Abstract
A wide variety of artifacts can be seen in clinical MR imaging. This review describes the most important and most prevalent of them, including magnetic susceptibility artifacts and motion artifacts, aliasing, chemical-shift, zipper, zebra, central point, and truncation artifacts. Although the elimination of some artifacts may require a service engineer, the radiologist and MR technologist have the responsibility to recognize MR imaging problems. This review shows the typical MR appearance of the described artifacts, explains their physical basis, and shows the way to solve them in daily practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Artifacts are often encountered during magnetic resonance (MR) imaging. They are defined as either any signal or void in the images that does not have an anatomic basis, or as the result of distortion, addition or deletion of information. Some of them are obvious and some are subtle. The latter may potentially lead to misinterpretation or misdiagnosis, especially when simulating pathologic conditions.
Some artifacts are due to scanner equipment malfunction, others due to inappropriate technique choice, and some are inherent to the MRI physics.
The prerequisite requirement of recognition and understanding is knowledge of the physical principles, familiarity with scanner techniques and theory of image formation. With this understanding many artifacts may be corrected, minimized or avoided. However the complexity and variety of imaging techniques and sequences make identification and minimization of artifacts sometimes difficult. In spite of these difficulties, the study of artifacts can be a step into a deeper understanding of the MRI principles.
This article gives an overview of the MR appearances and origins of the most common artifacts in body MR imaging along with ways to avoid or minimize them. For more technical details some excellent textbooks are available [1–4].
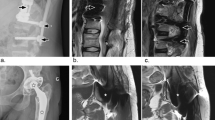
Truncation
Truncation or Gibbs artifacts are bright or dark lines that are seen parallel to edges of abrupt intensity change, sometime also described as “ringing” type of artifact following signal intensity borders (Fig. 1). They are observed particularly in brain and spine imaging, sometimes leading to interpretation problems, e.g., mimicking a syrinx.
This artifact is related to the finite number of encoding steps used by the Fourier transform to reconstruct an image. To understand the physical background, it is necessary to remember that sharp edged borders between areas of high contrast are represented by high spatial frequency data. The highest sampled frequency is inversely proportional to the pixel size, i.e., the smaller the pixel size, the higher the sampled frequency. Undersampling, e.g., by using smaller numbers of phase encoding steps to save time, means cutting off the highest frequencies, leading to incorrect imaging of sharp edges fine lines. The more encoding steps, the narrower the artifacts (with the same amplitude), making the artifact less visible.
As a fundamental effect of Fourier analysis, this effect is seen both in phase- and frequency-encoding direction. However, in most examinations the phase encoding steps are fewer than the frequency encoding steps, making the effect more visible in the phase direction.
Mathematical methods to extrapolate the higher frequency data were developed, but are not in widespread clinical use.

Aliasing
Maybe the most common artifact is aliasing or wrap-around (Fig. 2). It can occur whenever any part of the body extends outside the FOV and a signal produced by this structure reaches the receiver coil [5]. The body part that lies outside the FOV is wrapped inside to the opposite side of the image. In most cases this artifact is easily recognized and does not simulate disease; however, it can mask anatomical structures in the FOV.
The physical background lies in the fact that the continuous signal received from the object is converted into a digital value, a process called sampling. As a result of this sampling procedure the frequency values of signal from outside the FOV is somehow misinterpreted by the image-forming reconstruction algorithm as originating from inside the FOV. The physical principle of this effect is the same as in the aliasing effect known in many other imaging procedures, for example in Doppler ultrasound. In analogy for the phase-encoding direction the phase of the signal originating from inside the FOV has a range from 0°–360°. Due to the circular nature of phase a signal from outside the FOV with a phase of 400° (= 360° + 40°), for example, is not distinguishable from a phase of 40° from inside the FOV. Thus, the part of the body that lies beyond the borders of the FOV is wrapped into the other side of the image [6]. The physical principle of this effect is equal to the reverse spoke wheel effect seen in old western movies.
Aliasing in the frequency-encode direction can be eliminated by applying a low-pass filter on the signal (“No frequency wrap”), leading to attenuation of the higher frequencies from outside the FOV, and oversampling in the frequency encode direction. This means that the signal is measured in closer steps than would be necessary for the chosen FOV. These methods do not result in longer acquisition times. Technically speaking, the minimal sampling rate, known as the Nyquist frequency has to be twice the signal bandwidth [7].
Unfortunately there is no simple way to eliminate phase aliasing like filtering as is possible with frequency aliasing (Fig. 3). One possible solution to eliminate a wrap around artifact, called No Phase Wrap (NPW) or other equivalent vendor dependent functions (Phase Oversampling, Anti-wrap, Fold Over Suppression, Anti-alias), is based on a larger measured FOV to cover all the signal producing structures. A typical value is to double the size in the phase encoding direction. To maintain the spatial resolution the number of phase-encoding steps has also to be doubled and to keep the scan time constant, the number of averages has to be halved, if possible. This technique does not necessarily lead to loss of image quality because the additional phase encoding steps improve the signal to noise ratio. Finally, the information in the double-sized region of the field of view is eliminated.
Wraparound artifact. a: Axial T1 weighted image (GRE, TR 80 ms, TE 6.9 ms) shows wraparound of the parts of the lateral body wall, which are outside of the FOV, in the left-right phase encoding direction. b: Repeat scan with identical parameters but after switching the phase encoding direction to anterior-posterior. c: Wraparound disappears after applying the foldover suppression option of the scanner
Another principle to eliminate aliasing artifacts is to decrease the signal coming from structures outside the FOV. This can be done by applying special presaturation pulses or using surface coils, which have low sensitivity for distant signals.
A special appearance of aliasing artifacts can be seen in 3D imaging (Fig. 4). The same principle like in 2D imaging can lead to wrap around artifacts in the second phase encoding direction used for the slice definition. In this case, an entire slice moves from out of the FOV in the z-axis to the middle of the stack, being superimposed onto the image [7]. The principle of eliminating this artifact is not different from the 2D no phase wrap techniques. Additionally it is possible to excite only a limited part of the volume in the z-direction by applying a z-gradient pulse during the RF excitation.
The combination of aliasing artifacts and field inhomogeneity can lead to Moire fringes or zebra artifacts (Fig. 5). Basically these are interference patterns of superimposed images with different phases from one side of the body to the other that alternatively add and cancel [1]. These are especially seen in gradient echo techniques.
In parallel acquisition techniques like SENSE (or IPAD, ASSET of other vendors) aliasing artifacts have a different appearance. If the object size is larger than the FOV a so called SENSE ghost can be seen in the central portion of the SENSE images (Fig. 6). The location of the ghost depends on the SENSE factor [8]. The SENSE ghost moves toward the edge of the image as the SENSE factor is reduced. If the SENSE factor is zero the artifact transforms to conventional aliasing. Thus, parallel reconstruction techniques can reduce the fold-over component resulting from the reduced sampling of k-space lines, but not the additional fold-over from a reduced FOV.
SENSE-ghost artifact. Axial T1 weighted opposed phase GRE image demonstrating the effect of the SENSE factor on the position of the SENSE ghost. The position of the SENSE ghost (arrows) depends on the SENSE factor (SENSE factor: a = 1.7, b = 1.3, c = SENSE deactivated). 5a illustrates the term “hot lips” artifact for the SENSE-ghost artifact. In 5c the SENSE artifact transforms to a normal aliasing artifact

Magnetic susceptibility artifact
Magnetic susceptibility artifacts are the result of microscopic gradients of the magnetic field strength at the interfaces of regions of different magnetic susceptibility. Susceptibility describes the property of matter of becoming magnetized when exposed to a magnetic field. Paramagnetic materials (e.g., platinum, titanium, and gadolinium) have positive susceptibility and augment the external field. Diamagnetic substances (water, most biological substances) have negative susceptibility and slightly weaken the external field. Ferromagnetic materials (iron, cobalt, nickel) have strong nonlinear positive susceptibility [7]. Between these values lies air with a susceptibility of approximately zero.
There are two main effects of magnetic susceptibility. First, ferromagnetic materials can lead to a strong distortion of the B0 field and the linearity of the frequency encoding gradient close to the object. This frequency shift results in geometric distortion of the image (Fig. 7) [7, 9]. Second, susceptibility gradients result in different precession frequencies of adjacent protons, resulting in stronger dephasing of spins. The net results are bright and dark areas with spatial distortion of surrounding anatomy [10, 11].
Susceptibility artifact. Two manifestations of a susceptibility artifact originating from a metallic part of a catheter: a (SE, TR 11 ms, TE 5 ms) shows severe blooming around the ferromagnetic material, whereas b (SE, TR 4500 ms, TE 96 ms) shows bizarre distortion of the abdominal wall of the same patient
Although ferromagnetic objects lead to the most severe artifacts (Figs. 8, 9), such effects can also be found at the boundary of tissues with different susceptibilities, such as bone, brain and air. The artifacts can be seen for example around the paranasal sinuses the sella and around air filled bowel loops [12]. Increasing field strength is worsening the magnitude of this effect.
Susceptibility artifact. a: A seven year old boy was referred to a MRI of the spine. Repeated scout views showed large areas of signal void (GRE, TR 15 ms, TE 3.5 ms). The equipment was checked, without change of the effect. b: Fluoroscopy showed a metallic foreign body in the left abdomen, which turned out to be a part of a magnetically toy which was swallowed by the child
Susceptibility artifacts are worst with long echo times (giving the spins more time to diphase) and with gradient echo sequences [13]. Spin echo sequences are using a 180° RF to rephase the transverse magnetization to minimize the artifact. Gradient echo sequences using gradient reversal can not rephase to minimize the signal loss caused by local field inhomogeneities (Fig. 10). The best combination of spin echo and short TE are found in fast spin echo techniques rather than in conventional spin echo [14]. Increasing the frequency matrix and decreasing the slice thickness can also contribute to reduce the artifact size. A slight reduction of the artifact can also be achieved by using wide bandwidth techniques increasing gradient strength.

Central point artifact
The central point artifact is a focal dot of increased or decreased signal in the exact center of an image, often with a surrounding ringing artifact (Fig. 11).
This effect is the result of the Fourier transform of a constant offset in the raw data, which is caused by an offset of the receiver signal as a result of an error in receiver electronics [6]. Today, with the quality of the hardware, this artifact is only occasionally seen.
One technique to avoid this effect is based on phase alternation of two RF excitation pulses, cancelling out the signal offset at the cost of doubling the required number of pulses (i.e., doubling the acquisition time). A modification of this technique, which does not double the number of pulses, leads to bright lines on the top and bottom of the FOV. Additionally, self calibrating techniques of the receiver and software correction minimize the effect.

Zipper artifacts
These artifacts appear as discrete lines of noise or alternating bright and dark pixels in a line across the image in the phase encoding direction (Fig. 12).
There are many causes for this type of artifacts, most of them are based on hardware problems [6, 15]. A subgroup of causes is based on interference of extrinsic RF into an MRI system. There are many possible sources of this extrinsic RF: penetration of the scanning room, especially through open doors, electronic devices (e.g., monitoring equipment), static electricity (wool blanket), RF noise from defect light bulbs in the MR room. Width and position of the artifact depends on the frequency and bandwidth of the extrinsic signal. A specific appearance of this family of artifacts is the so called crisscross or herringbone artifact, resulting from a more discrete or spike formed radiofrequency external signal (Fig. 13).

Central artifacts
This artifact manifests itself as a bright signal at the central line either along the phase or the frequency encoding direction. However, the causes of the artifacts are different for the two directions [6].
Artifacts in the phase encoding direction result from RF feed-through from the transmitter, which is not completely gated off at the end of the pulse and the RF receiver. These artifacts are eliminated by sequence-built in alternating phase of paired excitation pulses.
Artifacts in the frequency encoding directions result from imperfect 180° pulse in SE sequences (note that the position in phase-encoded direction is fixed prior to the 180° pulse and so it is not affected). The 180° pulse is altered by interfering parts of the FID (free induction decay) after the 90° excitation pulse. To overcome this overlap of the signals, one can enlarge the gap between them (i.e., to increase TE), or to make the 180° pulse “narrower” by increasing the RF bandwidth of the signal (practically done by increasing slice thickness).
Closely related to the latter are artifacts originating from imperfect 180° pulses due to interference events in multiecho sequences or crosstalk with other slices. A potential solution is to apply spoiler gradients to destroy the interfering signals or to increase the interslice gap. These artifacts do also appear not only as line, but also as noise band in frequency encoding direction.

Motion
Motion is a very common artifact especially in body imaging and can be seen from heart or arterial pulsations, breathing, swallowing, peristalsis, tremor and gross movement of a patient [16]. The appearance of motion artifact is dependent if the motion is mainly random or periodic [17].
Random motion during the imaging sequence generally results in a blurring of the image (Figs. 14, 15), periodic motion produces ghost images (Fig. 15). The motion artifact is only apparent in the phase encoding direction [7]. Note that motion in all three planes, not only in phase encoding direction, leads to ghosts or blurring in the phase encoding direction. This is because normally patient motion is much slower than the fast sampling process along the frequency encoding direction which is in the order of milliseconds. So motion artifacts along the frequency encoding direction can occur, but they are only detected as slight blurring. On the other hand, sampling along the phase encoding direction needs all phase encoding steps and thus it is in the order of seconds. In this longer period in time the amount of motion can be large enough to result in disturbing artifacts.
Despite the fact that the mathematical background of ghost formation is quite subtle, the localisation of the ghost images in strictly periodic motion can be predicted with a simple formula, which describes the distance between the original structure and the ghost image of it: [7].
Thus, the higher the frequency (e.g., heart rate) of a pulsating vessel, the larger the distance between the original and the ghost vessel. The amplitude of the motion defines the brightness of the ghost, the larger the pulsation, the brighter the ghost. One possibility to eliminate the ghost is to increase the distance, so that the first ghost lies outside the image. However, increasing TR, phase encoding steps or NEX all result in longer scan time (Figs. 16, 17).
If the movement is sufficiently periodic it is possible to gate the sequence to the movement, for example the respiratory or cardiac cycle [18–20]. For imaging of the heart or the great vessels, this can be done by triggering the acquisition of phase encoding steps at a fixed time in the cardiac cycle, which means that in every phase encoding step the structure is in the same position. Respiratory gating can eliminate ghosting and blurring from diaphragm motion. However, gating methods are inefficient because only the data collected in specific parts of the cardiac or respiratory cycle can be used for image formation. This results in a considerable increase of scan time and long TR times. The more subtle techniques are based on re-ordering the k-space lines such that adjacent samples in the final data set have minimal differences in respiratory phase. These so-called respiratory compensation methods have only little time penalty, but are less effective in non-periodic breathing.
One possibility to reduce the artifact is to lower the original signal of the moving structure. Vessel pulsation artifacts can be reduced by spatial presaturation pulses to saturate the inflowing protons, e.g., presaturation pulses applied cranially to the acquisition slab in the abdomen will eliminate arterial pulsation artifacts. Vice versa an inferiorly placed presaturation slab will eliminate artifacts from venous inflow in the iliac veins. Presaturation pulses can also reduce swallowing and breathing artifacts if the moving structure is out of the region of interest. Likewise, surface coils can be used to focus the image to a non-moving region of interest. By using multiple averages random motion can be reduced substantially, with a minimal number of averages of four to six making this method very time consuming.
Recently, the advent of parallel imaging methods provides some new methods of reducing motion artifacts by using the extra information from the multiple coils [21].
Finally, it is often the solution to immobilize the patient by clear instructions (“don’t move”, “don’t breathe”, “don’t swallow”), fixation or sedation, which are clearly more effective if faster sequences are used. Involuntary movement like peristalsis can often be diminished with drugs, and additionally by using very fast sequences (e.g., HASTE) [22].

Chemical shift
Chemical shift artifact is a very common phenomenon especially in abdominal and spine imaging [22, 23]. It is manifested as bright or dark outlines at fat-water interfaces. It can be divided into two subtypes, known as chemical shift artifact of the first and second kind.
The physical key fact of these artifacts is a shift of the Larmor frequency of water and fat protons, due to a little difference of the local magnetic field which is caused by shielding electron clouds (“chemical”). The difference in frequency is approximately 3.5 ppm which at 1.5 Tesla corresponds to a shift of approximately 220 Hz (and analogically 440 Hz at 3 T).
In the frequency-encoding direction, the frequency of the signal is used to define spatial position. The effect of a shift in frequency encoding direction causes a black border at one fat-water interface, and a bright border at the opposite interface. This is called chemical shift artifact of the first kind (Figs. 18, 19). The actual spatial difference is further defined by the bandwidth and the matrix. For example, bandwidth (BW) of 32 kHz at a matrix of 256 pixel results in a BW/pixel of 125 Hz, thus a difference of 220 Hz corresponds to a position shift of 220 Hz/125 Hz = 1.8. Accordingly, a BW of 16 kHz with a 512 matrix using a 3 T equipment results in a shift of 14 pixels. Thus the degree of the effect can be altered by choosing adequate pixel matrix and bandwidth parameters, with a potential negative tradeoff on image resolution or SNR.
Chemical shift artifact of the first and second kind. Chemical shift of the first kind (left) on the T1w in-phase GRE image (TR 100 ms, TE 4.4 ms) shows a dark rim in the posterior kidney-fat interface. Frequency encoding direction is anterior-posterior. Chemical-shift artifact of the second kind: T1w opposed-phase GRE image (right) (TR 100 ms, TE 2.2 ms) shows a surrounding dark rim at the fat-tissue interface, independent of the frequency encoding direction
In conventional SE and GE sequences there are no visible chemical shift effects in phase encoding direction, which is not true for EPI sequences, where the effect is seen in phase encoding direction.
A different appearance of chemical shift artifacts is called chemical shift artifact of the second kind can be seen in GRE imaging [24]. The effect is based on the fact that there is a difference of the precession frequency between fat and water protons. This means that at particular time points the signals of water and fat protons cancel each other out (out of phase or opposed phase) or are amplified (in phase). At 1.5 T cancellation happens at 2.2 ms and amplification at 4.4 ms. If the signal measurement (i.e., TE) is performed at 2.2 ms a typical black rim is seen at the interface between fat and water containing tissue, where water and protons are found in one voxel (Fig. 19). Note that the same effect is seen in periodic values of a TE of 2.2 ms (e.g., 11.0 ms = 5 × 2.2 ms).
This type of chemical shift artifact is inherent to GRE imaging and is also used for diagnostic purposes [25]: the signal intensity drop of tissues on opposed-phases (versus in-phase images) indicates the presence of fat, which helps to make the diagnosis of adrenal adenoma [26] and fatty infiltration of the liver [27]. However, effect of chemical shift can be diminished by lowering the fat signal by choosing long TE or applying fat suppression techniques.

Crosstalk
Crosstalk is caused by the imperfect shape of the RF slice profiles, which should ideally be rectangular but are in reality more curve shaped. As a result of this the adjacent slices can overlap (“crosstalk”). Tissue in that overlapping region is excited in both slices leading to a saturation effect, which results in decreased signal intensity (Fig. 20) [28].
This artifact can be eliminated by setting the minimum spacing to a gap of more than 10% between the slices [29]. For inversion recovery sequences the slice profiles are worse so the gap should be 20% minimum. Another method of reducing the crosstalk artifact is the use of interleaved slices.

Partial volume
Partial volume artifact occurs when a voxel signal represents an average of different tissues, which results in a loss of resolution [9]. To avoid this artifact, thinner slices should be chosen, but this can lead to a poor signal to noise ratio.
In contrast studies, if an enhancing tumor, which is surrounded by fat, occupies less than 50–60% of the slice thickness, it can become undetectable on opposed-phase images. The reason is that due to signal cancellation of fat on the opposed-image, no signal change or even signal decrease results, as compared to the in-phase images [30]. Equivalent effects can be seen in fat suppressed contrast enhanced studies as compared to non-fat suppressed pre-contrast studies.

Summary
A wide variety of artifacts can be found in clinical MR imaging.
Although reduction of some artifacts may require a service engineer, the radiologist has the responsibility to recognize MR imaging problems. As a motivation to go deeper into the matter, this article gives a short review of the appearances and origins of the most common artifacts in MRI along with ways to avoid or minimize them. But the most important advice for minimizing artifacts and improving image quality is a basic knowledge of artifacts in general and to familiarize with the MR unit you work with.
References
Haacke EM, Brown RW, Thompson MR, Venkatesan R (1999) Magnetic resonance imaging: physical principle and image design. Wiley-Liss, New York
Hashemi RH, Bradley WG (2003) MRI the basics. Lippincott Williams and Wilkins, Baltimore
Bernstein MA, King KF, Zhou XJ (2004) Handbook of MRI Pulse Sequences. Elsevier, San Diego
Vlaardingerbroek MT, den Boer JA (1999) Magnetic Resonance Imaging. Springer, Berlin Heidelberg, 111–112
Pusey E, Yoon C, Anselmo ML, Lufkin RB (1988) Aliasing artifacts in MR imaging. Comput Med Imaging Graph 12:219–224
Weseby G, Adamis MK, Edelman RE (1996) Artifact in MRI: description, causes, and solutions. In: Edelman RE, Zlatkin MB, Hesselink JR (eds) Clinical Magnetic Resonance Imaging, 2nd ed. Volume 1, Saunders, Philadelphia, PA, 88–142
Arena L, Morehouse HT, Safir J (1995) MR imaging artifacts that simulate disease: how to recognize and eliminate them. Radiographics 15:1373–1394
Goldfarb JW (2004) The SENSE ghost: field-of-view restrictions for SENSE imaging. J Magn Reson Imaging 20:1046–1051
Taber KH, Herrick RC, Weathers SW, Kumar AJ, Schomer DF, Hayman LA (1998) Pitfalls and artifacts encountered in clinical MR imaging of the spine. Radiographics 18:1499–1521
Shellock FG, Morisoli SM (1994) Ex vivo evaluation of ferromagnetism, heating, and artifacts produced by heart valve prostheses exposed to a 1.5-T MR system. J Magn Reson Imaging 4:756–758
Shellock FG, Shellock VJ (1996) Vascular access ports and catheters: ex vivo testing of ferromagnetism, heating, and artifacts associated with MR imaging. Magn Reson Imaging 14:443–447
Elster AD (1993) Sellar susceptibility artifacts: theory and implications. AJNR Am J Neuroradiol 14:129–136
Czervionke LF, Daniels DL, Wehrli FW, Mark LP, Hendrix LE, Strandt JA, Williams AL, Haughton VM (1988) Magnetic susceptibility artifacts in gradient-recalled echo MR imaging. AJNR Am J Neuroradiol 9:1149–1155
Port JD, Pomper MG (2000) Quantification and minimization of magnetic susceptibility artifacts on GRE images. J Comput Assist Tomogr 24:958–964
Schiebler ML, Listerud J (1992) Common artifacts encountered in thoracic magnetic resonance imaging: recognition, derivation, and solutions. Top Magn Reson Imaging 4:1–17
Mirowitz SA (1998) Diagnostic pitfalls and artifacts in abdominal MR imaging: a review. Radiology 208:577–589
Wood ML, Henkelman RM (1985) MR image artifacts from periodic motion. Med Phys 12:143–151
Barish MA, Jara H (1999) Motion artifact control in body MR imaging. Magn Reson Imaging Clin N Am 7:289–301
Huber ME, Hengesbach D, Botnar RM, Kissinger KV, Boesiger P, Manning WJ, Stuber M (2001) Motion artifact reduction and vessel enhancement for free-breathing navigator-gated coronary MRA using 3D k-space reordering. Magn Reson Med 45:645–652
Gazelle GS, Saini S, Hahn PF, Goldberg MA, Halpern EF (1994) MR imaging of the liver at 1.5 T: value of signal averaging in suppressing motion artifacts. AJR Am J Roentgenol 163:335–337
Larkman DJ, Atkinson D, Hajnal JV (2004) Artifact reduction using parallel imaging methods. Top Magn Reson Imaging 15:267–275
Mitchell DG (1992) Abdominal magnetic resonance imaging: optimization and artifact suppression. Top Magn Reson Imaging 4:18–34
Peh WC, Chan JH (2001) Artifacts in musculoskeletal magnetic resonance imaging: identification and correction. Skeletal Radiol 30:179–191
Wehrli FW, Perkins TG, Shimakawa A, Roberts F (1987) Chemical shift-induced amplitude modulations in images obtained with gradient refocusing. Magn Reson Imaging 5:157–158
Hood MN, Ho VB, Smirniotopoulos JG, Szumowski J (1999) Chemical shift: the artifact and clinical tool revisited. Radiographics 19:357–371
Boland GW, Lee MJ (1995) Magnetic resonance imaging of the adrenal gland. Crit Rev Diagn Imaging 36:115–174
Venkataraman S, Braga L, Semelka RC (2002) Imaging the fatty liver. Magn Reson Imaging Clin N Am 10:93–103
Schwaighofer BW, Yu KK, Mattrey RF (1989) Diagnostic significance of interslice gap and imaging volume in body MR imaging. AJR Am J Roentgenol 153:629–632
Kneeland JB, Shimakawa A, Wehrli FW (1986) Effect of intersection spacing on MR image contrast and study time. Radiology 158:819–822
Heywang-Kobrunner SH, Wolf HD, Deimling M, Kosling S, Hofer H, Spielmann RP (1996) Misleading changes of the signal intensity on opposed-phase MRI after injection of contrast medium. J Comput Assist Tomogr 20:173–178
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stadler, A., Schima, W., Ba-Ssalamah, A. et al. Artifacts in body MR imaging: their appearance and how to eliminate them. Eur Radiol 17, 1242–1255 (2007). https://doi.org/10.1007/s00330-006-0470-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0470-4