Abstract
Objective
Juxta-articular venous malformations (VMs) are uncommon, but may cause early arthropathy of the knee in children and adolescents. We sought to describe the prevalence, extent and initial magnetic resonance imaging (MRI) features of knee arthropathy in children with VM adjacent to the knee joint.
Methods
Thirty-five patients with VM adjacent to the knee who had MRI performed between 2000 and 2009 were identified through a keyword search of the radiology information system.
Results
VM extended to the joint in 17 of the 35 patients (5.4–21.5 years, mean 11.8 years). Most of these 17 patients had joint changes (15/17, 88%), most commonly haemosiderin deposition (14/17, 82%). Other findings included the presence of subchondral bone lesions (eight, 47%), cartilage loss (six, 35%), synovial thickening (six, 35%), marrow oedema (six, 35%), joint effusion (five, 29%), subchondral cysts (five, 29%) and one loose body (6%). VM location and size did not correlate with the degree of articular involvement. Joint changes were present in focal as well as non-discrete VM.
Conclusion
We found that the frequency of arthropathy increased with extension of VM into the joint itself. This finding stresses the importance of early MRI evaluation of all juxta-articular VM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Venous malformations (VMs) of subcutaneous tissue adjacent to joints may extend into the articular tissues, and may be associated with arthropathy. According to the classification of Mulliken and Glowacki [1], VMs are congenital non-neoplastic lesions composed of dysplastic blood vessels with no cell proliferation, which grow proportionally with the patient and do not regress. Clinically they are often blue and easily compressible. VMs have the ability to cross multiple tissue boundaries. Not only the subcutaneous tissue is involved, but muscle groups, tendons, bone cortex and bone marrow may be violated [2–5].
VM is the most common vascular malformation of the extremities and can present in any muscle, but the quadriceps muscle is among those most commonly involved [6]. The clinical presentation depends on the location and size of the lesion and the structures that it involves. A VM may induce pain (the most common symptom), impaired mobility, oedema, ulceration and haemorrhage. VMs may also cause skeletal hypertrophy or remodelling. Physical examination findings alone significantly underestimate the extent of VM in most cases [4, 6, 7]. Magnetic resonance imaging (MRI) better defines the anatomical extent of the lesion and can correlate treatable components of the malformation with patient symptoms [6].
Arthropathy due to recurrent haemarthrosis is one of the most disabling complications of this disease. Fortunately, this only occurs in a subgroup of patients with juxta-articular VM. The aim of this study was to define the MRI features of articular VM and correlate these with arthropathy of the knee at initial MRI. This is intended as a first step to aid in understanding which lesion features are the highest risk for development of arthropathy.
Materials and methods
A retrospective study was performed in a paediatric tertiary care centre. Institutional ethics approval was obtained. Subjects with documented juxta-articular VM of the knee were identified using a radiology information system database keyword search of final radiology reports over a 10-year period (2000–2009). Combinations of the following search words were used: MRI, knee, vascular malformation, VM and lesion. If the subject had undergone more than one MRI examination, only the first set of MRI images was reviewed. A total of 35 patients were identified meeting inclusion criteria for the study. The mean age was 11.0 years (range 0.2–21.5 years). Their MRIs were reviewed in consensus by two paediatric radiologists. Although it was not possible to blind the reviewing radiologists to the original reported findings, the reviewing radiologists used the original report only as a means to identify patients for inclusion into the study.
MR examination
All MRI studies were performed using our routine contrast-enhanced knee protocol on a 1.5-Tesla system (Avanto, Siemens Medical, Erlangen, Germany). The affected knee was imaged in an eight-channel phased array coil or 15-channel transmit receiver coil (TxRx) (Siemens Medical, Erlangen, Germany). The sequences obtained during MRI examination included coronal T1-weighted spin echo (SE T1, TR/TE = 580 ms/14 ms); axial and sagittal fat saturated T2-weighted images (SE T2, TR/TE = 6,080 ms/72 ms); axial, coronal and sagittal fat-saturated PD (TE = 33 ms); three-dimensional (3D) volumetric spoiled gradient echo sequences (T2-GE, TR/TE/flip angle = 37 ms/20 ms/12). No direct arthrogram was performed. IV contrast administration of 0.2 ml/kg of dilute gadopentetate dimeglumine (Magnevist, Bayer Healthcare Pharmaceuticals, Berlin, Germany) was performed in all patients with axial, sagittal and coronal fat- saturated postcontrast T1-weighted images.
Image review
Initial review of the candidate images was performed to ensure MRI findings were compatible with a VM. These findings include cystic spaces or sinusoidal structures with T2 hyperintense signal intensity, presence of bodies of reduced signal due to phleboliths or thrombus, and a central enhancement pattern [8]. All of the patients reviewed had appropriate findings. The images were then reviewed in detail to assess the VM and the adjacent knee joint. The VM was categorised to be discrete if only a focal mass lesion was present or non-discrete if multiple components to the lesion were identified. The volume of the largest defined component of the lesion was measured in cubic centimetres (cm3). The extent of the lesion was categorised as being separate from the joint, reaching the capsule, reaching the synovium, inside the synovium or inside the bone.
For the purpose of this study, the knee was defined to extend from the distal femoral physis to the proximal tibial physis and separated into three parts. The superior third extended from the femoral physis to the inferior aspect of the suprapatellar pouch, the inferior third from the inferior aspect of the synovium of the knee to the tibial physis, the middle third in between the superior and inferior thirds (Fig. 1).
Sagittal fat-saturated T2-weighted MR image demonstrates the extent of the joint parts as defined for the purpose of this study. Superior (S, from the superior aspect of the suprapatellar pouch to the femoral physis), middle (M) and inferior (I, from the inferior aspect of the synovium of the knee to the tibial physis) are defined as illustrated
Simple joint effusions were categorised as small or large, based on whether it extended to all synovial compartments. The presence of haemarthrosis was documented separately from joint effusion. Synovial low-signal haemosiderin deposit was categorised as petechial, becoming confluent or continuous. Synovial hypertrophy was graded to be mild (<2 mm), moderate (2–5 mm) or severe (>5 mm). Chondral lesions were categorised as the presence of focal cartilage MRI signal change or focal cartilage loss. Subchondral bone lesions were categorised as bone marrow oedema, subchondral cyst formation or fragmentation with presence of loose bodies. Degenerative changes of subchondral sclerosis and osteophyte formation and other associated findings were recorded.
Statistical analysis
Basic descriptive statistics and Student’s t-test for comparison of continuous variables were performed where appropriate. A level of significance of p = 0.05 was selected.
Results
VMs
The locations of VMs are summarised in Table 1. There was a wide distribution of the localisation of juxta-articular VMs. Nearly half (46%) of these lesions extend into all three joint parts. VM extension was separate from the synovium in two (6%), abutted the capsule in 12 (34%), abutted the synovium in eight (23%) patients, extended through the synovium in five (14%) and involved the synovium and bone in eight (23%). The mean size of the VM was 7.55 cm3 (range 0.01–62.6 cm3). VM presented as a single, discrete mass in nine patients (26%), as a multifocal lesion in 17 patients (49%) or as diffuse lesions in nine patients (26%).
Arthropathy
Articular extension of VM was seen in 17 patients (49%). In this group, joint changes were identified in 15 (88%) patients. Synovial haemosiderin staining was common (14 patients, 82%) and was petechial in two patients (14%) and confluent in 12 patients (86%). Synovial hypertrophy was present in six patients (35%), small in four patients and moderate in two patients. Haemarthrosis was present in three patients (18%). Joint effusion was identified in five patients (30%), and was small in two patients and large in three. Cartilaginous lesions were identified in seven patients (41%), with cartilage signal change in one patient (6%) and focal loss of cartilage in six patients (35%). Subchondral bone lesions were identified in eight patients (47%), consisting of subchondral cysts in five patients (30%), bone marrow oedema in six (35%) patients and presence of a loose body in one patient (6%). Degenerative changes were identified in one patient (6%). This patient (age 17 years) presented with severe joint space narrowing, subchondral cyst formation and the presence of osteophytes.
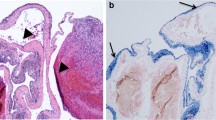
Representative images of several juxta-articular VMs demonstrating the spectrum of articular involvement and arthropathy are presented (Figs. 2, 3, 4, 5).
a,b VM of the right knee in a 2-year-old boy. a Sagittal fat-saturated PD-weighted MR image. A large heterogeneous hyperintense lesion (arrows) is identified abutting into the suprapatellar synovial pouch (thin arrow). There is no evidence of arthropathy. VM of the right knee in a 2-year-old boy. b Contrast-enhanced sagittal fat-saturated T1-weighted MR image. The lesion demonstrates patchy and predominantly central enhancement (arrow)
VM of the left knee in a 15-year-old boy. Axial fat-saturated PD-weighted MR image. A large heterogeneous hyperintense lesion extends along the lateral retinaculum, violates the muscles and the adipose tissue of the popliteal fossa (arrows). A small component of the lesion extends into the lateral joint space and abuts the synovium (short thin arrow). A small joint effusion indicates arthropathy (long thin arrow)
a–c VM of the left knee in a 9-year-old girl. a Axial fat-saturated PD-weighted MR image. A large knee joint effusion is present, extending over all synovial compartments (short arrows). Continuous haemosiderin staining of the synovium is identified (long arrows). VM of the left knee in a 9-year-old girl. b Sagittal fat-saturated PD-weighted MR image. Extension of the lesion from Hoffa’s fat pad posteriorly into the synovium of the knee joint is demonstrated (white arrows). A large knee joint effusion (asterisk) and haemosiderin staining of the synovium (black arrows) are again identified. VM of the left knee in a 9-year-old girl. c Contrast-enhanced axial fat-saturated T1-weighted image. Irregular synovial thickening and enhancement is present (arrows)
a–d VM of the left knee in a 17-year-old girl. a, b Coronal T1- and fat-saturated PD-weighted MR image. T1 and PD signal changes of the lateral femoral condyle and tibial plateau represent subchondral cyst formation and focal bone marrow oedema (arrows). Cartilage loss with joint space narrowing, subchondral cyst formation and the presence of an osteophyte represent degenerative changes (thin arrow). c Sagittal fat-saturated PD-weighted MR image. Subchondral cyst formation and focal bone marrow oedema is identified in the lateral femoral condyle (thick arrows) and proximal tibia (thin arrows). VM of the left knee in a 17-year-old girl. d Axial fat-saturated PD-weighted image. The small VM is centred along the anterior aspect of the knee joint and extends into the synovium
Relationship of the VM with arthropathy to the knee
Extension
VMs that extended deeper into the knee joint were more commonly associated with joint abnormalities than superficial VMs (Table 2). There was no statistical difference in joint involvement in patients with demonstrated focal and non-discrete lesions.
Location
There was poor correlation between the location of the VM and the presence of associated joint changes (Table 3). There is no statistically significant difference in the occurrence of joint involvement in lesions located in only one part of the knee compared with extensive lesions occupying two or all three compartments of the knee.
Size
Arthropathy occurred in small and large VMs (range 0.07–62.6 cm3). The mean size of VM extending into the knee joint (7.86 cm3) was larger than the lesions without articular violation (4.95 cm3); however, given the wide range of lesion sizes this was not statistically significant.
Discussion
Approximately half of the patients (49%) with VM adjacent to the knee joint in this series had intra-articular extension of the lesion, and most of this group (88%) have MRI evidence of arthropathy.
We found that VM location did not predict arthropathy, as joint involvement was demonstrated in all groups. Arthropathy was demonstrated in discrete as well in non-discrete lesions (without focal mass). Further, VM size (from very small to large) was also a poor predictor of joint involvement, as joint violation occurred in small and large VMs without statistically significant difference. Our study found that only the VM depth (i.e. joint involvement) correlated well with presence of arthropathy and thus advocates the use of MRI as a complementary component in the complete evaluation of VMs.
These findings stress the importance of MRI in the detection of early stages of the disease process, when radiographs are normal or show only subtle changes in the appearance of the knee joint. MRI may also provide useful information about the presence, size and location of loose bodies, the underlying cartilage and stability of the osteochondral lesions in articular extension of VM. MRI can characterise the malformations to guide treatment towards percutaneous embolisation in slow-flow vascular malformations [6].
Gadolinium-enhanced sequences are routinely used in the evaluation of VMs. In our study, we found these sequences particularly helpful in distinguishing flow-related signal voids from other causes of signal voids, for the characterisation of the vascular malformations, for the assessment of synovial hypertrophy and in defining the synovial extent of the VM. Furthermore, the typical central enhancement pattern with the absence of hypertrophied feeding arteries and enlarged draining veins may differentiate articular extension of VM from other articular vascular tumours such as synovial haemangioma, and arterial and arteriovenous malformations [9].
Arthropathy of the knee due to a VM is rare and the mechanism of joint destruction has not been clearly identified. Based on our image review, we postulate two mechanisms of joint destruction. First, direct focal extension into the joint with focal destruction of cartilage and subchondral bone. Second, joint destruction from inflammation due to recurrent articular haemorrhage. The latter mechanism appears similar to the changes seen in haemophilic arthropathy, with synovial thickening and haemosiderin deposits initiating the inflammatory changes leading to arthropathy [10, 11].
Our study has several limitations. It is a retrospective review with a relatively small sample size, which is an unavoidable consequence of the rarity of these lesions. The study design was further limited by the fact that the study population was based on radiology report text word searches. We did not have surgical/pathological correlation of extent of lesions or arthropathy, and no longitudinal follow-up was performed. The estimated prevalences are subject to referral bias. Some patients in our population may have had a juxta-articular VM that referring clinicians felt did not warrant MRI, and others may have been imaged but not captured in our keyword search of our imaging database. However, the wide range of lesions imaged (from very small to large) suggests the likelihood of a low clinical threshold for referral, and our keyword search was as exhaustive as was practical.
Conclusion
There is a high prevalence (nearly 50%) of intra-articular extension of VMs, and a strong association of these deep lesions with arthropathy (nearly 90%), often with haemosiderin deposition indicating bleeding into the joint. There is poor correlation between the size and location of the VM and associated joint changes. We found that the frequency of arthropathy increases with increasing extension of the VM into the joint. This finding stresses the importance of MRI evaluation of all juxta-articular VMs to identify possible associated arthropathy, which may be important in determining the timing and aggressiveness of therapy.
References
Mulliken JB, Glowacki J (1982) Haemangiomas and vascular malformations in infants and children based on endothelial characteristics. Plast Reconstr Surg 69:412–422
Donelly LF, Adams DM, Bisset GS (2000) Vascular Malformations and haemangiomas: A practical approach in a multidisciplinary clinic. AJR Am J Roentgenol 174:597–608
Breugem CC, Maas M, Reekers JA, van der Horst CAM (2001) Use of magnetic resonance imaging for the evaluation of vascular malformations of the lower extremity. Plast Reconstr Surg 108:870–877
Rinker B, Karp NS, Margiotta M, Blei F, Rosen R, Rofsky NM (2003) The role of Magnetic Resonance imaging in the Management of Vascular Malformations of the trunk and extremities. Plast Reconstr Surg 112:504–510
Theruvil B, Kapoor V, Thalava R, Nag HL, Kotwall PP (2004) Vascular malformation s in muscles around the knee presenting as knee pain. Knee 11:155–158
Fayad L, Harizolan T, Bleumke D, Mitchell S (2006) Vascular malformations in the extremities: emphasis on MR imaging features that guide treatment options. Skeletal Radiol 35:127–137
Abernethy LJ (2003) Classification and imaging of vascular malformations in children. Eur Radiol 13:2483–2497
Puig S, Casati B, Staudenherz A, Paya K (2005) Vascular low-flow malformations in children: current concepts of classification, diagnosis and therapy. Eur J Radiol 53:35–45
Moukaddam H, Pollak J, Haims AH (2009) MRI characteristics and classification of peripheral vascular malformations and tumors. Skeletal Radiol 38:535–547
Dobon M, Lucia JF, Aguilar C et al (2003) Value of magnetic resonance imaging for the diagnosis and follow-up of haemophilic arthropathy. Haemophilia 9:76–85
Pergantou H, Matsinos G, Papadopoulos A et al (2006) Comparative study of clinical, X-ray and magnetic resonance imaging in evaluation and management of haemophilic arthropathy in children. Haemophilia 12:241–247
Acknowledgements
The research was supported by the 2009 research grant of the Royal Belgian Radiology Society (RBRS).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jans, L., Ditchfield, M., Jaremko, J.L. et al. MRI demonstrates the extension of juxta-articular venous malformation of the knee and correlates with joint changes. Eur Radiol 20, 1792–1798 (2010). https://doi.org/10.1007/s00330-010-1733-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-010-1733-7