Abstract
The purposes of this study were to determine the (1) frequency with which nonenhanced computed tomography (CT) (NECT) permits conclusive diagnosis of acute appendicitis, (2) accuracy of NECT when findings are conclusive, and (3) overall accuracy of a CT protocol consisting of NECT with selective use of contrast. Five hundred and thirty-six patients underwent a NECT protocol with selective use of contrast. Diagnostic accuracy was then determined separately for (1) patients with conclusive initial NECT, (2) patients with inconclusive initial NECT, and (3) all patients. NECT was conclusive on initial interpretation in 404/536 patients and inconclusive in 132/536. Of 132 inconclusive studies, 126 were repeated with contrast (intravenous, oral or rectal). Sensitivity, specificity, and positive and negative predictive value for diagnosis of acute appendicitis were (1) 90%, 96.0%, 84.8%, and 97.4% in patients with conclusive NECT (n = 404); (2) 95.6%, 92.3%, 73%, and 99% in patients with inconclusive NECT followed by repeat CT with contrast; and (3) 91.3%, 95%, 82%, and 98% in all patients. The initial diagnosis of appendicitis may be made by NECT in 75% of patients, with contrast administration reserved for inconclusive NECT studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The lifetime incidence of appendectomy is 12% in men and 25% in women in the United States, making it the most commonly performed emergency operation. Clinically, diagnosis of acute appendicitis is challenging in early stages of the disease and elderly or very young patients, because the presentation is often atypical [1]. While still high, the negative appendectomy rate has decreased in the last decade from 45–15.3%, in part due to advances in imaging [2–4]. Computed tomography (CT) has been recently introduced as the first diagnostic test for patients with acute nontraumatic abdominal symptoms, although controversies exit regarding the necessity of intravenous contrast [5–7].
Marked differences exist also between CT protocols to evaluate appendicitis. In particular, controversy exits regarding the need for intravenous contrast material and the use of oral and/or rectal contrast. Three general CT imaging strategies have been advocated: (1) nonenhanced CT (NECT), (2) contrast-enhanced CT (CECT), and (3) NECT with selective use of contrast. NECT is reported as an extremely accurate (90–97%) and sensitive (87–98%) technique, not only for diagnosis of acute appendicitis but for many other conditions that mimic appendicitis [7, 8]. The major advantages of the NECT approach are that (1) patients can be scanned immediately after presentation to the emergency department (ED) without waiting for orally administered contrast material to opacify bowel, (2) there is no discomfort associated with rectally administered contrast, (3) potential complications associated with intravenous contrast are avoided, and (4) the cost of the study is kept to a minimum.
An alternative approach, currently used at our institution, is NECT with selective use of contrast. In this approach, patients with suspected appendicitis are evaluated initially with NECT. If NECT images are conclusive (positive or negative for appendicitis), no further imaging is necessary. However, if findings are inconclusive, a repeat scan is performed with contrast. No previous study, to our knowledge, has determined the frequency with which initial NECT is conclusive versus inconclusive for appendicitis. Thus, the purposes of this study were to were to determine the (1) frequency with which NECT permits conclusive diagnosis, (2) accuracy of NECT when findings are conclusive, and (3) overall accuracy of a CT protocol consisting of NECT with selective use of contrast.
Materials and methods
Patients
This was a retrospective study conducted in an urban teaching hospital with institutional review board approval. From January 1998 to April 2002, 536 consecutive patients were referred for CT for suspected acute appendicitis with atypical clinical presentation and underwent an imaging protocol consisting of NECT with selective use of contrast. Patients were not preselected: they did not undergo any imaging studies before CT (plain films, ultrasound). Patients were aged 18–86 (mean 38) years and consisted of 220 men (range 18–77 years, mean 40 years) and 316 women (range 18–86 years, mean 37 years). The mean age of men and women was statistically significant (P < 0.03, two-tailed Student’s t test). Patients who underwent appendectomy within 2 weeks of CT or did not undergo appendectomy but had documented clinical follow-up of at least 4 weeks were included.
Imaging technique
From January 1998 to March 2000, CT scans were obtained with a helical single-detector scanner (9800 CTi; GE Medical Systems, Milwaukee, WI, USA) at 5-mm slice thickness with a pitch of 1.0, and images were reconstructed at 5-mm intervals. From March 2001 to April 2002, scans were performed with a four-detector row scanner (GE Light Speed, GE Medical Systems) using 5-mm slice thickness and 4 × 2.5 detector configuration at 15-cm/s table speed. Scans were obtained from the top of the T12 vertebral body to the pubic symphysis. Scans were viewed on the CT monitor by a radiologist while the patient was on the CT table in order to determine the need for contrast. If NECT was felt to be inconclusive, contrast was administered. The type of contrast was determined on a case-by-case basis by the monitoring radiologist based on personal expertise and noncontrast imaging findings (age and gender did not play a role in this decision); rational choice of contrast material was tailored to the patient’s anatomy. If determined necessary, intravenous and/or rectal contrast was administered immediately, and the patient was rescanned prior to leaving CT. If oral contrast was selected, the patient received oral contrast and was rescanned at least 40 min after drinking the contrast. Following preliminary review of images on the CT monitor, final image interpretation was performed with film (Kodak Image Link system, Eastman Kodak Company, Rochester, NY, USA) until April 2001 and with a picture archiving and communication system network (Agfa Healthcare IMPAX, Agfa Corporation, Ridgfield Park, NJ, USA) after April 2001. Diagnosis was made on only axial images; no multiplanar reformatted images were used.
Image interpretation
The radiology staff at our institution is heterogeneous, because even if we have dedicated radiologist (chest radiologist, gastrointestinal radiologist), everybody is involved in routine clinical work, but before CT was introduced in appendicitis diagnosis protocol at our hospital, conferences were taken by all radiology staff to introduce CT signs of appendicitis and CT morphological criteria of normal appendix. During the study, CT scans were reviewed by one radiologist, and no consult was admitted with a senior gastrointestinal radiologist. In this way, the protocol was focused to determine the purposes of our study in routine clinical work. Initial NECT scans were prospectively interpreted as negative if the appendix had intraluminal gas extending to its tip or if a nonopacified appendix was less than 6 mm in diameter. Because up to 42% of asymptomatic patients have an appendix diameter more than 6 mm [9], in symptomatic patients, CT was interpreted as positive if the appendix was greater than 6 mm in diameter and there were periappendiceal inflammatory changes, or if the appendix was not identified but secondary signs were present, with the center of inflammation in the expected region of the appendix [10, 11]. An isolated appendicolith was not considered sufficient for the diagnosis of acute appendicitis [12]. Thus, the initial NECT was considered conclusive if the nonenhanced images permitted diagnosis or exclusion of appendicitis, and NECT was considered inconclusive otherwise. If the appendix was not visualized and secondary signs were absent, the initial NECT was interpreted as inconclusive. Patients with inconclusive NECT were rescanned with contrast. Interpretation criteria of CT with contrast were the same as with NECT images except that the combination of a nonvisualized appendix and absent secondary signs were considered negative for the diagnosis of appendicitis.
Data analysis
Retrospectively, an abdominal radiologist reviewed all dictated CT reports without knowledge of patient outcome and recorded the following data: (1) whether each initial NECT was conclusive or inconclusive and (2) the final CT interpretation (positive or negative for appendicitis). Interobserver agreement between the retrospective and prospective readings was assessed using the kappa statistic.
Each patient’s medical chart, including surgical and pathological reports and discharge summaries, was then reviewed by the same radiologist. In patients who underwent surgery within 2 weeks of CT, pathological evaluation of the surgically removed appendix served as the reference standard for the diagnosis of appendicitis. In patients without appendectomy, clinical follow-up served as the reference standard. The final CT interpretation for each patient was then scored as true positive, true negative, false positive or false negative.
The percentage of cases in which the initial NECT was conclusive was calculated. This calculation was repeated after stratifying by patient gender and by the year (1998, 1999, 2000, 2001, 2002) in which the study was performed. Frequency differences between genders and years were compared using chi-squared tests. Sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) were calculated separately for (1) conclusive NECT examinations, (2) inconclusive NECT examinations that were followed by CECT examinations, and (3) all CT examinations (1 and 2 combined). Ninety-five percent confidence intervals (95% CI) were calculated for all performance parameters using the Wald method. Sensitivity, specificity, accuracy, PPV, and NPV were also calculated over all patients after stratifying by the year (from 1998 to 2002) in which the study was performed and by the CT scanner used (helical single-detector scanner from January 1998 to March 2000, four-detector row scanner from March 2001 to April 2002). Finally, a different abdominal radiologist (7 years’ experience) blinded to prospective reading and clinical outcome reviewed NECT images of all cases in which initial NECT was followed by CT with contrast. In this retrospective review, each NECT was considered either truly inconclusive or not in order to outline whether expertise in abdominal radiology could influence the necessity of additional CT scan with contrast or not. The inconclusive NECTs followed by CT with contrast were also reviewed to determine whether the additional contrast (intravenous or oral or rectal) was helpful or not.
Results
Patients with conclusive NECT
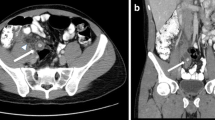
On prospective reading, NECT was conclusive in 404/536 (75%) patients, including 175/220 (80%) male and 229/316 (72%) female patients. The proportion of male (175) patients with conclusive NECT was higher than the proportion of female (229) patients (P < 0.04). Of the 404 conclusive NECT scans, 73/404 were true positive. CT was true negative in 310/404 patients with no evidence of appendicitis on pathology (n = 10) or clinical follow-up of at least 4 weeks (n = 300). In 13 patients with false positive CT, no appendectomy was performed and patients had a benign clinical follow-up (n = 12) or negative appendectomy (n = 1). In eight false negative cases, CT failed to detect subsequently proven appendicitis. Thus, sensitivity, specificity and accuracy of conclusive NECT were 90% (73/81; 95% CI: 0.81–0.95), 96.0% (310/323; 95% CI: 0.93–0.98), and 95% (383/404; 95% CI: 0.92–0.97). The PPV was 84.8% (73/86; 95% CI: 0.76–0.91); the NPV was 97.4% (310/318; 95% CI: 0.95–0.99) (Figs. 1, 2, 3)(Table 1).
Conclusive nonenhanced computed tomography (NECT): 40-year-old woman with pathologically proven acute appendicitis. The appendix (arrow) is enlarged (14 mm) with thickened wall (> 3 mm); two appendicoliths are recognizable. Lateroconal fascia is thickened, and there is mild periappendiceal stranding
Patients with inconclusive NECT
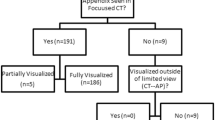
Initial NECT was inconclusive in 132/536 (25%) patients, including 45/220 (20%) male and 87/316 (28%) female patients (two-tailed P value = 0.0669). A repeat CT with contrast was recommended in all cases. In six patients, the CT with contrast was not performed, and they were excluded from statistical analysis because they did not follow the radiologist’s recommendation. Retrospective review of inconclusive NECT agreed with the prospective reading in 73.33% of observations (kappa = 0.322). The type of contrast administered was chosen at the discretion of the interpreting radiologist. Of the 126 patients who had repeat CT, 81 received intravenous contrast only, 32 received intravenous and oral contrast, five received intravenous and rectal contrast, seven received rectal contrast only, and one received oral contrast only. Summarizing, 118 patients received intravenous contrast, 33 oral contrast, and 12 rectal contrast (Fig. 4).
In the 126 patients who had NECT followed by repeat CT with contrast, the CECT was true positive in 22/126 patients (all with positive appendectomy), true negative in 95/126 (all with negative clinical follow-up without appendectomy), false positive in 8/126 (one patient with negative appendectomy and seven with benign follow-up), and false negative in 1/126 (positive appendectomy). Thus, in patients with inconclusive NECT, the follow up CECT led to a conclusive study in all patients and had a sensitivity of 95.7% (22/23; 95% CI: 0.77–1.0), specificity of 92.2% (95/103; 95% CI: 0.85–0.96), accuracy of 93% (117/126; 95% CI: 0.87–0.96), PPV of 73% (22/30; 95% CI: 0.55–0.86), and NPV of 99.0% (95/96; 95% CI: 0.94–1.0) (Fig. 5) (Table 1). As above, diagnostic accuracy was not calculated separately for male and female patients because of the small number of false positive and false negative cases. The frequency of nondiagnostic NECT examinations was constant for each year of the study.
The 126 nondiagnostic scans were reviewed by an abdominal radiologist and considered truly not diagnostic in 16% (85/530) of cases and diagnostic in 8% (41/530) of cases. Considering the small number of patients who received some type of contrast, it was not possible to perform a statistical analysis over all. Relative to each subset of patients in the retrospective reading, two abdominal radiologists in consensus reviewed the exams and considered for each type of contrast whether it was found to be helpful to reach a conclusive diagnosis or not. Intravenous contrast was felt to be helpful in increasing the confidence of diagnosis in 70% of cases (82/118), oral contrast was helpful in 65 % of case (13/20), and rectal contrast was given only in 12 cases and was felt to be helpful in 41% (5/12) of cases (Fig. 6).
All patients
A total of 530 patients were evaluated using NECT with selective use of contrast protocol (excluding the six patients in whom the protocol was not followed). Overall, based on prospective interpretation, there were 95 true positive cases with positive appendectomy, 405 true negative cases (negative appendectomy in 14 and negative clinical follow-up in 391), 21 false positive cases (negative appendectomy in two and negative clinical follow up in 19), and nine false negative cases (all with pathologically proven appendicitis). Thus, NECT with selective use of contrast had a sensitivity for acute appendicitis of 91.3% (95/104; 95% CI: 0.84–0.96), specificity of 95% (405/426; 95% CI: 0.93–0.97), and accuracy of 94.3% (500/530; 95% CI: 0.92–0.96). The PPV was 81.9% (95/116; 95% CI: 0.74–0.88) and the NPV was 97.8% (405/414; 95% CI: 0.96–0.99). The positive LR likelihood ratio (LR) was 19, and the negative LR was 0.09 (Table 1). Sensitivity, specificity, accuracy, PPV, and NPV, stratifying patients by year, were, respectively: for 1998 (43/530) 91.6%, 90%, 90.6%, 78.5%, and 96.5%; for 1999 (113/530) 84%, 92.5%, 91%, 69%, and 96.6%; for 2000 (118/530) 95.8%, 94.6%, 95%, 82%, and 98.8%; for 2001 (190/530) 81%, 98%, 96.8%, 81%, and 98%; for 2002 (66/530) 85.7%, 95%, 94%, 66.6%, and 98%. Sensitivity, specificity, accuracy, PPV, and NPV with helical single-detector scanner (186/530) were, respectively, 88.5%, 91%, 90.8%, 70.4%, and 97%, and with the four-detector row scanner, (344/530) 92.7%, 97%, 99.1%, 88.8%, and 98%. In 187/530 (35%) patients, there were 206 possible causes of abdominal pain: abnormal pelvic findings in female patients (75/530), gastrointestinal findings (59/530), urinary findings (61/530), and miscellaneous (11/530).
Retrospective false positive CT analysis
There were 21 false positive cases in prospective readings; three patients had negative appendectomy: two of them had cecal diverticulitis, and the other patient had on CT an appendix 9 mm in diameter with no secondary inflammatory signs, but the pathology was negative. Of the 18 patients with positive CT for acute appendicitis who did not undergo appendectomy, 13 were hospitalized with admitting diagnosis of acute appendicitis, and they were treated conservatively, with symptom resolution. The remaining 5/18 patients with positive CT and no appendectomy were discharged, with instructions to contact a doctor in case of increasing pain, especially on the right side. Thus, there were 13 patients who did not undergo surgery but who were treated conservatively for acute appendicitis. Those patients were considered false positive by our criteria, because there was no pathological reference. If considered true positive for acute appendicitis, the specificity and positive predictive value of CT would increase. Specificity and PPV would be 98.8% and 95%, respectively, overall; 99.7% and 98.6%, respectively, for patients who had an initial conclusive NECT; and 97.9% and 91.6%, respectively, for patients who underwent repeat CT with contrast.
Discussion
The use of CT for diagnosis of acute appendicitis has increased dramatically in recent years. CT is highly accurate, and it is well tolerated even by very sick patients. In asymptomatic patients, a normal appendix is visualized on CECT in 43–82% and in 77–82% on NECT [9, 13].
Specific primary and secondary signs have been described for CT diagnosis of acute appendicitis. Primary signs require visualization of the appendix, an important diagnostic goal that is strongly dependent by appendiceal size, amount of periappendiceal fat, and degree of ileocecal bowel opacification [11]. Primary signs are related to the morphological aspect of the appendix and include appendiceal enlargement, wall thickening, ill-defined margins, focal enhancement, and mural stratification. Secondary signs include appendicolith [12], and signs related to periappendiceal inflammation: cecal edema, inflammation of the mesoappendix or lateroconal fascia, and localized lymphadenopathy. Many of these signs can be detected without enteric or intravenous contrast because intraperitoneal fat is the intrinsic contrast medium [10, 14–16]. The most important sign of acute appendicitis on NECT is periappendiceal inflammation, which has been considered by many investigators a necessary criterion for diagnosing acute appendicitis, and it has been reported to be 98–100% sensitive [17, 18]. This can be seen as high-attenuation, linear, streaky densities or as poorly defined areas of increased density within the normal homogenous pericecal mesenteric fat. The optimal technique and role of CT remains controversial and varies among institutions. High accuracy has been reported with all CT techniques. At our institution, patients with suspected appendicitis are evaluated with NECT. If NECT is inconclusive, a repeat CT is performed with contrast.
Some investigators reported high accuracy with NECT alone, and some suggested that contrast is not necessary [8, 10, 11, 19–21]. However, in the 75% of cases with definitive NECT, the exam is very accurate (91.3%). We found that NECT alone was conclusive 75% of the time in routine clinical settings, but in 25% of cases, with no correlation to patient gender (P 0.0669), it was inconclusive and contrast administration was helpful. In our series, most patients with inconclusive NECT received intravenous contrast. Early in our experience, we found that intravenous contrast was most useful and could be given immediately with no delay in diagnosis. With intravenous contrast, the inflamed appendix enhances more than adjacent bowel loops, facilitating its identification. The disadvantages of intravenous contrast material are increased risk of contrast reaction or extravasation, and increased cost. The added risk and cost are justified in the minority of patients with truly nondiagnostic NECT, but we feel it is not necessary in the majority of patients undergoing CT for suspected appendicitis.
Oral contrast and rectal contrast were administered less frequently in our study, in part due to the associated delay. Oral contrast is associated with a 45- to 60-min delay, and rectal contrast is associated with a 15-min delay and with patient discomfort and anxiety. As reported in the literature [22], enteric contrast materials have been used to increase appendix visualization and to avoid false positive results caused by fluid-filled terminal ileal loops that could be misdiagnosed as distended, inflamed appendices.
Opacification of the appendix has been reported to exclude appendicitis; however, in some patients, the appendix may partially fill proximal to the site of appendiceal obstruction and lead to false negative exams [23]. Furthermore, the lack of opacification does not diagnose disease; up to 76% of normal appendices do not fill with oral contrast, and up to 15–20% of normal appendices do not fill with rectal contrast material [9, 24]. Also, once the bowel is opacified with enteric contrast, it may be more difficult to identify an enhancing inflamed appendix than if no enteric contrast was administered.
There were several limitations to our study: It was subject to the biases associated with a retrospective design. Another limitation was the lack of appropriate reference standard in some cases. For negative CT, clinical follow-up is a reasonable reference standard; however, in our series, 18 patients with positive CT (on prospective and retrospective reading) had no appendectomy at our institution as of the time of review. These patients were considered false positive based on our criteria; however, many were admitted and treated with antibiotics (some with an admitting diagnosis of appendicitis). Thus, some of these patients might have had appendicitis that was successfully treated medically. While not standard practice, conservative management of appendicitis has been reported in the literature for cases in which surgery in the acute phase may be complicated [25, 26]. Another bias is the different result in conclusive NECT between male and female, which may be due to difference in body mass index, but this data was not evaluated during our study.
Compared with other CT imaging protocols, NECT with selective use of contrast has several advantages for patients with suspected appendicitis in a busy emergency department setting. This is especially important, as the use of CT has dramatically increased recently and has become routine in the initial assessment of the emergency department patient with acute nontraumatic abdominal pain [6, 27–30]. NECT can serve as a general abdominal screen without the added cost and risk of contrast. Disadvantages of the protocol primarily involve the minority of patients who require repeat scanning, but in order to minimize the negative impact, it is most important to limit repeat scanning by appropriate patient selection: because only 25% of patients have a repeat CT, there is a globally limited radiation exposure. However, even with appropriate patient selection, it is likely some patients will require contrast for conclusive diagnosis, and the radiation and cost involved in scanning these patients twice must be seriously considered [31, 32].
Conclusion
We have found that when conclusive, NECT is diagnostic with high accuracy in the majority of patients with suspected appendicitis in routine clinical settings. Additional scanning with contrast enhancement should be used is selected cases when NECT is inconclusive.
References
Flum DR, Koepsell T (2002) The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 137(7):799–804
Hale DA et al (1997) Appendectomy: a contemporary appraisal. Ann Surg 225(3):252–261
Flum DR et al (2001) Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA 286(14):1748–1753
Schmidt T et al (2005) Phase-inversion tissue harmonic imaging compared to fundamental B-mode ultrasound in the evaluation of the pathology of large and small bowel. Eur Radiol 15(9):2021–2030
Lee SY et al (2006) Prospective comparison of helical CT of the abdomen and pelvis without and with oral contrast in assessing acute abdominal pain in adult Emergency Department patients. Emerg Radiol 12(4):150–157
Tsushima Y et al (2002) Effect of contrast-enhanced computed tomography on diagnosis and management of acute abdomen in adults. Clin Radiol 57(6):507–513
Basak S et al (2002) Is unenhanced CT sufficient for evaluation of acute abdominal pain? Clin Imaging 26(6):405–417
Christopher FL et al (2002) Unenhanced helical CT scanning of the abdomen and pelvis changes disposition of patients presenting to the emergency department with possible acute appendicitis. J Emerg Med 23(1):1–7
Tamburrini S et al (2005) CT appearance of the normal appendix in adults. Eur Radiol 15(10):2096–2103
Funaki B (2000) Nonenhanced CT for suspected appendicitis. Radiology 216(3):916–918
Ege G et al (2002) Diagnostic value of unenhanced helical CT in adult patients with suspected acute appendicitis. Br J Radiol 75(897):721–725
Lowe LH et al (2000) Appendicolith revealed on CT in children with suspected appendicitis: how specific is it in the diagnosis of appendicitis? AJR Am J Roentgenol 175(4):981–984
Benjaminov O et al (2002) Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology 225(2):400–406
Balthazar EJ, Gordon RB (1989) CT of appendicitis. Semin Ultrasound CT MR 10(4):326–340
Lane MJ et al (1997) Unenhanced helical CT for suspected acute appendicitis. AJR Am J Roentgenol 168(2):405409
Rao PM, Rhea JT, Novelline RA (1997) Sensitivity and specificity of the individual CT signs of appendicitis: experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr 21(5):686692
Pereira JM et al (2004) Disproportionate fat stranding: a helpful CT sign in patients with acute abdominal pain. Radiographics 24(3):703715
Balthazar EJ et al (1988) Computed tomography of the abnormal appendix. J Comput Assist Tomogr 12(4):595601
Malone AJ (1999) Unenhanced CT in the evaluation of the acute abdomen: the community hospital experience. Semin Ultrasound CT MR 20(2):68–76
Mindelzun RE, Jeffrey RB (1997) Unenhanced helical CT for evaluating acute abdominal pain: a little more cost, a lot more information. Radiology 205(1):43–45
Rao PM (2000) Nonenhanced CT for suspected appendicitis. Radiology 216(3):916
Rao PM et al (1997) Helical CT combined with contrast material administered only through the colon for imaging of suspected appendicitis. AJR Am J Roentgenol 169(5):1275–1280
Rao PM, Rhea JT, Novelline RA (1997) Distal appendicitis: CT appearance and diagnosis. Radiology 204(3):709–712
Funaki B, Grosskreutz SR, Funaki CN (1998) Using unenhanced helical CT with enteric contrast material for suspected appendicitis in patients treated at a community hospital. AJR Am J Roentgenol 171(4):997–1001
Cobben LP, de Van Otterloo AM, Puylaert JB (2000) Spontaneously resolving appendicitis: frequency and natural history in 60 patients. Radiology 215(2):349–352
Oliak D et al (2000) Nonoperative management of perforated appendicitis without periappendiceal mass. Am J Surg 179(3):177–181
Urban BA, Fishman EK (2000) Targeted helical CT of the acute abdomen: appendicitis, diverticulitis, and small bowel obstruction. Semin Ultrasound CT MR 21(1):20–39
Smith RC et al (1996) Diagnosis of acute flank pain: value of unenhanced helical CT. AJR Am J Roentgenol 166(1):97–101
Rosen MP et al (2003) Value of abdominal CT in the emergency department for patients with abdominal pain. Eur Radiol 13(2):418–424
Brown DF et al (2002) The role of abdominal computed tomography scanning in patients with nontraumatic abdominal symptoms. Eur J Emerg Med 9(4):330–333
Golding SJ, Shrimpton PC (2002) Commentary. Radiation dose in CT: are we meeting the challenge? Br J Radiol 75(889):1–4
Dixon AK, Goldstone KE (2002) Abdominal CT and the Euratom Directive. Eur Radiol 12(6):1567–1570
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamburrini, S., Brunetti, A., Brown, M. et al. Acute appendicitis: diagnostic value of nonenhanced CT with selective use of contrast in routine clinical settings. Eur Radiol 17, 2055–2061 (2007). https://doi.org/10.1007/s00330-006-0527-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0527-4