Abstract
Patient dose is usually estimated for a single radiographic projection or computed tomography (CT) series. In this study, patient dose was calculated for predefined clinical indications (24 radiography, 11 CT). Members of the radiology staff of each of 11 hospitals were trained in dose measurement and calculation techniques. Based on clinical indications participants decided on imaging protocols and calculated cumulative effective dose for a complete examination. Effective dose ranged from <1 μSv to 0.6 mSv for examinations with radiographs and from 0.2 to 12 mSv for CT scans. Differences in the imaging protocols contributedd to a substantial variation in patient dose. For mammography, average glandular dose (AGD) was estimated for 32-, 53- and 90-mm compressed breast thicknesses, with a median value of 0.74, 1.74 and 3.40 mGy, respectively. The results presented here demonstrate that a pragmatic choice of dosimetry methods enables local staff to estimate effective dose. The inclusion of imaging protocols in the dose surveys provided a broader view on the variations in patient dose between hospitals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In line with the European council directive 97/43 [1], Dutch legislation requires that the owner of radiology equipment “supplies the data that are needed to estimate mean and spread of effective and equivalent dose in radiological examinations for the general population and relevant reference groups” [2]. For decades, the acquisition of such data was laborious, requiring equipment and an expertise in radiation dosimetry that were not commonly available in a radiology department. Under those circumstances it would have been difficult to fulfill current legal requirements. In recent years, however, new tools have become available, including user-friendly PC software and dosimetry equipment, that are more easily accessible to radiology staff [3–6].
The main goals of the project reported here were threefold: (1) to implement a pragmatic method for clinical patient dosimetry, based on clinical indication; (2) to train radiology staff to a level that they can carry out patient dosimetry and dose calculations independently; (3) to acquire insight in the inter- and intra-departmental spread of patient radiation dose. To this end, data were acquired for the period from late 2001 until early 2004. The dose results were made available to the National Institute for Public Health and the Environment to be incorporated in the Dutch Information System Medical Exposures.
Materials and methods
Approach
Physicians refer patients to the radiology department stating a medical indication, such as ‘hip fracture’, ‘pulmonary metastasis’ or ‘acute stroke’. Radiologists then define the radiographic projections or computed tomography (CT) series that best suit the diagnostic demand. Consequently, patient dose resulting from a clinical examination is not only dependent on the radiation dose for individual radiographs or CT-series but also on the protocol applied. For the purposes of this study and in order to realistically estimate the spread of radiation dose we defined a number of medical indications (see Table 1). Care was taken to include examinations that are performed in high numbers or with high dose levels and which therefore may contribute significantly to collective dose. We then asked radiologists of the participating departments to decide which protocol they preferred for the given indications. Subsequently, all exposure geometries and X-ray techniques applied were recorded. Corresponding dose measurements and calculations were performed to obtain the effective dose for individual exposures, while a summation of these yielded the effective dose to the patient for a complete examination. This approach enabled a comparison between hospitals from a clinical perspective and provided a broader view on the protocols commonly practiced and the associated level and spread of patient dose.
Participants
This was a multicenter study in which five general hospitals, four teaching hospitals and two university hospitals participated. Five hospitals appointed one radiographer to take part in the project, four hospitals appointed two radiographers, and in one hospital three radiographers were involved. In two hospitals other staff members – for example, medical physicist and manager – were available to support the radiographers. To provide insight on possible difficulties, the authors performed measurements and calculations for their own site.
Categories of examinations
Effective dose (E) is the most suitable dose quantity to express and compare patient dose for inhomogeneous exposures [7]. Estimation of E consists of three main components: (1) a description of the X-ray technique parameters and exposure geometry, followed by (2) a dose measurement that is used as input for (3) calculating dose distribution, organ dose in exposed tissues and effective dose. In standard projection radiography, part of the patient anatomy is exposed to a stationary X-ray field that is well defined in the examination protocol. CT requires a different approach in dosimetry because the X-ray tube rotates around the patient while the patient travels through the plane of the X-ray beam. Exposure conditions in mammography are different from other radiological examinations in the sense that risk to the patient is mainly constituted by radiation dose to a single tissue type, the glandular tissue in the breast. Therefore, in mammography, patient dose is expressed as organ dose rather than as effective dose.
Considering exposure conditions and dosimetry methods available that fit well with clinical practice, we separated radiological examinations into three categories: radiography, CT and mammography.
Dosimetric methods for each category
Methods for dose measurement and calculation needed to be easily employed by radiographers while workload was kept to an acceptable level. Hospitals were provided with dose measurement equipment during the project. Care was taken to use methods which are compliant to those already implemented in modern X-ray equipment, thereby ensuring that participating hospitals would be able to continue dose evaluation after the conclusion of the project at a minimal level of cost with respect to both equipment and staff. Because diversity in protocols increased the variation in patient dose, outliers were encountered more often. It was therefore decided to express dose values in terms of median dose. For a broader overview, the percentage coefficient of variation (i.e. standard deviation/mean × 100), the minimum and maximum values and the ratio Emax/Emin are also given.
Radiography
For radiography, dose-area product (DAP) was measured. Primarily due to variations in patient physiques, a reliable estimation of average DAP in patients for any given radiograph requires that an extended effort be made to collect data on a sufficiently large population over a long time period. It was therefore decided to perform dosimetry on an anthropomorphic phantom (Rando man; The Phantom Laboratory, Salem, N.Y.). According to specifications, this phantom represents an average (American) male with a length and weight of 1.75 m and 73.5 kg, respectively. However, as the average length and weight of Dutch males are greater than these parameters, dose measurements on this phantom would result in an underestimation of patient dose for males. Consequently, we considered the Dutch population on a whole (males and females), for which the average length is 1.74 m and the average weight is 74.9 kg [8]. Within this framework, the Rando man can be considered to be representative of the general adult patient.
The phantom was sent to each hospital together with a DAP meter (Diamentor M4, PTW, Freiburg). Radiographers were asked to mimic the clinical situation with respect to projection angle and field size of the X-ray beam. DAP was measured with technique settings (kVp, filter, exposure control) applied according to the clinical protocol. For radiographs without an automatic exposure control (AEC) – i.e. with an X-ray technique set manually–field size was set on an average adult volunteer while the exposure was made without the volunteer. A light visor and a cardboard sheet were used to record field size at the level of the entrance point of the X-ray beam in a plane perpendicular to the central beam. Tube voltage, total beam filtration, focus skin distance (FSD), focus detector distance (FDD) and film-screen or detector system were registered.
The computer program PCXMC ver. 1.5.1 (STUK, Radiation and Nuclear Safety Authority, Helsinki, Finland) was used to calculate E from DAP. This software runs on a personal computer and uses Monte Carlo simulations to calculate photon tracks and organ doses in a mathematical phantom [5]. PCXMC generates three kinds of output files: (1) a geometry file with data on beam size, position and direction; (2) an energy file with data on the Monte Carlo simulation; (3) a dose file that contains E and organ dose for more than 20 different organs.
In addition to total E for all clinical indications, participants were asked to submit DAP, E, technique registration forms and PCXMC files for all radiographs. All incoming data were screened on the level of individual radiographs. The E/DAP ratio (mSv Gy−1 cm−2) proved to be a strong tool for detecting erroneous data. When necessary, participants were contacted and measurements or calculations repeated.
Computed tomography
All hospitals received a CT questionnaire. For each clinical indication the protocol applied was specified, i.e. the number of scans in the series and in each scan, the area of the body scanned and technique settings presented separately. Summation of E for all individual series yielded E for a clinical indication.
CTDosimetry.xls ver. 0.99e developed by ImPACT [4] was used to calculate E in CT. Dose input for CTDosimetry is CT-dose index (DI)-free in air (CTDIair), which was measured on all scanners. To optimize dose calculations, scanner dose characteristics as incorporated in CTDosimetry software were adjusted to local values. To enable this, CTDIc and CTDIp were measured in a cylindrical perspex phantom of 16- and 32-cm diameter for head and body CT scans, respectively, according to international protocols [9]. Dose measurements were performed with a Capintec CT probe model PC-4P connected to a Keithley 35050A dosemeter. CTDIc and CTDIp values were measured on all but one scanner. All CTDI measurements were performed by local radiographers, assisted by the authors, for all relevant kVps and collimations.
As in radiography, results were checked for outliers. The ratio of effective dose/dose length product (E/DLP) served as the primary tool, following which all of the applied techniques were assessed. In case of doubt, the participants were contacted and measurements or calculations repeated.
Mammography
The method described by Dance et al. [10] was used for the dose calculations in mammography. In modern mammography equipment, the kV and anode- and beam filter material are selected (semi-) automatically to optimize image quality and patient dose. During this process the height of the compressor plate over the detector is used as the main input. We performed dose measurements on 30-, 45- and 70-mm-thick polymethyl-methacrylate (PMMA; Perspex), which corresponds with a breast thickness of 32, 53 and 90 mm respectively [10]. To ensure a clinically correct position of the compressor plate, we corrected for the difference in thickness by adding a 2-, 8- or 20-mm thickness of lightweight foam to the PMMA, respectively. With PMMA plus foam in place, an exposure was made using system settings according to clinical practice.
For all thicknesses, incident air kerma at the upper surface without backscatter was measured with a Keithley 35050A electrometer connected to a 0.6-cm3 NE Farmer type ionization chamber. Radiation transmission in 99.99% pure aluminum (filter set type: T43009.1.007-0016; PTW, Freiburg, Germany) was also measured to enable the calculation of half value layers (HVLs). Incident air kerma to average glandular dose conversion factors (g-factor), breast composition correction factor (c-factor) and spectrum correction factors (s-factor) were taken from Dance [10]. To optimize the dose calculations, we adjusted the g- and c-factors for breast thickness and HVL by linear interpolation. The c-factors for age group 50–64 years were applied to all calculations. Dose measurements were performed by participants and authors together; dose calculations were performed only by the authors.
Training
All of the participants were trained in two full-day sessions. During day one, at the start of the project, emphasis was on dosimetry equipment and methods and dose calculations. The training involved hands-on dosimetry with the anthropomorphic phantom and the use of dose calculation software for both radiography and CT. Presentations on practical dose levels and considerations in radiation protection were given to broaden the perspective and for motivation purposes. The second day of training was organized 7 months later. Time was spent on exchanging experiences, and analyses of received data were shown, with special attention given to pitfalls and solutions for problems encountered by the participants. These items were also addressed in newsletters that were sent to participants on a regular basis.
During the whole project the participants were free to contact authors for support.
Results
Radiography
The 24 clinical indications under investigation rendered dose information for 71 different radiographic projections.
Table 2 shows the imaging modalities applied. Film-screen systems are used by four hospitals for all radiographs and by two hospitals for all radiographs except those for chests for which a digital chest system was used. One hospital uses flat panel detectors for all imaging with the exception of those for mobile chests where a film-screen system is used. Four hospitals use phosphor plate technology for all radiographs. The film-screen speed class for extremity examinations is 100–150, although one hospital uses a speed class of 600. For all other examinations a speed class of 400–600 is used. Manufacturer data on speed class for digital systems is not defined uniformly and therefore not compared in this study.
In classic dosimetric studies for individual radiographs, a Emax/Emin ratio of up to a factor of 10 between hospitals is not uncommon. Comparable values were found in this study, as can be seen in Table 3, which gives an overview of a typical effective dose for radiographs that were analyzed by at least ten hospitals.
Using the clinical indication as a starting point, we found a much larger variation in dose due to the contribution of differences in the protocols applied. This is illustrated in Fig. 1a and b, which show cumulative dose for the cervical spine ‘neck pain’ and pelvis ‘fracture’ protocols. While the Emax/Emin ratio for a single anteroposterior (AP) view of the cervical spine and pelvis was 9.9 and 7.7, respectively (see Table 3), it was 12.9 and 23.3 for the complete protocols (see Table 4) due to variations in both geometry and the number of radiographs applied. The strongest influence of diagnostic protocol was found for abdomen ‘free air’, shown in Fig. 1c. Application of a single posteroanterior (PA) left decubitus image that covers only the right-side one-third of the abdomen led to a Emax/Emin >39 for diagnoses of free air.
Table 4 shows effective dose (mSv) in radiography for all clinical indications defined in this study.
From a clinical point of view complete radiography examinations can be divided into three categories: Emedian<1 μSv for examinations of the extremities that do not include part of the trunk, 1 μSv ≤ Emedian<0.1 mSv for examinations superior of the diaphragm (including head and neck), thoracic spine excepted, and 0.1 mSv ≤ Emedian<1 mSv for examinations of the thoracic spine and trunk inferior of the diaphragm.
Computed tomography
All scanners included in this study were capable of spiral acquisition, varying from single row to 16-detector row technique.
The influence of diagnostic protocols on patient dose was also clearly observable in CT. Figure 2 shows the results for examinations for ‘liver metastases’. In this example, the Emax/Emin ratio for the whole abdomen and arterial phase of the liver was 1.9 and 3.4, respectively, and 6.2 for the complete examinations. As in radiography, variations in dose for a given clinical indication showed a minimum Emax/Emin ratio of about 3. In radiography, however, high Emax/Emin ratios are encountered more often than in CT, probably due to better international agreements on imaging protocols and techniques. Table 5 shows the effective dose for the investigated CT examinations.
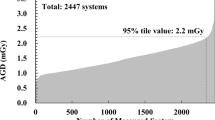
Mammography
Average glandular dose (AGD) was estimated for all three breast thicknesses on 12 mammography systems, nine using film-screen combinations and three using phosphor plates. Compressor plate height is of importance in systems that automatically adjust exposure technique. For example, on all three Siemens Mammomat 3000 systems under investigation a molybdenum/molybdenum (Mo/Mo) anode/filter combination was selected automatically for the 45-mm-thick perspex phantom; however, a Mo/rhodium (Rh) combination was automatically selected when 8 mm of foam was added to get the compressor plate to the corresponding breast thickness of 53 mm. Figure 3 shows the first HVL for all techniques encountered. A tendency towards a higher HVL with increasing atomic number of the anode and filter material can be observed. The Mo/Mo combination showed a higher HVL with higher kVp; however, other anode/filter combinations do not demonstrate this trend. This can be explained by the relatively low number of measurements and the fact that systems of several manufacturers are involved, and these may result in different inherent filtration. For one system, an outlying HVL value of 0.304 mm Al was calculated for a Mo/Rh combination at 31 kVp. Following this result, the mammography system was inspected, revealing that Rh filter was missing; this result is denoted as Mo/- in Fig. 3.
Table 6 shows the AGD for 32- 53- and 90-mm compressed breast thickness for all hospitals. No value for location K1, 90-mm thickness is presented because of the missing beam filter. Values represent AGD for a single exposure of the standard phantom with clinical technique settings. Compared with radiography and CT, patient dose in mammography shows the smallest variation with a AGDmax/AGDmin ratio <3 for all three breast thicknesses. This can be attributed to the thorough optimization of X-ray techniques in mammography.
Discussion
The dosimetry methods applied in this study were chosen for their relative simplicity and easy adoption in a clinical environment. To avoid the influence of patient size, we used an anthropomorphic phantom for the radiographic measurements. According to specifications, the phantom is constructed with a natural human skeleton cast inside material that is radiologically equivalent to soft tissue, and the lungs are represented by material that simulates a median respiratory state. In addition the size and weight of the phantom correspond well with those of the average Dutch adult. It is therefore assumed that dose values are also representative of the average Dutch adult. The radiological representation of the anthropomorphic phantom relative to the situation in vivo was beyond the scope of this study.
The dose values reported in this study represent standard radiological procedures – for average Dutch adults and for given clinical indications. In clinical practice, however, patient dose will vary with patient size, and retakes after a bad exposure or faulty positioning may lead to higher dose values. These factors were not taken into account in this study, and together with the use of an anthropomorphic phantom they may be considered to be limitations of the study.
In this study, one phantom was acquired; this was stationed at a central location and transported to a hospital when needed as for most hospitals the cost of such a phantom would impose too large a burden on the financial budget. As an alternative, data can be acquired from clinical examinations, although this will require data collection on a sufficiently large number of patients. Modern X-ray equipment is provided with a built-in DAP meter. Clinical experience has taught that it is necessary to perform calibration measurements before using a built-in DAP meter for patient dosimetry.
A comparison of results from this study with those published in the literature is difficult. In earlier studies, Entrance Skin Dose or DAP were often measured for individual X-ray projections, or DAP was used for combinations on projections (for example, AP and lateral). More recent studies report DAP values for the complete examination of a given anatomical area, however, without differentiation of clinical indication. Table 7 gives an overview of values found in other studies [11–13] that we consider to be the best suited for comparison with the results of the present study.
In addition, with respect to the measurements required for this study, the authors also analyzed in detail the collective effective dose for radiology examinations over a 1-year period in their radiology department. We concluded that examinations involving the chest, thoracic spine, lumbar spine, abdomen, hips or pelvis deliver 88% of the collective dose in radiographic examinations. For monitoring patient dose in radiography, it would therefore appear to be sufficient to restrict dose measurements to these examinations to fulfill legislative demands. When the department was considered as a whole, 69% of the collective dose came from CT alone. Information from other participants indicates that CT plays a similar major role in patient dose in all hospitals.
Table 8 shows the results for CT compared with those reported in the literature [14–17]. Because of a lack of median values in these publications, Table 8 shows mean effective dose.
Overall, results in this study are comparable to those reported elsewhere. High mean effective dose in ‘Abdomen, liver metastases from primary colon carcinoma’ is a result of the extensive protocol some hospitals apply. However, a multi-phase liver scan, with blank, arterial portal and late phase, is considered to be justifiable for the indication ‘primary liver tumor’ by other hospitals. In these locations, a more basic scan routine is applied that consists of a contrast-enhanced abdomen only. This difference in approach results in a relatively high percentage coefficient of variation (%CV).
The high %CV for ‘Chest, HiRes’ can be attributed to differences in slice thickness, the number of slices imaged (except for one, all locations apply incremental CT) and whether one or two series, expiration and inspiration, are executed.
As mentioned earlier, measurements in mammography were performed by participants and authors together. Although radiographers should be able to perform these measurements autonomously after some additional training, dose calculations are complex and should be performed by personnel with experience in mammography dosimetry. The measurement results in this study led to the discontinuation of mammography in a unit with a beam filter missing and the replacement of intensifier screens in another location. In 2001, Kruger and Schueler published a comparison of compressed breast thickness and AGD values for film-screen mammography (craniocaudal view) [18]. The average breast thickness and AGD, and their corresponding ranges, calculated from nine studies that were compared, are respectively 50 (45–52) mm and 2.0 (1.3–2.8) mGy. Most of the results from our current study for a breast thickness of 53 mm fall well within this range; at two locations we even assessed an AGD lower than 1.3 mGy – namely 0.9 and 1.1 mGy.
For dose measurements in examinations that incorporate fluoroscopy, participants were provided with a DAP meter to install in a fluoroscopy suite of their choice. Participants recorded cumulative DAP per examination. However, because of the large variation in both type of examination and number of results for a given examination type, data were considered too heterogeneous for publication. The data did, however, confirm our experience that dose estimation in fluoroscopy examinations is complex [19, 20] and that it requires continuous staff motivation and discipline to render reliable data within an acceptable time frame.
Conclusions
When patient dose in different hospitals is compared, clinical protocols have to be included in the analysis for they can have a profound effect on spread in dose values. In radiography, a difference between the lowest and highest effective patient dose for a given clinical indication of a factor 3–25 is not uncommon; in CT, this ratio ranges from 3 to 15. In mammography, the highest AGD is less than threefold higher than the lowest dose found. A better agreement on imaging techniques and protocols appears to lead to a reduction in dose variation.
Following 2 days of training the radiology personnel in each hospital were capable of carrying out the required dose measurements and calculations for estimating the effective dose in the radiography and CT examinations. However, supervision by someone with sufficient experience in dosimetry – for example, a medical physicist – was found to be necessary.
The involvement of local staff proved to be very efficient for a broad survey of dose values that represent clinical practice. Also, it provided a deeper insight into examination protocols and conditions that should be met to enable autonomous and reliable estimation of patient dose.
Median effective dose for a complete examination with radiographs was found to vary from <1 μSv to 0.6 mSv, depending on the anatomy under investigation and the protocol used. In CT, median effective dose varied from 0.2 mSv for a low-dose sinus protocol to 12 mSv for an extensive liver examination.
By applying the methods described in this study, radiology departments can easily meet the criteria set by European legislation for monitoring patient dose.
References
European Union (1997) Council Directive 97/43/Euratom. On health protection of individuals against the dangers of ionizing radiation in relation to medical exposure. Luxembourg
Staatsblad van het Koninkrijk der Nederlanden, Besluit Stralenbescherming, 16 juli 2001, Stb. 2001, 397
CT dose calculator ImpactDose, VAMP GmbH, Erlangen Germany. Internet: http://www.vamp-gmbh.de/software/impactdose.php
ImPACT (Imaging Performance Assessment of CT) group. CTdosimetry.xls spreadsheet can be downloaded from http://www.impactscan.org/ctdosimetry.htm. In this study, version 0.99e was used
Tapiovaara M, Lakkisto M, Servomaa A (1997) PCXMC: A PC-based Monte Carlo program for calculating patient doses in medical x-ray examinations, report STUK-A139, Helsinki: Finnish Centre for Radiation and Nuclear Safety. For information and demo version. see http://www.stuk.fi/pcxmc/
Radiography dose calculator: WinODS, RTI Electronics AB, Mölndal, Sweden. Internet: http://www.rti.se/products_accessories/software.htm
ICRP publication 60 (1991) 1990 Recommendations of the International Commission on Radiological Protection. Pergamon Press, Oxford, UK
Length and weight of the Dutch population, 1998/2000. Statistics Netherlands, Voorburg/Heerlen
European Commission (1999) EUR 16262 – European guidelines on quality criteria for computed tomography. Luxembourg, Office for Official Publications of the European Communities
Dance DR, Skinner CL, Young KC, Becket JR, Kotre CJ (2000) Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol 45:3225–3240
Grøn P, Olerud HM, Einarsson G, Leitz W, Servomaa A, Schoultz BW, Hjardemaal O (2000) A nordic survey of patient doses in diagnostic radiology. Eur Radiol 10:1988–1992
Leitz W, Jönsson H (2001) Patientdoser från röntgenundersökningar I Sverge, sammanställning av resultaten från sjukvårdens rapportering (1999). SSI Rapport 2001–2001. Swedish Radiation Protection Institute, Stockholm
Hart D, Wall BF (2002) Radiation exposure of the UK population from medical and dental X-ray examinations. National Radiological Protection Board publication NRPB-W4, Chilton
Shrimpton PC, Hillier MC, Lewis MA, Dunn M (2005) Doses from computed tomography (CT) examinations in the UK – 2003 review. National Radiological Protection Board publication NRPB-W67, Chilton
Clarke J, Cranley K, Robinson J, Smith PHS, Workman A (2000) Application of draft European Commission reference levels to a regional CT dose survey. Br J Radiol 73:43–50, Jan
Origgi D, Vigorito S, Villa G, Bellomi M, Tosi G (2006) Survey of computed tomography techniques and absorbed dose in Italian hospitals: a comparison between two methods to estimate the dose-length product and the effective dose and to verify fulfilment of the diagnostic reference levels. Eur Radiol 16:227–237, Jan
Brix G, Nagel HD, Stamm G, Veit R, Lechel U, Griebel J, Galanski M (2003) Radiation exposure in multi-slice versus single-slice spiral CT: results of a nationwide survey. Eur Radiol 13:1979–1991, Aug
Kruger RL, Schueler BA (2001) A survey of clinical factors and patient dose in mammography. Med Phys 28:1449–1454, Jul
Geleijns J, Broerse JJ, Shaw MP, Schultz FW, Teeuwisse W, van Unnik JG, Zoetelief J (1997) Patient dose due to colon examination: dose assessment and results from a survey in The Netherlands. Radiology 204:553–559, Aug
Geleijns J, Broerse JJ, Chandie Shaw MP, Schultz FW, Teeuwisse W, Van Unnik JG, Zoetelief J (1998) A comparison of patient dose for examinations of the upper gastrointestinal tract at 11 conventional and digital X-ray units in The Netherlands. Br J Radiol 71:745–753
Acknowledgements
This project was supported by ZorgOnderzoek Nederland, project no. 1630-0004. The authors would like to thank Bianca Alsemgeest, Marinka van Asselt, Edwin van Harn, Willy Hummel, Matthijs Huttinga, Rinke Kattenberg, Martin Kuikman, Michael Melis, Arjen van der Most, Willem Rasenberg, Kees Roscher, Enouschka Schleurholts, Wouter Stam, Lamberta Wielinga, Nienke vd Zee, Rintje Zijlstra and Luc Zwart for their enthusiastic participation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teeuwisse, W., Geleijns, J. & Veldkamp, W. An inter-hospital comparison of patient dose based on clinical indications. Eur Radiol 17, 1795–1805 (2007). https://doi.org/10.1007/s00330-006-0473-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0473-1