Abstract
The purpose was to assess osteoporotic vertebral fractures and other spinal lesions in sagittal reformations obtained from routine multidetector computed tomography (MDCT) studies of the thorax and abdomen, to compare sagittal reformations with axial images in detecting these lesions and to investigate how frequently they were missed in the official radiology report. Routine abdominal or thoracoabdominal MDCT using a standard protocol was performed in 112 postmenopausal women. Axial images and sagittal reformations were analyzed separately by two radiologists in consensus and were compared in order to evaluate how often spinal lesions could be detected. In addition the official radiology reports were assessed to determine how many of those abnormalities were identified. Spine abnormalities were visualized in 101/112 postmenopausal women. In 27 patients osteoporotic vertebral deformities were found; 6 of these were shown in the axial images, but none of these were diagnosed in the official radiology report. Additional abnormalities included degenerative disc disease, osteoarthritis of the facet joints, scoliosis, hemangiomas and bone metastases. In only 9/101 patients spine abnormalities were mentioned in the radiology report. Sagittal reformations of standard MDCT images provide important additional information on spinal abnormalities; in particular, osteoporotic vertebral deformities are substantially better detected.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent studies have demonstrated that osteoporotic vertebral deformities are underdiagnosed and insufficiently reported by radiologists in standard radiological exams [1, 2]. Gehlbach et al., for example, found a prevalence for moderate to severe vertebral fractures of 14.1% in postmenopausal women older than 60 years diagnosed in lateral chest radiographs, yet only half of the official radiology reports documented these fractures [2]. As this underdiagnosis led to substantial undertreatment of patients with osteoporosis, the International Osteoporosis Foundation (IOF) in conjunction with the Osteoporosis Group of the European Skeletal Society of Radiology (ESSR) started an international teaching initiative [3]. The aim was to familiarize and sensitize radiologists to osteoporotic vertebral fractures. Our study extends this concept from standard radiographs to abdominal and thoracic multidetector CT studies, which visualize the spine, providing high quality sagittal reformations, yet so far were not used on a routine basis to diagnose vertebral osteoporotic fractures.
With an extended life expectancy, osteoporosis-related fractures are becoming an increasing health problem [4–6]. Women have an individual lifetime risk of about 40–50% to suffer from an osteoporotic fracture. This risk increases as society ages [7]. In this context, vertebral fractures are of special importance [2]. They are the most common osteoporotic fracture, but often remain undetected because they are frequently asymptomatic. The individual subject with a prevalent fracture has a three- to five-fold risk for future fractures leading to disability and increased mortality [8]. Because these and other fractures can be significantly reduced with appropriate treatment, early recognition and diagnosis are of particular importance.
Multidetector CT (MDCT) currently is standard in many countries; this technique provides thin-section visualization of the chest and abdomen, making high-quality sagittal reconstructions of the spine feasible. Previously obtained standard axial 5-mm slices were not suited to detect osteoporotic deformities [9]. With recent advances in MDCT technology, large volumes of the patient can be covered during a short data acquisition, and small collimations can be used without adding radiation dose [10]. From these raw data, well-resolved multiplanar reformations can be obtained, in case of the most recent scanners even without first creating additional thin-section axial images.
The purpose of this study was (1) to assess the prevalence of osteoporotic vertebral fractures and additional spinal abnormalities visualized using sagittal reformations obtained from routine MDCT studies of the thorax and abdomen, (2) to investigate how frequently these abnormalities could be detected on the axial sections and (3) how frequently they were missed in the official radiology reports.
Materials and methods
Study population
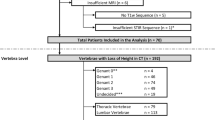
The study population consisted of 112 consecutive women aged 55 years and older who underwent a routine abdominal or thoracoabdominal MDCT at our institution in a 6-month period. The age range in these patients was 55 to 87 years, and the average age was 67.4±8.2 years. Patients with a suspected or known history of bone marrow disease other than osteoporosis were excluded from this study. This included patients with multiple myeloma and renal osteodystrophy, for example.
MDCT imaging
All CT studies were performed with a 16-row MDCT system (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) using a standard protocol with a collimation of 16×0.75 mm, 200 mAs and 120 kVp. From these raw data, images were reconstructed with a slice thickness of 1 mm and an increment of 0.8 mm. The axial images were transferred to a Leonardo workstation (Siemens Medical Solutions), and sagittal reformations of the thoracic and lumbar spine were acquired with a slice thickness of 3 mm.
Time required to perform sagittal reconstructions was about 2 min, consisting of processing (1 min) and transferring (40 s) the axial images and creating the reformations (20 s). Of note, in more recent CT systems, where sagittal reformations can be obtained directly from the raw data, this whole process just takes about 20 s.
Image analysis
Two experienced radiologists reviewed the axial images and the sagittal reformations of the thoracic and lumbar spine in consensus, blinded to age and clinical information. All images were reviewed on a standard PACS workstation in random order with dual, high-resolution, high-brightness monitors. Brightness, contrast, magnification and measurement features were individually adjusted in each imaging study.
First axial images were analyzed for signs of a vertebral fracture, including fracture lines, visualization of the posterior parts of the vertebra across more sections than the anterior parts, suggesting wedge deformity and pathologically increased diameter. Based on these findings a vertebra was classified as fractured or not fractured.
In addition, other spinal diseases, such as degenerative disc disease, osteoarthritis of the facet joints, scoliosis, hemangiomas and bone metastases, were identified.
Subsequently, the sagittal reformations were reviewed in a random order, and osteoporotic fractures were graded using the Spinal Fracture Index (SFI) previously described by Genant et al. [11]. According to the semiquantitative (SQ) classification, deformities with greater than 20% height reduction are defined as fractures. Grade I fractures are defined as a deformity with a reduction in vertebral height ranging from 20–25%, grade II from 25–40%, and grade III fractures show deformities of more than 40% height reduction. Originally the SFI was used for lateral spine radiographs; however, recently it was also introduced to grade vertebral fractures in sagittal reformations of MDCT images [9]. On the sagittal reformations also reduced disc height, osteophytes and increased sclerosis of the facet joints along with hypertrophy and osteophytes were recorded as signs of degenerative disk and facet joint disease.
Retrospective analysis of radiology reports
After all images had been analyzed, the original CT reports were reviewed concerning description of vertebral fractures and other lesions of the spine. All of these reports originated from board-certified radiologists of the Department of Radiology.
Data analysis
Descriptive statistics are provided for the study population. The prevalence of vertebral fractures and other spine abnormalities are given in frequency distributions. Comparisons of proportions were calculated using the Fisher's exact test and the chi-square test. The level of significance was set to p<0.05 for the whole study.
Results
Forty-three abdominal and 69 thoracoabdominal MDCT examinations were studied. Abdominal examinations included the whole lumbar spine up to T10/11, and thoracoabdominal examinations included the whole lumbar and thoracic spine. In most of the patients, MDCT (110/112) was performed for malignancy evaluation. Nineteen women were examined for the primary diagnosis and staging of a tumor, and 42% (8/19) presented with metastases. In addition 91 patients were examined for follow-up of a malignant disease with a prevalence of 70% (64/91) for metastatic tumors. One patient was studied for the exclusion of an intraperitoneal abscess and one for the assessment of a retroperitoneal hematoma (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Table 1, Table 2).
Osteoporotic deformities
The prevalence of osteoporotic deformities in our study population was 24% (27/112) with 15% (17/112) of the patients showing a single fracture and 9% (10/112) having more than one osteoporotic vertebral deformity. Thirty of those osteoporotic spine fractures showed a mild (grade 1), 10 a moderate (grade II) and 8 a severe deformity (grade III). Only a mild deformity was found in 14 patients compared to 13 postmenopausal women with a grade II or grade III fracture (Table 2).
There was a trend to an increase of fracture prevalence with age: 17% (9/53) of the patients were under age 65 and 31% (18/59) aged 65 and older (p>0.05). However, a significant difference of the older versus the younger patients was only demonstrated for the women aged 75–87 years with 53% (15/28) fracture prevalence. According to their SQ grade, there was no significant age difference between patients with a mild deformity compared to the postmenopausal women with a moderate or a severe vertebral fracture (p>0.05). The frequency distribution of the 48 osteoporotic spine fractures concerning the location is given in Fig. 2.
On the axial images only one moderate (1/10) and five severe deformities (5/8) could be detected that were visualized on the sagittal reformations. These were diagnosed on the axial images based on findings consistent with fracture lines and retropulsion of the posterior elements along with increased sagittal diameter suggestive of deformity (Fig. 3). As expected and taking all fracture grades into account, diagnosis of vertebral fractures in the axial sections was substantially limited and worse compared to the sagittal reformations (Fig. 4 and Table 2). Only severe fractures (grade 3) were not significantly (p>0.05) better recognized in the sagittal images. In none of the 27 patients with osteoporotic spine fractures in this study were the deformities described in the report of the MDCT examinations.
Other spinal abnormalities
Using axial images and sagittal reformations, spinal disease was visualized in 101 of the 112 postmenopausal women as shown in Fig. 1 and Table 1. As expected, a high percentage of degenerative changes was found in the elderly study population: 86 patients showed degenerative disc disease (reduced disc height and spondylophytes/osteophytes), 80 osteoarthritis of the facet joints (increased sclerosis and osteophytes), 3 patients demonstrated haemangiomas and 4 patients bone metastases (Fig. 1 and Table 2). Reduced disc height and scoliosis were significantly better depicted in the sagittal reformations (Table 2). The detection of hemangiomas, bone metastases and osteoarthritis of the facet joints was comparable for the axial images and the sagittal reformations. In 28 patients scoliosis was diagnosed as evidenced by rotation of the vertebrae in the axial images. The official radiology reports only described spinal problems in 9 of the 112 patients: in 4 patients osteoarthritis of the facet joints and/or degenerative disc disease was described, in 1 patient scoliosis and in 1 a hemangioma and in 3 postmenopausal women bone metastases. Using odds ratios no significant association between the risk for vertebral fractures and degenerative disc disease or osteoarthritis of the facet joints could be calculated.
Discussion
In this study using routine MDCT examinations in postmenopausal women aged 55 or older, osteoporotic vertebral fractures were diagnosed in 24% (27/112) of the patients. None of these fractures were mentioned in the original radiology report, and only in six patients could fractures be detected retrospectively in the axial images. Sagittal reformations therefore clearly are an essential component of the CT exam in subjects at risk for osteoporosis.
The prevalence rate of 24% for spine fractures found in this study is in the range compared to that found in previous studies involving Caucasian women of similar age groups (14–25%) [2, 12–14]. Of note, however, the presented prevalence of 24% included grade I fractures, and other studies also considering mild deformities revealed a higher prevalence of osteoporotic spine fractures (25–33%) [15–17]. Including only moderate and severe deformities, a prevalence rate of only 12% (13/112) was found in this study. Compared to the study by Gehlbach et al., with a prevalence of 14%, a substantially younger study population was analyzed in this study [2]. As demonstrated in previous studies, the prevalence for vertebral fractures increases with age [18, 19]. In our study the group of women aged 75 and older showed a significantly higher prevalence in fractures.
As vertebral deformities often appear clinically silent, a large number of those fractures (approximately 50%) do not come to medical attention [20]. However, they are associated with increased back pain, functional limitation as well as disability, and therefore radiographic diagnosis is of substantial significance [20]. Additionally, prevalent vertebral insufficiency fractures are of major concern for treatment planning. Currently, an anti-resorptive therapy is recommended for patients with a 10-year fracture risk of more than 30% [21]. In a 60-year-old postmenopausal woman, this is the case for a BMD T-score of less than -4 without vertebral fractures, or if two or more insufficiency fractures are present, regardless the BMD. Unfortunately, several studies demonstrated that there is a poor reporting rate of vertebral fractures by radiologists [1, 2, 12, 22]. In our study none of the osteoporotic deformities were mentioned in the official radiology report. In previous studies, routine lateral chest radiographs were analyzed with a detection rate in the official radiology report between 15 and 60% [1, 2, 12, 22]. To our knowledge this is the first study to analyze fracture recognition of vertebral deformities on MDCT images. The radiology reports were based on axial MDCT images, where possible recognition is limited, compared to sagittal reformations. Less than 1/4 of the osteoporotic fractures could be detected on the axial sections (Fig. 1). In addition to difficulties in detecting fractures, only on axial sections could a further problem be the radiologist's clinical focus. Most of the patients were examined for malignancy evaluation. Therefore, osteoporotic deformities and additional spine lesions might not have been considered to be relevant and important for the patient. However, in cancer with long-term survival, such as lymphoma, patients may benefit from a timely diagnosis of an osteoporotic fracture in terms of life quality, mortalitiy and morbidity [23]. Also, it should be considered that long-term survivors of cancer are at higher risk for osteoporotic fracture; in particular, chemotherapy and radiation are detrimental to the bone, and insufficiency fractures are a frequent finding [23].
Our study demonstrated that sagittal reformations are of great value in detecting vertebral deformities of the spine. For instance, none of the SFI grade I fractures could be detected on the axial sections, though images were reviewed by two experienced radiologists. It seems that especially mild deformities can be better detected by sagittal MDCT reformations than with conventional radiographs [9]. However, the recognition and description of mild fractures seem of special interest as these patients benefit from timely diagnosis and treatment. A patient with a mild deformity has a 10% risk to develop a subsequent fracture in the following 3 years [24].
In this study we showed that osteoporotic vertebral fractures can be detected using sagittal reformations. This finding is in agreement with previous studies that demonstrated that sagittal reformations are comparable with conventional radiographs in the diagnosis of vertebral deformations when a 3-mm slice thickness is used [9, 25]. However, current MDCT technology allows thin multiplanar reformations using the original raw data even without first creating additional thin-section axial images, given this technology fracture visualization will be substantially enhanced compared to standard radiographs.
Additional spinal problems such as degenerative disc disease, scoliosis, osteoarthritis of the facet joints and hemangiomas and metastases were found in this study. Of those spinal problems, in particular degenerative disc disease was better visualized in sagittal reformations than in the original axial sections. Osteoarthritis of the facet joints as well as hemangiomas and metastases could be detected with similar diagnostic performance. However, sagittal reformations may give additional information in ambiguous cases in which axial sections are insufficient [26, 27].
Compared to other studies, we could not find a relationship between degenerative disc disease and risk for vertebral fractures [28, 29]. Those researchers found a higher prevalence of vertebral fracture only for disc space narrowing and not for the existence of osteophytes. However, another recent study found discordant results with a reduced risk for fracture for patients with spine osteoarthritis [30].
This study has several limitations. First of all, there was no consistent gold standard for the evaluation of the different spinal conditions. The frequency distributions were based on the sagittal reformations, except for the osteoarthritis of the facet joints. In addition, the study population showed a high prevalence of malignancy evaluation, and therefore the rate of spinal abnormalities may not be representative for postmenopausal women in general. However, it was shown that vertebral fractures are underdiagnosed using standard axial sections and inadequately reported by radiologists.
In summary this study demonstrated that sagittal MDCT reformations are well suited to detect spinal lesions. Especially osteoporotic spine fractures are substantially better recognized in sagittal reformations compared to axial MDCT data, which may have direct clinical implications for the individual patient. As recent CT systems allow reconstructing images without additional radiation exposure, we suggest obtaining sagittal reformations of the spine as a standard in all patients at risk for osteoporosis.
References
Kim N, Rowe BH, Raymond G, Jen H, Colman I, Jackson SA, Siminoski KG, Chahal AM, Folk D, Majumdar SR (2004) Underreporting of vertebral fractures on routine chest radiography. AJR Am J Roentgenol 182(2):297–300
Gehlbach S, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood J (2000) Recognition of vertebral fracture in a clinical setting. Osteoporos Int 11:577–582
Link TM, Guglielmi G, van Kuijk C, Adams JE (2005) Radiologic assessment of osteoporotic vertebral fractures: diagnostic and prognostic implications. Eur Radiol 15(8):1521–1532
Center JR, Nguyen TV, Schneider D, Sambrook NP, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Cockerill W, Lunt M, Silman AJ, Cooper C, Lips P, Bhalla AK, Cannata JB, Eastell R, Felsenberg D, Gennari C, Johnell O, Kanis JA, Kiss C, Masaryk P, Naves M, Poor G, Raspe H, Reid DM, Reeve J, Stepan J, Todd C, Woolf AD, O, Neill TW (2004) Health-related quality of life and radiographic vertebral fracture. Osteoporos Int 15(2):113–119
O’Neill TW, Cockerill W, Matthis C, Raspe HH, Lunt M, Cooper C, Banzer D, Cannata JB, Naves M, Felsch B, Felsenberg D, Janott J, Johnell O, Kanis JA, Kragl G, Lopes Vaz A, Lyritis G, Masaryk P, Poor G, Reid DM, Reisinger W, Scheidt-Nave C, Stepan JJ, Todd CJ, Woolf AD, Reeve J, Silman AJ (2004) Back pain, disability, and radiographic vertebral fracture in European women: a prospective study. Osteoporos Int 15(9):760–765
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3–S7
Ensrud K, Thompson D, Cauley J, Nevitt M, Kado D, Hochberg M, Santora A2, Black D (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc 48:241–249
Bauer JS, Muller D, Ambekar A, Dobritz M, Matsuura M, Eckstein F, Rummeny EJ, Link TM (2006) Detection of osteoporotic vertebral fractures using multidetector CT. Osteoporos Int 17(4):608–615
Ohnesorge B, Flohr T, Schaller S, Klingenbeck-Regn K, Becker C, Schopf UJ, Bruning R, Reiser MF (1999) [The technical bases and uses of multi-slice CT]. Radiologe 39(11):923–931
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Mui LW, Haramati LB, Alterman DD, Haramati N, Zelefsky MN, Hamerman D (2003) Evaluation of vertebral fractures on lateral chest radiographs of inner-city postmenopausal women. Calcif Tissue Int 73(6):550–554
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of osteoporotic fractures research group. Arch Intern Med 159(11):1215–1220
Melton LJ III, Lane AW, Cooper C, Eastell R, O, Fallon WM, Riggs BL (1993) Prevalence and incidence of vertebral deformities. Osteoporos Int 3(3):113–119
Delmas PD, van de LL, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20(4):557–563
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis the study of osteoporotic fractures research group. J Bone Miner Res 11(7):984–996
Mueller D, Isbary M, Boehm H, Bauer JS, Rummeny EJ, ink TM (2004) Recognition of osteoporosis-related vertebral fractures on chest radiographs in postmenopausal women. RSNA Chicago, 2004, p 305
Davies KM, Stegman MR, Heaney RP, Recker RR (1996) Prevalence and severity of vertebral fracture: the saunders county bone quality study. Osteoporos Int 6(2):160–165
Johansson C, Mellstrom D, Rosengren K, Rundgren A (1993) Prevalence of vertebral fractures in 85-year-olds. Radiographic examination of 462 subjects. Acta Orthop Scand 64(1):25–27
Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, Segal M, Genant HK, Cummings SR (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann intern Med 128(10):793–800
Pfeilschifter J (2006) 2006 DVO-guideline for prevention, diagnosis, and therapy of osteoporosis for women after menopause, for men after age 60 executive summary guidelines. Exp Clin Endocrinol Diabetes 114(10):611–622
Majumdar SR, Kim N, Colman I, Chahal AM, Raymond G, Jen H, Siminoski KG, Hanley DA, Rowe BH (2005) Incidental vertebral fractures discovered with chest radiography in the emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Arch Intern Med 165(8):905–909
Pfeilschifter J, Diel I (2000) Osteoporosis due to cancer treatment: pathogenesis and management. J Clin Oncol 18:1570–1593
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachi JD (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33(4):522–532
Begemann PG, Kemper J, Gatzka C, Stork A, Nolte-Ernsting C, Adam G (2004) Value of multiplanar reformations (MPR) in multidetector CT (MDCT) of acute vertebral fractures: do we still have to read the transverse images? J Comput Assist Tomogr 28(4):572–580
Mahnken AH, Wildberger JE, Gehbauer G, Schmitz-Rode T, Blaum M, Fabry U, Gunther RW (2002) Multidetector CT of the spine in multiple myeloma: comparison with MR imaging and radiography. AJR Am J Roentgenol 178(6):1429–1436
Sandrasegaran K, Rydberg J, Tann M, Hawes DR, Kopecky KK, Maglinte DD (2007) Benefits of routine use of coronal and sagittal reformations in multi-slice CT examination of the abdomen and pelvis. Clin Radiol 62(4):340–347
Sornay-Rendu E, Munoz F, Duboeuf F, Delmas PD (2004) Disc space narrowing is associated with an increased vertebral fracture risk in postmenopausal women: the OFELY Study. J Bone Miner Res 19(12):1994–1999
Sornay-Rendu E, Allard C, Munoz F, Duboeuf F, Delmas PD (2006) Disc space narrowing as a new risk factor for vertebral fracture: the OFELY study. Arthritis Rheum 54(4):1262–1269
Roux C, Fechtenbaum J, Briot K, Cropet C, Liu-Leage S, Marcelli C (2007) Inverse relationship between vertebral fractures and spine osteoarthritis in post menopausal women with osteoporosis. Ann Rheum Dis. (Epub ahead of print) DOI 10.1136/ard.2007.069369
Acknowledgements
The work was supported by the grant “Tandem-Projekt Osteoporose, Max-Planck-Society.”
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Müller, D., Bauer, J.S., Zeile, M. et al. Significance of sagittal reformations in routine thoracic and abdominal multislice CT studies for detecting osteoporotic fractures and other spine abnormalities. Eur Radiol 18, 1696–1702 (2008). https://doi.org/10.1007/s00330-008-0920-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-0920-2