular end-diastolic volumes, septal flattening, e- to a-wave ratios at the tricuspid valve and for the right ventricular end-diastolic pressures. For determination of the best cut-off points to differentiate healthy subjects from those with CP, the Youden index was used [20, 21]. According to that result, sensitivities and specificities were calculated. As intracardiac catheter examinations were not performed in healthy subjects, normal right ventricular end-diastolic pressures (less than 8 mmHg) were assumed for calculation of sensitivity and specificity. P values below 0.05 were considered to indicate significant differences.
Results
Pericardial morphology
Magnetic resonance imaging revealed abnormal pericardial thickening of 4 mm or more—either focally or globally—in 17 of the 22 patients with CP and in none of the healthy subjects. A globally thickened pericardium (type I) was seen in 7 patients; in 2 patients the pericardial thickening was limited to the atria (type II) and 8 patients had a pericardial thickening confined to the right ventricle. A thickened pericardium, limited to the left ventricle (type III) or an effusive constrictive pattern (type V) was not found among our patients. Five cases of CP were classified as type VI, i.e. a pericardial thickening of more than 2 mm but less than 4 mm was present. The mean maximum pericardial thickness of all patients with CP was 6.5 mm ± 1.5 (SD).
Systolic function
The assessment of systolic function revealed impairment of right ventricular and left ventricular function in patients with CP (Table 1). The mean right and left ventricular end-diastolic volumes, the stroke volumes and the mean right and left ventricular ejection fractions were significantly smaller in patients with CP compared with those of healthy subjects.
Diastolic function
Septal motion
Analysis of septal movement during diastole revealed a septal flattening in 20 patients with CP. Septal inversion was seen in 1 patient. One patient and all healthy volunteers had a normal septal configuration during diastole. During systole septal motion was normal in all patients with CP, and in all healthy subjects.
Diastolic flow
The results of velocity-encoded flow measurements at the mitral and tricuspid valves in patients versus control subjects are summarised in Table 2. Measurements at the tricuspid valves showed a significantly lower e- to a-wave ratio in patients with CP in comparison to healthy subjects (p < 0.001). The assessment of the maximum velocity of the a-waves at the tricuspid valve revealed a significantly higher a-wave amplitude in CP compared with controls (p = 0.0035). The calculation of mean values of the transtricuspid e-wave did not display any significant difference in patients with CP in comparison to healthy subjects. Measurements at the mitral valve did not reveal any significant differences between the mean values of the amplitudes of the e-waves, the a-waves or the e- to a-wave ratios in patients with CP compared with controls.
The comparison of the patients with intermediate pericardial thickening (2–4 mm) and those with a pericardial thickness of 4 mm or more revealed no significant differences in diastolic dysfunction (Table 3).
The evaluation of correlation between the right ventricular e- to a-wave ratios and right ventricular end-diastolic pressure measurements of the intracardiac catheter examinations resulted in a correlation coefficient of r = 0.6 (p = 0.01; Fig. 6).
The assessment of intra-individual correlation of e- to a-wave ratios of the measurements across the mitral and the tricuspid valves revealed a good correlation in the healthy subjects (r = 0.86; p < 0.0001). The e- to a-wave ratios of mitral and tricuspid valves showed no significant correlation in patients with CP (r = −0.04; p = 0.86)
Sensitivities and specificities
The values for the sensitivity and specificity for detection of CP by using the parameters of pericardial thickness, right ventricular end-diastolic volumes, septal flattening, e- to a-wave ratios at the tricuspid valve and the right ventricular end-diastolic pressures are shown in Table 4. Calculation of ROC curves resulted in ROC values between 0.833 and 0.976 (Table 4) with septal flattening being superior to e- to a-wave ratios and RVEDP (p = 0.040 and p = 0.035). The combined approach of the variables derived from MR (pericardial thickness, RVEDV, septal flattening and e- to a-wave ratios) resulted in a sensitivity of 0.83 and a specificity of 0.90.
Discussion
Constrictive pericarditis predominantly presents with signs and symptoms of diastolic right heart failure. The aim of this study was therefore in particular to evaluate right ventricular diastolic function in patients with constrictive pericarditis by using velocity-encoded flow measurements at the level of the atrioventricular valves. The major important findings were: (a) The e- to a-wave ratios measured at the tricuspid valves correlated with intracardiac right ventricular catheter measurements in patients with CP. (b) While left and right ventricular e- to a-wave ratios showed a good correlation in healthy subjects, none was present in CP. (c) Abnormal septal movement was seen in all patients but one.
Constrictive pericarditis may present as localised effusive (effusion present), occult (volume depleted), or transient constriction [22]. The hallmark for identification of CP is the thickened and sometimes calcified pericardium. However, CP may also be present without obvious or only minor pericardial thickening (Table 3) [23]. Other typical signs, e.g. small end-diastolic ventricular volumes, may give a hint as to the diagnosis and severity of diastolic dysfunction (Table 1). However, especially when both systolic dysfunction and diastolic dysfunction are present, it is important to assess the severity of diastolic dysfunction in order to select the adequate treatment.
Although velocity-encoded flow measurements for the evaluation of diastolic function are routinely performed by Doppler echocardiography, patients with CP in particular may be difficult to examine because of pericardial calcifications. Therefore, MRI and MR-flow measurements are attractive alternatives for the assessment of diastolic function in this disease entity [24].
In healthy subjects diastole consists of 4 phases: isovolumetric dilatation, early rapid filling, diastasis and atrial contraction resulting in a typical biphasic flow profile with two peaks: early diastolic peak from early rapid filling (E) and late filling peak from atrial contraction (A). In normal conditions the early-filling e-wave velocity is higher than the a-wave velocity, and the e- to a-wave ratio is about 1.5 (Fig. 3b) [25].
In diastolic dysfunction various flow patterns may occur. In early diastolic dysfunction an e- to a-wave ratio of less than or about 1 indicates impaired myocardial relaxation without a significant increase in left atrial pressure. As diastolic function deteriorates, increasing LV filling pressure results in an increase in peak e- and a-wave velocity, caused by an increase in left atrial pressure [26–28]. This “pseudonormalisation” is a transitional phase between abnormal relaxation and restrictive physiology and signifies increased filling pressure combined with decreased compliance. In this phase the flow pattern across the AV valves resembles the normal flow pattern with an e- to a-wave ratio of about 1.5. As can be derived from our data (Table 2, Fig. 6) early diastolic dysfunction and pseudonormalisation were present in most of our patients. In further progression of the disease ventricular diastolic filling occurs primarily during early diastole, because the ventricular pressure at end-diastole is so high that atrial contraction contributes less to left ventricular filling than normal. This so-called restrictive pattern indicates a poor prognosis and may be associated with significantly higher mortality [29].
While diastolic dysfunction is easily identified in abnormal relaxation (e- to a-wave ratios less than 1) and in restriction, difficulties remain in the transitional phase of pseudonormalisation. To differentiate this condition from the normal flow pattern, various echocardiographic parameters were proposed such as measurement of pulmonary venous flow or assessment of diastolic function during a Valsalva manoeuvre [30–32]. Although these measurements could be performed during an MR examination, neither was obtained in the current study and they have to be evaluated in future work.
However, a comprehensive MR examination with evaluation of pericardial thickness, right end-diastolic volumes and the evaluation of septal motion during diastole can contribute information to identify patients with CP with a high sensitivity and specificity. As shown in Table 4 and as previously published by Giorgi et al. [19], abnormal septal motion allows one to discriminate CP patients from healthy subjects and patients with restrictive cardiomyopathy with a high diagnostic accuracy. The predominantly right-sided intracardiac pressure elevation in CP, which contributes to this phenomenon, is typically measured in intracardiac catheter examination. The calculation of the correlation coefficients of right ventricular pressures and e- to a-wave ratios in our patients with CP resulted in a value of r = 0.6 (p = 0.01; Fig. 6). Similar observations have been made for the left ventricle in echocardiography in several disease entities, but to our knowledge no data exist for right ventricular measurements so far [33, 34].
Further diagnostic information may be obtained by a correlation of the intra-individual tricuspid and mitral e- to a-wave ratios. In healthy populations, close correlations have been found between individual right and left ventricular diastolic parameters [35, 36]. Constrictive pericarditis predominantly involves right ventricular diastolic function to a variable extent, independent from an involvement of the left ventricular diastolic function—which may, however, appear in the course of the disease. Therefore this close correlation is lost in CP (Fig. 5).
Limitations
In the current study only cases of surgically proven CP were evaluated and compared with healthy subjects. The differentiation between CP and restrictive cardiomyopathy, the top differential diagnosis, in patients who present with diastolic dysfunction, was not the subject of this research and has to be evaluated in a future work.
None of our healthy subjects had received catheter examinations. Therefore calculations were based on values obtained from the literature.
The velocity-encoded flow measurements were acquired with a two-dimensional technique. Our results therefore might have been influenced by the longitudinal motion of the plane of the valves during the cardiac cycle. Navigator-gated valve-tracking techniques could be one possibility to tackle this problem; however, this technique was not available to us.
Conclusion
Magnetic resonance velocity-encoded flow measurements at the level of the AV valves are feasible and provide a valuable, non-invasive method for the assessment of diastolic dysfunction in patients suffering from CP. In combination with assessment of morphology and cine function, flow measurements help to differentiate between systolic and diastolic dysfunction in patients presenting with heart failure. Calculated tricuspid e- to a-wave ratios correlate with right ventricular end-diastolic pressure measurements and may indicate increased ventricular pressure and conclusions on the severity of diastolic dysfunction may be drawn.
References
Spodick DH (1997) The pericardium: a comprehensive textbook. Marcel Dekker. New York, pp 233–464
Frank H, Globits S (1999) Magnetic resonance imaging evaluation of myocardial and pericardial disease. J Magn Reson Imaging 10:617–626
Talreja DR, Edwards WD, Danielson GK, Schaff HV, Tajik AJ, Tazelaar HD, Breen JF, Oh JK (2003) Constrictive pericarditis in 26 patients with histologically normal pericardial thickness. Circulation 108:1852–1857
Appleton CP, Hatle LK, Popp RL (1988) Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol 12:426–440
Hatle LK, Appleton CP, Popp RL (1989) Differentiation of constrictive pericarditis and restrictive cardiomyopathy by Doppler echocardiography. Circulation 79:357–370
European Study Group on Diastolic Heart Failure (1998) How to diagnose diastolic heart failure. Eur Heart J 19:990–1003
Vigneswaran WT, McDougall JC, Olson LJ, Breen JF, McGregor CG, Rumberger JA (1993) Right ventricular assessment in patients presenting for lung transplantation. Transplantation 55:1051–1055
Hartiala JJ, Mostbeck GH, Foster E, Fujita N, Dulce MC, Chazouilleres AF, Higgins CB (1993) Velocity-encoded cine MRI in the evaluation of left ventricular diastolic function: measurement of mitral valve and pulmonary vein flow velocities and flow volume across the mitral valve. Am Heart J 125:1054–1066
Hartiala JJ, Foster E, Fujita N, Mostbeck GH, Caputo GR, Fazio GP, Winslow T, Higgins CB (1994) Evaluation of left atrial contribution to left ventricular filling in aortic stenosis by velocity-encoded cine MRI. Am Heart J 127:593–600
Mostbeck GH, Hartiala JJ, Foster E, Fujita N, Dulce MC, Higgins CB (1993) Right ventricular diastolic filling: evaluation with velocity-encoded cine MRI. J Comput Assist Tomogr 17:245–252
Heidenreich PA, Steffens J, Fujita N, O'Sullivan M, Caputo GR, Foster E, Higgins CB (1995) Evaluation of mitral stenosis with velocity-encoded cine-magnetic resonance imaging. Am J Cardiol 75:365–369
Helbing WA, Niezen RA, Le CS, van der Geest RJ, Ottenkamp J, de RA (1996) Right ventricular diastolic function in children with pulmonary regurgitation after repair of tetralogy of Fallot: volumetric evaluation by magnetic resonance velocity mapping. J Am Coll Cardiol 28:1827–1835
Rebergen SA, Helbing WA, Van der Wall EE, Maliepaard C, Chin JG, de RA (1995) MR velocity mapping of tricuspid flow in healthy children and in patients who have undergone Mustard or Senning repair. Radiology 194:505–512
Rebergen SA, Niezen RA, Helbing WA, Van der Wall EE, de RA (1996) Cine gradient-echo MR imaging and MR velocity mapping in the evaluation of congenital heart disease. Radiographics 16:467–481
Bauner K, Schoenberg SO, Schmoeckel M, Reiser MF, Huber A (2007) Evaluation of diastolic function in patients with constrictive pericarditis before and after pericardectomy. Radiologe 47:342–349
Rienmuller R (1990) Computerized tomography versus nuclear magnetic resonance tomography in clinical diagnosis of cardiac diseases. Internist (Berl) 31:321–332
Talreja DR, Edwards WD, Danielson GK, Schaff HV, Tajik AJ, Tazelaar HD, Breen JF, Oh JK (2003) Constrictive pericarditis in 26 patients with histologically normal pericardial thickness. Circulation 108:1852–1857
Pattynama PM, Lamb HJ, Van der Velde EA, Van der Wall EE, de Roos A (1993) Left ventricular measurements with cine and spin-echo MR imaging: a study of reproducibility with variance component analysis. Radiology 187:261–268
Giorgi B, Mollet NR, Dymarkowski S, Rademakers FE, Bogaert J (2003) Clinically suspected constrictive pericarditis: MR imaging assessment of ventricular septal motion and configuration in patients and healthy subjects. Radiology 228:417–424
Perkins NJ, Schisterman EF (2006) The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol 163:670–675
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47:458–472
Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK (2004) Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol 43:271–275
Talreja DR, Edwards WD, Danielson GK, Schaff HV, Tajik AJ, Tazelaar HD, Breen JF, Oh JK (2003) Constrictive pericarditis in 26 patients with histologically normal pericardial thickness. Circulation 108:1852–1857
Rubinshtein R, Glockner JF, Feng D, Araoz PA, Kirsch J, Syed IS, Oh JK (2009) Comparison of magnetic resonance imaging versus Doppler echocardiography for the evaluation of left ventricular diastolic function in patients with cardiac amyloidosis. Am J Cardiol 103:718–723
Oh JK, Appleton CP, Hatle LK, Nishimura RA, Seward JB, Tajik AJ (1997) The noninvasive assessment of left ventricular diastolic function with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 10:246–270
Garcia MJ, Smedira NG, Greenberg NL, Main M, Firstenberg MS, Odabashian J, Thomas JD (2000) Color M-mode Doppler flow propagation velocity is a preload insensitive index of left ventricular relaxation: animal and human validation. J Am Coll Cardiol 35:201–208
Ishida Y, Meisner JS, Tsujioka K, Gallo JI, Yoran C, Frater RW, Yellin EL (1986) Left ventricular filling dynamics: influence of left ventricular relaxation and left atrial pressure. Circulation 74:187–196
Choong CY, Abascal VM, Thomas JD, Guerrero JL, McGlew S, Weyman AE (1988) Combined influence of ventricular loading and relaxation on the transmitral flow velocity profile in dogs measured by Doppler echocardiography. Circulation 78:672–683
Bella JN, Palmieri V, Roman MJ, Liu JE, Welty TK, Lee ET, Fabsitz RR, Howard BV, Devereux RB (2002) Mitral ratio of peak early to late diastolic filling velocity as a predictor of mortality in middle-aged and elderly adults: the Strong Heart Study. Circulation 105:1928–1933
Tenenbaum A, Motro M, Hod H, Kaplinsky E, Vered Z (1996) Shortened Doppler-derived mitral A wave deceleration time: an important predictor of elevated left ventricular filling pressure. J Am Coll Cardiol 27:700–705
Giannuzzi P, Imparato A, Temporelli PL, de VF, Silva PL, Scapellato F, Giordano A (1994) Doppler-derived mitral deceleration time of early filling as a strong predictor of pulmonary capillary wedge pressure in postinfarction patients with left ventricular systolic dysfunction. J Am Coll Cardiol 23:1630–1637
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Previtali M, Chieffo E, Ferrario M, Klersy C (2007) Echocardiographic evaluation of left ventricular diastolic function: correlation between echocardiographic and hemodynamic parameters. Minerva Cardioangiol 55:733–740
Yamamoto K, Nishimura RA, Chaliki HP, Appleton CP, Holmes DR Jr, Redfield MM (1997) Determination of left ventricular filling pressure by Doppler echocardiography in patients with coronary artery disease: critical role of left ventricular systolic function. J Am Coll Cardiol 30:1819–1826
Yu CM, Sanderson JE, Chan S, Yeung L, Hung YT, Woo KS (1996) Right ventricular diastolic dysfunction in heart failure. Circulation 93:1509–1514
Zoghbi WA, Habib GB, Quinones MA (1990) Doppler assessment of right ventricular filling in a normal population. Comparison with left ventricular filling dynamics. Circulation 82:1316–1324
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauner, K., Horng, A., Schmitz, C. et al. New observations from MR velocity-encoded flow measurements concerning diastolic function in constrictive pericarditis. Eur Radiol 20, 1831–1840 (2010). https://doi.org/10.1007/s00330-010-1741-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-010-1741-7