Abstract
Objective
To compare the outcome of patients affected by biliary leak after major biliary surgery and treated with percutaneous transhepatic biliary drainage (PTBD) alone with that of similar patients treated with PTBD and concurrent positioning of an occlusion balloon (PTBD-OB).
Methods
We retrospectively reviewed the results of the use of PTBD or PTBD-OB performed at our institution from 2004 to 2008 in patients with post-surgical biliary leak. Sixteen patients entered the evaluation. PTDB alone was performed in 9 men (age 59.7 ± 13.4 years [mean ± standard deviation]; median 60 years), while PTBD-OB was performed in 7 patients (5 men, 2 women, age 71.3 ± 9.3 years; median 68 years).
Results
No significant difference between groups was found regarding age (p = 0.064) and sex (p = 0.175) distribution, number of procedures (3.1 ± 1.62; 2 vs 1.7 ± 1.1; 1, p = 0.151), and days of disease before recovery, death or modification of treatment (51.6 ± 66.8; 23 vs 18.6 ± 15.1; 14, p = 0.266). The number of patients treated with PTBD-OB who fully recovered (7/7, 100%) was significantly higher than that of patients treated with PTBD alone (4/9, 44%, p = 0.034).
Conclusion
This procedure appears to be clinically effective, being associated with a higher probability of recovery in patients treated for post-surgical biliary leak. Further studies are needed to confirm these preliminary results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary leaks represent an important complication of several surgical procedures, such as cholecystectomy, duodenocephalopancreasectomy (Whipple’s procedure) and liver transplant [1]. These occurrences could determine relevant clinical problems, such as biliary peritonitis and sepsis [2], and are currently considered to be among the major causes of prolonged hospitalisation and post-surgical death [1, 3, 4].
Surgical repair and endoscopic management were proven to be effective in the treatment of biliary leaks [1]. For surgical re-intervention, postoperative mortality could reach 70% [2, 3], whereas endoscopic management represents the treatment of choice, being effective and less invasive [5–7]. However, following a Billroth II gastrectomy or Roux-en-Y bilio-enteric reconstruction, the postoperative anatomy makes the endoscopic treatment impossible to perform [8–10]. In these patients, percutaneous transhepatic biliary drainage (PTBD) has been proven to be an effective tool in the treatment of biliary leakage [8–10].
The occlusion balloon (OB) is a device built to interrupt the flow within a vessel and is currently used in interventional procedures, such as selective angiography, vascular pre-surgical occlusion and control of acute haemorrhage [11]. To our knowledge, OB have never been used in the treatment of biliary leaks. The aim of using such devices during biliary interventional procedures is to avoid contact between bile and the fistula and thereby to promote the healing process.
The purpose of our work was to retrospectively compare the outcome of patients affected by biliary leakage after major biliary surgery and treated with percutaneous transhepatic biliary drainage (PTBD) alone with that of patients affected by the same condition and treated with PTBD and a concurrent OB positioning (PTBD-OB).
Materials and methods
Patients
Institutional review board approval was obtained and patients’ informed consent was waived. We retrospectively reviewed our case series of patients who attended our institution between January 2004 and July 2008 for the treatment of a postoperative biliary leak that could not be managed by endoscopy.
The diagnosis of biliary leak was obtained according to clinical parameters (body temperature, leukocytosis, abdominal pain, peritonitis and sepsis), the presence of bile in surgical drainage or the evidence of fluid collection on imaging studies [1].
All patients underwent percutaneous transhepatic cholangiography (PTC) performed by one of three interventional radiologists with more than 10 years’ experience. During the same procedure, PTBD was positioned.
Sixteen patients were included in our series. They were 14 men and 2 women, aged 64.5 ± 12.9 years (mean ± standard deviation), with a median of 65.5 years. PTBD alone was positioned in 9/16 patients (9 male, age 59.7 ± 13.4 years; median 60 years). Among these, two patients who did not respond to the procedure were treated with a delayed positioning of an OB. Seven out of sixteen patients (5 males, 2 females, age 71.3 ± 9.3 years; median 68 years) were treated with a PTBD and concurrent positioning of an OB (PTBD-OB). All patients had non-dilated bile ducts. Demographics, basic disease, surgical procedure, site of fistula, and data regarding biliary leak treatment of the 16 patients are summarised in Table 1.
PTBD and OB technique
All patients were given a broad-spectrum antimicrobial therapy (ciprofloxacin 500 mg/day by mouth), beginning on the day of the procedure; this was maintained for at least 10 days.
PTBD was positioned after injection of local anaesthetic (lidocaine or carbocaine without adrenaline, 2%) within the subcutaneous tissue and on Glisson’s capsule. The puncture of the biliary ducts was performed through a right or left intercostal percutaneous approach under fluoroscopic or ultrasonographic guidance. Since patients had non-dilated intrahepatic bile ducts, an initial puncture was performed close to the hilum where the ducts are bigger. There, a small amount of iodinated contrast (iomeprol 300 mg/ml, Iomeron 300, Bracco, Italy) was injected to opacify the biliary tree and to allow one to puncture a peripheral duct. Then, a 0.18-inch microguide wire was advanced through the biliary system and later substituted by a conventional 0.35-inch angiographic guide by means of a micropuncture conversion system (Accustick, Boston Scientific, Natich, MA, USA). Next, an 8-Fr internal-external biliary drainage catheter was inserted (Flexima, Boston Scientific, Natick, MA, USA) with two series of side holes separated by a blind segment. The upper series of holes was specifically cut by the operator according to the location of the leak as shown on PTC. The tip of the drainage catheter was positioned deeper to the bilio-enteric anastomosis in order to have the upper series of holes above the leak and the lower series of holes below the leak to obtain a complete exclusion of the leakage. In some patients with thicker bile, the drainage catheter was later substituted with a 10- to 12-Fr catheter during follow-up.
In 7/16 patients who underwent a PTBD-OB procedure, two guides were inserted into the same intrahepatic biliary duct. Over a first guide, an OB (10 or 12 mm, according to the dimension of the biliary ducts; standard occlusion balloon catheter, Boston Scientific, Natick, MA, USA or Admiral extreme, Invatec, Switzerland) was inserted, positioned above the biliary leak and then inflated. The correct maintenance of the inflation of the OB was assured by the positioning of a high pressure stopcock (Smiths Medical Deutschland GmbH, Kirchseeon, Germany) at the free end of the catheter. Later, a drainage catheter was inserted over the second guide wire and positioned above the OB. In those patients who underwent delayed positioning of an OB, the previously positioned PTBD was removed and a PTBD-OB procedure was performed in the same session.
In the case of displacement or obstruction of the drainage or deflation of the OB with the persistence of a biliary leak, patients underwent a new procedure to reposition the device. Days of disease before recovery were considered starting from the first OB positioning. Flushing of the catheter with sterile saline was routinely performed twice a day. After positioning of the catheters, cholangiographic controls were carried out to check the evolution of the fistula.
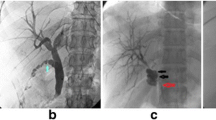
Two examples of PTBD-OB procedure are shown in Figs. 1 and 2.
Use of an occlusion balloon for treating a biliary leak. a Percutaneous transhepatic cholangiography showing the biliary tree (BT), the bilio-digestive anastomosis (white arrow) and the presence of contrast in the bowel (B). A contrast leakage (asterisk) is clearly visible, dripping from left-sided biliary leak (black arrow). b The balloon is positioned into the bile duct above the leak (large arrowheads radiopaque markers of the balloon) and distended with saline solution (small arrowheads balloon right profile); BT biliary tree; B bowel. c During follow-up, the balloon (large arrowheads radiopaque markers) got displaced in the bowel (B) and recurrence of the leakage (asterisk) occurred, dripping again from the left-sided biliary leak (black arrow); white arrow bilio-digestive anastomosis; BT biliary tree. d At the end of the treatment, complete healing of the leak is demonstrated, with contrast confined within biliary tree (BT) and bowel (B)
Biliary leak after duodenocephalopancreasectomy treated with occlusion balloon technique. a The leak (black arrow) arises at the dead end of the bowel stump (B), dripping a large amount of contrast (asterisks) along the right paracolic gutter. BT biliary tree; white arrow bilio-digestive anastomosis. b Positioning of the balloon (large arrowheads radiopaque markers; small arrowheads balloon left profile) above the bilio-digestive anastomosis (white arrow); BT biliary tree; B bowel. c During follow-up, the balloon (arrowheads radiopaque markers) got displaced in the bowel (B) and large recurrence of the leakage (asterisks) occurred, dripping again from the dead end (black arrow) of the bowel stump; white arrow bilio-digestive anastomosis. d Final result with complete healing of the leak and absence of contrast leakage (asterisk); BT biliary tree; white arrow bilio-digestive anastomosis; B bowel stump
For each patient, the type of interventional procedure, the number of procedures and the number of days of disease before recovery were recorded (see Table 1).
Statistical analysis
Patients who underwent PTBD and, later, a PTBD-OB procedure, were considered part of the PTBD group, because the first PTBD could have influenced in some way the outcome of the PTBD-OB procedure.
Patient age at entry and days of disease before recovery of PTBD patients were compared with those of PTBD-OB patients using the Mann–Whitney U test. Sex distribution and number of recovered patients of the PTBD group were compared with those of the PTBD-OB group using the Fisher’s exact test. Number of procedures performed on PTBD patients were compared with those performed on PTBD-OB patients by using the χ 2 test.
For statistical analyses, SPSS software version 17 (SPSS, Chicago, IL) was used. A P value equal to or less than 0.05 was considered significant.
Results
PTC and PTBD and OB positioning were successful in all cases. No immediate major or minor complications occurred. In all patients, no surgical re-intervention was needed for bile leak treatment.
Among the nine patients included in the PTBD group, three died before healing of the fistula could be demonstrated (see Table 1), one had a persistent leak for up to 31 days and one had a persistent leak for up to 187 days. In these two patients, a positioning of a PTBD-OB allowed complete recovery of the leak to be obtained (see Table 1).
In three patients included in the PTBD-OB group, the cholangiographic controls demonstrated an incomplete obstruction of the main biliary duct because of displacement or deflation of the balloon. In these patients, the OB was re-inflated or repositioned.
Results regarding comparison between PTBD and PTBD-OB groups for age and sex distribution, number of procedures, days of disease before recovery, number of deaths, modification of treatment and number of patients who fully recovered are shown in Table 2.
Discussion
Our experience demonstrated that the combined use of external drainage and an OB in the treatment of post-surgical biliary leaks leads to the recovery of a number of patients that is significantly higher compared with the use of PTBD alone. In addition, the mean recovery time of patients treated with PTBD-OB was lower than that of patients treated with PTBD alone.
Bile leakage may complicate any procedure involving bilio-enteric anastomosis [1] and is associated with significant morbidity and mortality [9]. The incidence of bile leakage is extremely variable, in particular according to the type of surgery: it ranges between 0.1 and 1.4% in cases of cholecystectomy [12], with higher percentages in the case of laparoscopic surgery, 0.4% and 3% in patients who underwent duodenocephalopancreasectomy [13–16] and reaches up to 2.5% or 8% in patients who underwent liver resection [17] or transplantation [4, 18], respectively. Biliary leaks after major hepatobiliopancreatic surgery are considered among the most important causes of prolonged hospitalisation and postoperative death [8, 10]. In their series of 856 liver transplants from living donors, Kim et al. [9] reported 19% of leak-related deaths in patients who developed this complication.
In the past, biliary leaks were treated with surgery. More recently, less-invasive procedures, such as papillosphincterotomy, endoscopic stent positioning in conjunction with PTBD [5–7], or CT- or ultrasound-guided percutaneous positioning of drainages [8–10] allowed the number of surgical treatments, the length of hospitalisation and mortality to decrease. PTBD, however, may represent the only access to the biliary system in certain conditions, such as after Roux-en-Y bilio-enteric reconstruction, where endoscopy is not feasible [1, 18–21]. It must be underlined that patients with biliary leaks have non-dilated biliary ducts, making the percutaneous approach more difficult.
Potential risks of PTBD treatment of biliary leaks include minor (biloma, transitory haemobilia, cutaneous haematomas, and obstruction, displacement or rupture of the drainage) and major complications (sepsis, haemorrhage, fistulas, abscesses, peritonitis, cholangitis and pseudo-aneurysms) [22]. An overall incidence of 10% of such complications has been reported [22]. Weber et al. [23] studied a series of 419 consecutive patients treated with PTBD positioning, reporting an overall incidence of complications that was double in patients with non-dilated biliary ducts compared with patients with dilated biliary ducts (14.5% vs 6.9%, respectively) and an incidence of major complications that was four times lower in the latter group (8.4% vs 2.1%).
The positioning of an OB produces a compression on the wall of the bile duct into which it is inserted. Therefore, the balloon could theoretically favour ulceration or mucosal necrosis of the duct itself. To the best of our knowledge, no data on such a complication have been published and we did not observe such an occurrence in any patient of our series.
Currently, at our Institution, PTBD positioning is the treatment of choice for patients with biliary leakage that cannot be treated endoscopically. The rationale of percutaneous biliary drainage is to reduce the pressure on the leak and to avoid the contact of bile with bilio-enteric anastomosis in order to facilitate cicatrisation. In this setting, the positioning of an angioplastic balloon proximal to the anastomosis produces an immediate interruption of bile flow that in turn could help to reduce the leakage duration. To our knowledge, no other authors have described a similar technique.
In our experience, the positioning of PTBD was possible in all cases (16/16, 100%) and was never associated with major or minor complications. In the group treated with PTBD alone, three patients died of causes that were not related to the procedure, but all three were still affected by biliary leak and were therefore considered not recovered. However, it is reasonable to suppose that patient 14 would not have recovered after 147 days of leakage. The same thing cannot be hypothesised for patients 1 and 2. In two patients where PTBD alone was not effective in the treatment of the leak, our technique allowed a relatively prompt recovery. In particular, patient 9, whose leak persisted for 187 days, experienced recovery after 11 days and the positioning of two PTBD-OB. In patient 5 we decided to position a PTBD-OB only 31 days after the first positioning of PTBD alone, because of an unmodified radiological appearance of the leak. This solution allowed a complete recovery after 60 days.
We did not find a significant difference in the number of procedures and days of disease before recovery between patients treated with PTBD alone and those treated with PTBD-OB, which can reasonably be ascribed to the small sample size of patients. However, we can underline that patients treated with PTBD-OB showed a lower mean time of recovery than patients treated with PTBD alone (18.6 ± 15.1 days, median 14 days vs 51.6 ± 66.8, median 23 days). The positioning of an OB was effective in 7/7 patients (100%) treated with such a technique, compared with 4/9 patients (44%) who recovered with the positioning of PTBD alone (p = 0.034). However, this result should be tempered by the presence of three patients who died, who were considered non-recovered. In Table 3, we report data obtained by a review of the literature on the treatment of biliary leaks by positioning of a PTBD. Among 13 papers, only eight report a series of more than ten patients and only three more than 20 patients. The results of our experience are coherent with data reported in literature.
Several limitations of our study should be taken into account, the first of which was the low number of patients (16, only seven with PTBD-OB positioning). Even though the number of patients is not dissimilar to those reported by other authors (see Table 3)—most patients are treated endoscopically—the current study should be considered as only a preliminary report in favour of the PTBD-OB technique.
The second limitation was that patients were not randomised for the inclusion in the PTBD alone group or the PTBD-OB group. In addition, our analysis was conducted on patients suffering from different afflictions who underwent different types of surgery and whose fistulas were affecting different anatomical structures with variable consistency. However, both groups were homogeneous with regard to age and sex distribution, making the comparison somewhat more reliable.
The third limitation was that the critical status of our patients, often hospitalised in intensive therapy units, did not allow a radiological follow-up at regular time points. Therefore, data regarding days of disease refer to the first radiological control available, giving a potential overestimation of the duration of existence of the fistulas. In addition, the difficult management of these patients led to a deflation or a displacement of the balloon in 3/7 cases (43%), thus increasing the duration of existence of the fistula. A complete occlusion of the biliary duct does not allow cholangiographic control of the leakage. For this reason, the balloon must be deflated to demonstrate the persistence or healing of the leak. However, these limitations partially strengthen the validity of our work because the PTBD-OB procedure compared favourably with the positioning of PTBD alone.
In conclusion, the positioning of an OB to obstruct the biliary duct could represent a new option in the treatment of persistent biliary leaks. Such a technique seems to be more effective in the treatment of postoperative biliary leaks compared with the positioning of PTBD alone. The PTBD-OB technique seems to be safe, effective and without complications when performed in patients with non-dilated biliary ducts. However, further investigations are required to confirm these preliminary results.
References
Zyromski NJ, Lillemoe KD (2006) Current management of biliary leaks. Adv Surg 40:21–46
Pace RF, Blenkharn JI, Edwards WJ et al (1989) Intra-abdominal sepsis after hepatic resection. Ann Surg 209:302–306
Lam CM, Lo CM, Liu CL et al (2001) Biliary complications during liver resection. World J Surg 25:1273–1276
Righi D, Franchello A, Ricchiuti A et al (2008) Safety and efficacy of the percutaneous treatment of bile leaks in hepaticojejunostomy or split-liver transplantation without dilatation of the biliary tree. Liver Transpl 14:611–615
Kaffes AJ, Hourigan L, De Luca N et al (2005) Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc 61:269–275
Sandha GS, Bourke MJ, Haber GB et al (2004) Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc 60:567–574
Lee CS, Liu NJ, Lee CF et al (2008) Endoscopic management of biliary complications after adult right-lobe living donor liver transplantation without initial biliary decompression. Transplant Proc 40:2542–2545
Cozzi G, Severini A, Civelli E et al (2006) Percutaneous transhepatic biliary drainage in the management of postsurgical biliary leaks in patients with nondilated intrahepatic bile ducts. Cardiovasc Intervent Radiol 29:380–388
Kim JH, Ko GY, Sung KB et al (2008) Bile leak following living donor liver transplantation: clinical efficacy of percutaneous transhepatic treatment. Liver Transpl 14:1142–1149
Baker TA, Aaron JM, Borge M et al (2008) Role of interventional radiology in the management of complications after pancreaticoduodenectomy. Am J Surg 195:386–390
Yang JH, Shih JC, Liu KL et al (2007) Combined treatment with temporary intraoperative balloon occlusion of common iliac arteries and hysteroscopic endocervical resection with postoperative cervical balloon for intractable cervical pregnancy in an infertile woman. Fertil Steril 88:1438.e11–1438.e13
Karvonen J, Gullichsen R, Laine S et al (2007) Bile duct injuries during laparoscopic cholecystectomy: primary and long-term results from a single institution. Surg Endosc 21:1069–1073
Winter JM, Cameron JL, Yeo CJ (2008) Duodenojejunostomy leaks after pancreaticoduodenectomy. J Gastrointest Surg 12:263–269
Grobmyer SR, Pieracci FM, Allen PJ (2007) Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg 204:356–364
Yeo CJ, Cameron JL, Sohn TA et al (1997) Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg 226:248–257
Vin Y, Sima CS, Getrajdman GI et al (2008) Management and outcomes of postpancreatectomy fistula, leak, and abscess: results of 908 patients resected at a single institution between 2000 and 2005. J Am Coll Surg 207:490–498
Jarnagin WR, Gonen M, Fong Y et al (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 236:397–406
Aytekin C, Boyvat F, Harman A (2007) Percutaneous management of anastomotic bile leaks following liver transplantation. Diagn Interv Radiol 13:101–104
Ernst O, Sergent G, Mizrahi D (1999) Biliary leaks: treatment by means of percutaneous transhepatic biliary drainage. Radiology 211:345–348
Sohn TA, Yeo CJ, Cameron JL et al (2003) Pancreaticoduodenectomy: role of interventional radiologists in managing patients and complications. J Gastrointest Surg 7(2):209–219
Kaufman SL, Kadir S, Mitchell SE et al (1985) Percutaneous transhepatic biliary drainage for bile leaks and fistulas. AJR Am J Roentgenol 144:1055–1058
Burke DR, Lewis CA, Cardella JF et al (2003) Society of interventional radiology standards of practice committee. quality improvement guidelines for percutaneous transhepatic cholangiography and biliary drainage. J Vasc Interv Radiol 14:S243–S246
Weber A, Gaa J, Rosca B et al (2008) Complications of percutaneous transhepatic biliary drainage in patients with dilated and nondilated intrahepatic bile ducts. Eur J Radiol. Epub Oct 14. doi:10.1016/j.ejrad.2008.08.012
Smith AC, Shapiro RH, Kelsey PB et al (1986) Successful treatment of nonhealing biliary-cutaneous fistulas with biliary stents. Gastroenterology 90:764–769
Vaccaro JP, Dorfman GS, Lambiase RE (1991) Treatment of biliary leaks and fistulae by simultaneous percutaneous drainage and diversion. Cardiovasc Intervent Radiol 14:109–112
Trerotola SO, Savader SJ, Lund GB et al (1992) Biliary tract complications following laparoscopic cholecystectomy: imaging and intervention. Radiology 184:195–200
Hunt JA, Gallagher PJ, Heintze SW et al (1997) Percutaneous microcoil embolization of intraperitoneal intrahepatic and extrahepatic biliary fistulas. Aust NZ J Surg 67:424–427
Funaki B, Zaleski GX, Straus CA et al (1999) Percutaneous biliary drainage in patients with nondilated intrahepatic bile ducts. AJR Am J Roentgenol 173:1541–1544
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pedicini, V., Poretti, D., Mauri, G. et al. Management of post-surgical biliary leakage with percutaneous transhepatic biliary drainage (PTBD) and occlusion balloon (OB) in patients without dilatation of the biliary tree: preliminary results. Eur Radiol 20, 1061–1068 (2010). https://doi.org/10.1007/s00330-009-1637-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1637-6