Abstract
This study assessed the diagnostic effectiveness of multidetector spiral CT arthrography (MDCTa) in detecting hyaline cartilage abnormalities of the shoulder joint, with correlation to arthroscopy. Shoulder MDCTa images prospectively obtained in 22 consecutive patients (mean age, 50 years; age range, 23–74 years; 12 female, 10 male) were evaluated for glenohumeral cartilage lesions. Two musculoskeletal radiologists independently analysed the cartilage surfaces of the humeral head and of the glenoid fossa in nine anatomical surface areas. Observations of MDCTa were compared to arthroscopic findings. The sensitivity and specificity of MDCTa for grade 2 (substance loss <50%) or higher and grade 3 (substance loss ≥50%) or higher cartilage lesions, the Spearman correlation coefficient between arthrographic and arthroscopic grading, and K statistics for assessing Intra and Interobserver reproducibility were determined. At MDCTa, sensitivities and specificities ranged between 80% and 94% for the detection of grade 2 or higher cartilage lesions, and between 88% and 98% for the detection of grade 3 or higher cartilage lesions. Spearman correlation coefficients between MDCTa and arthroscopic grading of articular surfaces ranged between 0.532 and 0.651. Interobserver agreement was moderate for grading all articular surfaces (κ = 0.457), but substantial to almost perfect for detecting lesions with substance loss (κ, 0.618–0.876). In conclusion, MDCTa is accurate for the study of cartilage surface in the entire shoulder joint. This technique may beneficially impact patient’s management by means of selecting the proper treatment approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance (MR) imaging and MR arthrography (MRa) are the imaging modalities of choice for the assessment of the glenohumeral joint. The diagnostic effectiveness of these techniques in evaluating many of the articular structures of the glenohumeral joint, such as the rotator cuff, the glenoid labrum and the biceps tendon, has been widely studied [1–4]. More recently, Guntern, et al. have shown moderate accuracy of MRa in detecting glenohumeral cartilage lesions [5].
The articular cartilage of the knee, which is relatively thick (approximately 4 mm), has been studied extensively by using MR and spiral CT arthrography [6–11]. In a few studies, investigators have evaluated thinner articular cartilages, such as those present in the hip, ankle, elbow and other small joints [12–14].
Developments in spiral CT technology, with multidetector arrays that enable submillimeter spatial resolution in large joints, raised the question of the potential use of multidetector spiral CT arthrography (MDCTa) for the assessment of the hyaline cartilage of the glenohumeral joint. This question is of potential clinical value, since the integrity of the cartilage surface of the shoulder has an influence on the differential diagnosis of shoulder pain and, many times, on the treatment options [15]. An accurate imaging method is needed to recognize patients who might benefit from the most recent therapeutic approaches of cartilage lesions.
To our knowledge, the performance of MDCTa in this indication has not yet been evaluated.
The purpose of this study was to assess the value of MDCTa in the evaluation of the entire shoulder cartilage.
Materials and methods
Patients
Twenty-two patients were prospectively enrolled between December 2004 and December 2005.
The inclusion criteria were:
-
(a)
chronic shoulder pain or disorder with proposed arthroscopic treatment,
-
(b)
MDCTa of the shoulder performed at our institution according to a standardized protocol, as part of pre-operative work-up,
-
(c)
arthroscopy performed at our institution by the same orthopaedic surgeon with a prospective precise analysis and description of the gleno-humeral cartilage according to a defined protocol (cf. infra), and
-
(d)
preserved gleno-humeral joint and subacromial space on conventional radiographs, with no osteophytosis, to avoid selection of patients with severe and extensive cartilage lesions due to degenerative shoulder disease.
The time delay between MDCTa and the arthroscopy had to be less than 1 month.
Patients with a previous history of arthroscopic or open shoulder surgery were excluded from this study.
Twelve patients were female and ten were male. Age ranged between 23 and 74 years (mean, 50 years). Eleven left and 11 right shoulders were examined.
Patients were informed about the possibility that their arthrographic and arthroscopic charts could be reviewed for scientific purposes, and gave their informed consent.
The final diagnoses based on MDCTa and arthroscopic observations were: (1) subacromial impingement syndrome (supraspinatus tendinopathy or partial rotator cuff tear, narrowing of the subacromial space due to a subacromial spur, osteoarthritis of the acromio-clavicular joint, subacromial bursitis, degenerative changes of the long tendon of biceps) [n = 14], (2) full thickness rotator cuff tear [n = 4], (3) a superior, superior anteroposterior labral (SLAP) tear [n = 9], (4) tendon calcifications [n = 5], (5) secondary osteochondromatosis [n = 2], and (6) history of previous shoulder dislocation with residual instability treated by arthroscopy [n = 4] (more than one diagnosis possible).
Multidetector spiral CT arthrography (MDCTa)
All spiral CT arthrograms were performed by the same musculoskeletal radiologist.
Immediately before the MDCTa examination, and after local anaesthesia, a 10-ml volume of ionic contrast material (320 mg of iodine per millilitre; meglumine ioxalate and sodium ioxalate; Hexabrix 320, Guerbet, Aulnay-sous-bois, France) diluted with 5 ml of local anesthetic (Scandicaine) was injected under fluoroscopic guidance.
Spiral CT was performed on a sixteen-detector helical CT unit (MX8000IDT, Philips Medical Systems, Best, The Netherlands), with the spiral-scanning mode. All patients were placed in supine, head first, the arm along the body, with the shoulder in neutral position and the thumb pointing upward. After a face projection scout image, a 10- to 15-second scanning was performed to image the area between the upper pole of the acromio-clavicular joint and the lower margin of the opacified axillar recess of the shoulder joint.
Spiral scanning was performed at 120 kVp and 350 mAs, with a focal spot size of 0.8 × 1.2 mm. The collimation beam was 12 mm. A dynamic oscillating spot was used. The field of view at acquisition was 25 cm. The table speed was 4.8 mm/sec (effective pitch of 0.3,) and the effective section thickness was 0.8 mm. For reconstruction, a 3D Cone Beam back projection algorithm, a high frequency kernel, an increment of 0.4 mm (50% section overlap), and a zoom factor of 1.2 were used. Images were reconstructed on a 512 × 512 matrix, and in-plane resolution was 12 lp/cm resolution (isotropic resolution, filter C). Longitudinal resolution was 0.4 mm, because with a pitch value of 0.3 and a reconstruction increment of 50% of the nominal section width, longitudinal resolution equalled the reconstruction increment of 0.4 mm.
Arthroscopy
The same orthopaedic surgeon, who was unaware of the precise imaging appearance of the cartilage on the spiral CT, performed shoulder arthroscopies in all patients using the following procedure. The patients were placed in lateral position. The procedures were performed with the patient under a combined scalene block and general anesthesia. A 30°, 4-mm arthroscope was introduced in the gleno-humeral joint through a posterior approach (viewing portal). Arthroscopic examination of the cartilage was performed with a hook introduced via an anterior portal.
The system used to grade articular cartilage at macroscopic inspection was a modification of the Outerbridge and Noyes classification systems, usually used at arthroscopy (Table 1) [16, 17]. This system is based on the following four parameters, which were carefully recorded: integrity of the articular surface, depth of substance loss, location of the lesion, and diameter of the lesion.
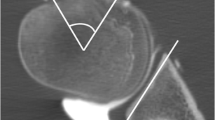
Grading of articular surfaces and delineation of the lesions were performed in nine anatomic areas for each humeral head and glenoid cartilage surface, and reported on diagrams in which each articular surface was divided into three virtual thirds in both cranio-caudal and antero-posterior directions (Fig. 1). Grading system of cartilage lesions is summarized in Table 1 and Fig. 2.
Schematic view of the delimitation of nine anatomic regions in each humeral head (right) and glenoid (left) cartilage surface. These surfaces are divided into three virtual thirds in both cranio-caudal and antero-posterior directions. These diagrams were used for cartilage grading at arthroscopy and during MDCTa images review
Schematic drawing of the system used for cartilage lesion grading at MDCTa and at arthroscopy. Grade 0: sharp surface, without substance loss. Grade 1: loss of the sharp and smooth contour of cartilage surface with appearance of subtle undulations and unsharpness of the surface; no contrast material within the cartilage at MDCTa. Grade 2: cartilage defect at arthroscopy and contrast penetration at MDCTa, that involve less than half of the thickness of the normal adjacent cartilage surface. Grade 3: cartilage defect at arthroscopy and contrast penetration at MDCTa, that involve at least the superficial half of the cartilage thickness but do not reach the subchondral bone. Grade 4: complete loss of normal cartilage, with contrast material reaching the subchondral bone at MDCTa
Diagnosis and treatment of the above detailed rotator cuff, capsulo-labral or other joint disorders were performed during the same arthroscopic procedure.
Image analysis
All CT arthrograms were prospectively stored on optical disks. In April 2006, one experienced musculoskeletal radiologist and one 5th-year resident in radiology separately analyzed the spiral CT arthrograms on a workstation (Omnipro; Silicon Graphics, Mountain View, CA, USA) using coronal and transverse multiplanar reconstructed (MPR) images. The sets of CT examinations were reviewed in a random order, blinded to the identity of the patients and without knowledge of arthroscopic findings. Coronal and transverse MPR images with a 0.8 mm section thickness were reviewed simultaneously, using bone settings (window width, 1,900 HU; window level, 450 HU), and a zoom factor of 2.8. For the nine anatomic regions of each humeral head and glenoid fossa, which were identical to those defined for the arthroscopic analysis (Fig. 1), the grade of the articular surface was determined. When more than one lesion was present in a defined region, the deepest lesion observed in that region was taken into account for grading.
Articular surfaces were graded according to the following system (Fig. 2).
Grade 0 surface was defined by a sharp line of contrast material on the cartilage surface, without substance loss (Fig. 2; Table 1). Grade 1 surface was defined by a loss of the sharp and smooth contour of the cartilage surface, with the appearance of subtle undulations and unsharpness of the cartilage surface; there was no contrast material within the cartilage. Grade 2 surface was defined by the penetration of contrast material within the cartilage, that involved less than half of the thickness of the normal adjacent cartilage. Grade 3 surface was defined by the penetration of contrast material within the cartilage, that involved at least the superficial half of the cartilage thickness but did not reach the subchondral bone. Grade 4 surface was defined by the complete loss of normal cartilage, with contrast material reaching the subchondral bone. When surface grading differed between the imaging planes, the most severe grade was elected.
After a 2-month delay, the first observer repeated the blinded interpretation of all examinations to determine intraobserver reproducibility.
Statistical analysis
Statistical analysis was performed by a statistician. Sensitivity and specificity for detecting grade 2 or higher cartilage lesions were calculated by considering as test-positive areas all areas in which at least grade 2 lesions were present at MDCTa. Sensitivity and specificity for detecting grade 3 or higher lesions (lesions with at least 50% substance loss) were calculated by considering as test-positive areas all areas in which at least grade 3 lesions were present at MDCTa. Correlations between grades determined at MDCTa and those determined by arthroscopic inspection were assessed by using the Spearman rank coefficient. Interobserver and intraobserver agreements were assessed by using κ statistics. As suggested by Landis and Koch, κ values less than 0 were considered to be poor agreement; between 0 and 0.2, slight agreement; between 0.21 and 0.40, fair agreement; between 0.41 and 0.60, moderate agreement; between 0.61 and 0.80, substantial agreement; and between 0.81 and 1.0, almost perfect agreement [18].
Results
Arthroscopic findings
At arthroscopic examination, 260 of 396 articular surface areas (22 shoulders × [nine humeral + nine glenoidal surfaces] in each shoulder) were intact (grade 0; Fig. 3); 101 surface areas were categorized as grade 1 (Fig. 4); nine surfaces, grade 2 (Fig. 5); 17 surfaces, grade 3 (Fig. 6); and nine surface areas, grade 4 (Fig. 7) (Table 2).
Coronal (a) and transverse (b) reformations of the gleno-humeral joint reconstructed after MDCTa show discrete loss of cartilage surface sharpness within the central portion of the humeral head (arrows), considered to be grade 1 (this grading is highly subjective and could probably have been considered as almost normal—grade 0). c Close-up photograph of the corresponding area at arthroscopy shows cartilage softening (surface depression at palpation)
Coronal (a) and transverse (b) reformations of the glenohumeral joint reconstructed after MDCTa show contrast material penetration (arrows) in the central portion of the glenoid cartilage surface. This lesion was considered to be grade 2 because substance loss was inferior to 50% of normal cartilage. Note the presence of an ossified nodule in relation to secondary synovial osteochondromatosis in the axillary recess of the joint (asterisk in a). c Close-up photograph of the corresponding area at arthroscopy shows a defect (arrows) in the glenoid cartilage surface that involves less than 50% of the cartilage thickness
Coronal (a) and transverse (b) reformations of the glenohumeral joint reconstructed after MDCTa show contrast material penetration (arrows) in the central portion of the glenoid cartilage surface. This lesion was considered to be grade 3 because the defect involved more than 50% of cartilage thickness but did not reach the subchondral bone. c Close-up photograph of the corresponding area at arthroscopy reveals evident defect of the articular cartilage surface of the glenoid fossa (arrows)
Coronal (a) and transverse (b) reformations reconstructed after MDCTa show deep focal penetration of contrast material in the glenoidal cartilage (arrows). This lesion was considered to be grade 4 because the lesion reached the subchondral bone. c On the corresponding arthroscopic image and at palpation of the glenoid surface, the defect (arrows) reaches the subchondral bone (grade 4)
Detection of grade 2 or higher and grade 3 or higher cartilage lesions
Sensitivity and specificity values are listed in Table 3. Sensitivities of MDCTa for the detection of grade 2 or higher cartilage lesions were 94% and 80% for observers 1 and 2 respectively; specificities were 94% and 92% for observers 1 and 2 respectively. Sensitivities for the detection of grade 3 or higher cartilage lesions were 96% and 88% for observers 1 and 2 respectively; specificity was 98% for both observers.
Grading of articular surfaces
At MDCTa, 250 (63%) of the 396 regions were graded identically to macroscopic examination by observer 1. The 146 regions that were graded differently at MDCTa and arthroscopic examination differed by one grade in 128 regions and by two grades in 18.
A total of 95% of the regions were graded within one grade, and 100% were within two grades (Table 4). Results obtained by observer 1 and observer 2 are listed in Table 4.
There was moderate to substantial agreement between grading at arthroscopic examination and grading at MDCTa (Spearman correlation coefficients ranging from 0.532 to 0.651) (Table 5).
Interobserver and intraobserver reproducibility (Table 6)
At MDCTa, interobserver agreement was moderate for grading articular surfaces (κ of 0.457). Agreement was substantial for detecting grade 2 or higher and almost perfect for detecting grade 3 or higher cartilage lesions (respective κ values of 0.618 and 0.876) (Table 6). Intraobserver agreement was substantial for grading articular surfaces (κ of 0.634) and almost perfect for detecting grade 2 or higher and grade 3 or higher cartilage lesions (respective κ values of 0.845 and 0.851).
Discussion
The vast majority of imaging studies dedicated to the shoulder have focused on the use of MR imaging, CT arthrography or MR arthrography (MRa) to analyze lesions of the rotator cuff and of the glenoid labrum [1–4, 19–22]. In contrast to this fibrocartilage, the hyaline cartilage of the shoulder has barely been studied by modern imaging techniques. Guntern recently studied this cartilage using MRa [5].
The current study assessed the value of multidetector spiral CT arthrography (MDCTa) of the shoulder, and found that this technique enables accurate assessment of the articular cartilage of the glenoid fossa and of the humeral head. Sensitivities and specificities of MDCTa ranged between 80% and 94% for the detection of grade 2 and higher cartilage lesions, and between 88% and 98% for the detection of grade 3 and higher cartilage lesions (lesions with substance loss).
The diagnostic effectiveness of MDCTa in detecting glenohumeral cartilage lesions in our study is similar to that of the single- or dual-detector spiral CT arthrography in the knee. Vande Berg et al. studied CT arthrography in the knee, and reported respective sensitivities and specificities of 80% and 88% for the detection of lesions with less than 50% substance loss, and 85% and 94% for lesions with more than 50% substance loss [6]. MDCTa thus seems able to reach this effectiveness in larger anatomic areas than the knee, and in thinner cartilage surfaces (the humeral head and glenoidal cartilage have respective mean thicknesses of 1.24 mm and 1.88 mm, whereas the cartilage of the knee measures up to 4 mm thick) [11, 21].
We found moderate to substantial agreement between grading of articular surfaces at MDCTa and grading at arthroscopy, with Spearman correlation coefficients ranging from 0.532 to 0.651. Reproducibility of the technique for the detection of lesions with substance loss (grade 2 or higher) was substantial to almost perfect, whereas reproducibility for grading of all lesions was limited. These imperfect results reflect well-known difficulties of CT arthrography in differentiating normal cartilage surfaces (grade 0) from qualitative cartilage changes without substance loss (grade 1) (see also lack of evident difference in cartilage appearance on Figs. 3 and 4) [6].
We found no report in the literature to compare our results with previous studies of the shoulder cartilage using CT arthrography. Our results with MDCTa appear promising when compared to published results of assessment of glenohumeral cartilage lesions with MRa [5]. Other investigators found lower sensitivity, specificity and reproducibility values using MRa for the study of the shoulder cartilage [5, 23]. However, this comparison of our results using MDCTa with published evaluation of MR imaging and MRa must remain cautious. Indeed, differences may be related to the number of response categories between the current study and previous studies.
Several reasons may be proposed to explain the valuable assessment of the shoulder cartilage by MDCTa.
First, MDCTa offers excellent spatial resolution. The slice thickness in our study was 0.8 mm. This is much lower than slice thickness usually obtained in routine practice and in published studies using MR imaging and MRa [5, 23]. This value of MDCTa could further be compared to studies using more advanced MR protocols (3D, thin sections).
Second, multiplanar capacity of MDCTa allows excellent analysis of the cartilage. Coronal oblique and transverse images reconstructed after MCDTa enable excellent depiction of the glenohumeral cartilage because these images are perpendicular to the articular surfaces. The in-plane and longitudinal resolution of 0.4 mm also contributes to these results.
Third, MDCTa provides images with high contrast resolution. Administration of an intraarticular positive iodinated contrast agent enables delineation of the cartilage surface with excellent lesion conspicuity, because open (grade 2 or higher) cartilage lesions filled with contrast material show high-attenuation density, whereas intact cartilage shows low-attenuation density [24]. In comparison, MR imaging and MRa may face difficulties in detecting cartilage surface lesions, because the signal of cartilage defects is highly variable on these images, and because of the limited contrast between cartilage and surrounding structures [6, 25, 26].
A limitation of the current study is that we did not assess the distribution of cartilage lesions on the glenoid and humeral head surface. This decision results from the wide variety of inclusion criteria and articular disorders in our series of patients, and from the limited number of observations of lesions of each grade.
Compared to other studies, we did not obtain cadaveric or histologic correlations [6, 23, 25]. This could be obtained in a future study, although cadaveric studies generally limit information to elderly patients, whereas clinical series enable the study of cartilage lesions in a wide age range of adult patients. However, because of the limited size of the current series, we did not address the correlation between patient profile (age, gender, profession and sports activities, ...) and the severity of cartilage lesions.
MDCTa definitely has several intrinsic disadvantages in comparison with MR imaging. First, MDCTa is invasive, because it requires intraarticular material injection and ionizing radiation. Second, it is limited to the depiction of the cartilage surface, and closed cartilage lesions remain occult [27]. Indeed, it is inherently limited for the study of the intrinsic changes within the cartilage, due to the lack of attenuation variability within the zones of the hyaline cartilage [6].
Further works could concentrate on the comparison between MDCTa and MR imaging, or between MDCTa and MRa, which are both invasive, in the same series of patients. This was not done in this study, which only focused on routine preoperative examinations performed at our institution, with no addition of paramagnetic contrast material and imaging procedures.
In terms of clinical significance, cartilage lesions within the shoulder joint may be regarded as an ancillary finding, at the background of rotator cuff or labrum disorders [28]. However, the high frequency of these lesions, and the potential clinical and therapeutic impact of their proper assessment, must be underlined.
In the setting of the differential diagnosis of shoulder pain, arthritic changes may be clinically relevant, because they can accompany or mimic symptoms of shoulder impingement syndrome, and the treatment options for these two conditions are different [15].
Traditionally, after exclusion of other joint abnormalities, treatment of shoulder osteoarthritis consists of conservative treatment with oral anti-inflammatory medications and physical therapy. If conservative therapy fails to relieve symptoms, arthroscopic treatment may be considered [29]. For localized articular cartilage damage, joint lavage, loose body removal, degenerative cartilage debridement and repair of rotator-cuff tears may offer significant improvement, with relatively low morbidity [30]. Diffuse articular lesions may be treated by more invasive procedures, such as microfractures and perforations, which are supposed to provoke a bleeding response and subsequent growth of fibrocartilage to reinforce the articular surface [25]. More recent therapeutic options such as osteochondral transplantation may be performed for well-delimited deep cartilage defects [31]. We believe that MDCTa may play a role in the recognition of patients who are candidates to this therapeutic approach and in treatment planning.
In conclusion, this work assessed the value of MDCTa for studying the articular of the entire shoulder. This technique had a sensitivity and specificity range between 80% and 94% for detection of all open cartilage lesions and between 89% and 98% for detection of lesions with at least 50% substance loss.
References
Hodler J, Kursunoglu-Brahme S, Snyder SJ et al (1992) Rotator cuff disease: assessment with MR arthrography versus standard MR imaging in 36 patients with arthroscopic confirmation. Radiology 182:431–436
Zanetti M, Weishaupt D, Gerber C, Hodler J (1998) Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography. AJR Am J Roentgenol 170:1557–1561
Bencardino JT, Beltran J, Rosenberg ZS et al (2000) Superior labrum anterior-posterior lesions: diagnosis with MR arthrography of the shoulder. Radiology 214:267–271
Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP (2001) Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology 218:127–132
Guntern DV, Pfirrman CW, Schmid MR et al (2003) Articular cartilage lesions of the glenohumeral joint: diagnostic effectiveness of MR arthrography and prevalence in patients with subacromial impingement syndrome. Radiology 226:165–170
Vande Berg BC, Lecouvet FE, Poilvache P et al (2002) Assessment of knee cartilage in cadavers with dual-detector spiral CT arthrography and MR. Radiology 222:430–436
Vande Berg BC, Lecouvet FE, Malghem J (2002) Frequency and topography of lesions of the femoro-tibial cartilage at spiral CT arthrography of the knee. Skeletal Radiol 31:643–649
McCauley TR, Kier R, Lynch KJ, Jokl P (1992) Chondromalacia patellae: diagnosis with MR imaging. AJR Am J Roentgenol 158:101–105
Recht MP, Kramer J, Marcelis S et al (1993) Abnormalities of cartilage in the knee: analysis of available MR techniques. Radiology 187:473–478
Bredella MA, Tirman PF, Peterfy CG et al (1999) Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol 172:1073–1080
Hall FM, Wyshack G (1980) Thickness of articular cartilage in the normal knee. J Bone Joint Surg Am 62:408–413
Hodler J, Trudell D, Pathria MN, Resnick D (1992) Width of the articular cartilage of the hip: quantification by using fat-suppression spin-echo MR imaging in cadavers. AJR Am J Roentgenol 159:351–355
Tan TC, Wilcox DM, Frank L et al (1996) MR imaging of cartilage in the ankle: comparison of available imaging sequences and methods of measurement in cadavers. Skeletal Radiol 25:749–755
Waldt S, Bruegel M, Ganter K, Kuhn V, Link TM, Rummeny EJ, Woertler K (2005) Comparison of multislice CT arthrography and MR arthrography for the detection of articular cartilage lesions of the elbow. Eur Radiol 15:784–791
Ellman H, Harris E, Kay SP (1992) Early degenerative joint disease simulating impingement syndrome: arthroscopic findings. Arthroscopy 8:482–487
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg 43:752–757
Noyes FR, Stabler CL (1989) A system for grading articualr cartilage lesions at arthroscopy. Am J Sports Med 17:505–513
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Roger B, Skaf A, Hooper AW, Lektrakul N, Yeh L, Resnick D (1999) Imaging findings in the dominant shoulder of throwing athletes: comparison of radiography, arthrography, CT arthrography, and MR arthrography with arthroscopic correlation. AJR Am J Roentgenol 172:1371–1380
De Maeseneer M, Van Roy F, Lenchik L et al (2000) CT and MR arthrography of the normal and pathologic anterosuperior labrum and labral-bicipital complex. Radiographics 20:S67–S81
Waldt S, Metz S, Burkart A et al (2006) Variants of the superior labrum and labro-bicipital complex: a comparative study of shoulder specimens using MR arthrography, multi-slice CT arthrography and anatomical dissection. Eur Radiol 16:451–458
Blum A, Coudane H, Mole D (2000) Gleno-humeral instabilities. Eur Radiol 10:63–82
Yeh LR, Kwak S, Kim YS et al (1998) Evaluation of articular cartilage thickness of the humeral head and the glenoid fossa by MR arthrography: anatomic correlation in cadavers. Skeletal Radiol 27:500–504
Gagliardi JA, Chung EM, Chandnani VP et al (1994) Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol 163:629–636
Hodler J, Loredo RA, Longo C, Trudell D, Yu JS, Resnick D (1995) Assessment of articular cartilage thickness of the humeral head: MR-anatomic correlation in cadavers. AJR Am J Roentgenol 165:615–620
Vande Berg BC, Lecouvet FE, Maldague B, Malghem J (2004) MR appearance of cartilage defects of the knee: preliminary results of a spiral CT arthrography-guided analysis. Eur Radiol 14(2):208–214
Hodler J, Resnick D (1996) Current status of imaging of articular cartilage. Skeletal Radiol 25:703–709
Petersson CJ (1983) Degeneration of the gleno-humeral joint. An anatomical study. Acta Orthop Scand 54:277–283
Matthews LS, Scerpella TA (1996) Arthroscopic management of degenerative arthritis of the shoulder. In: McGinty JB (ed) Operative arthroscopy, 2nd ed. Lippincott-Raven, Philadelphia, pp 793–799
Weinstein DM, Bucchieri JS, Pollock RG, Flatow EL, Bigliani LU (2000) Arthroscopic debridement of the shoulder for osteoarthritis. Arthroscopy 16:471–476
Scheibel M, Bartl C, Magosch P, Lichtenberg S, Habermeyer P (2004) Osteochondral autologous transplantation for the treatment of full-thickness articular cartilage defects of the shoulder. J Bone Joint Surg Br 86:991–997
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lecouvet, F.E., Dorzée, B., Dubuc, J.E. et al. Cartilage lesions of the glenohumeral joint: diagnostic effectiveness of multidetector spiral CT arthrography and comparison with arthroscopy. Eur Radiol 17, 1763–1771 (2007). https://doi.org/10.1007/s00330-006-0523-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0523-8