Abstract
The purpose of the study was to perform phantom studies to assess the impact of computed tomography (CT) system variability on quantitative measurements of contrast enhancement. A phantom containing tubes of contrast material at dilutions of 120, 1:35, 1:50, 1:100 and 1:200 arranged in air or water was imaged using 11 CT systems at 9 institutions. All systems had undergone routine calibration against air and water in accordance with the manufacturers’ recommendations. For a given tube voltage, the relationship between the iodine concentration and CT attenuation value on a single system varied by 17 to 24% over 46–48 weeks. The coefficients of variance for iodine calibration factors across different CT systems were 8.9% in air and 5.1% in water. Calibration of individual CT systems for iodine response is required to allow comparison of quantitative measurements of contrast enhancement across different institutions. Using the iodine calibration factor to express contrast enhancement as iodine concentration would facilitate the universal application of diagnostic enhancement thresholds, especially if the necessary calculations were performed by software installed on the CT console.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Quantification of contrast enhancement is increasingly advocated as a means to improve diagnostic accuracy during computed tomography (CT). Applications within thoracic imaging include the use of contrast enhancement measurements to characterise pulmonary nodules [1]. This technique has attracted interest as a means to evaluate pulmonary nodules detected during CT screening for lung cancer [2] and has been evaluated as a potential method for characterising and assessing treatment response in advanced bronchial cancers [3, 4]. Quantification of contrast enhancement has also been used to assess perfusion abnormalities associated with congenital pulmonary diseases [5]. Within the abdomen, quantification of hepatic enhancement during dual-phase spiral CT of the liver has been reported as a means of identifying patients at risk of subsequently developing hepatic metastases [6, 7]. Densitometry during contrast-enhanced CT has also been proposed for the characterisation of adrenal masses and diagnosis of lymph node metastases from gastric carcinoma [8–10].
The biological basis underlying these techniques is that tumour enhancement reflects tissue vascularity. In the case of tumour tissue, this premise is supported by reported correlations between contrast enhancement and histological measures of tumour microvessel density from lung and renal cancers [11–13]. Peak tumour enhancement can be converted to a physiological measure describing tumour perfusion normalised to average whole-body perfusion (the Standardised Perfusion Value) by using the patient’s weight, the dose of iodine injected and an iodine calibration factor that defines the linear relationship between the measured attenuation in (HU) and the concentration of contrast material [14]. However, most quantitative contrast-enhanced CT (QECT) techniques have adopted simple measures of enhancement expressed in HU with the assumption that, provided routine calibration of the CT system is undertaken, the relationship between measured attenuation and iodine concentration remains constant over time. Furthermore, when transferring the results of studies to other imaging sites, or when performing such techniques on a multi-center basis, it is often assumed that the increase in attenuation for a given concentration of contrast material is constant for all CT systems. This investigation tests the validity of such assumptions by performing a series of phantom studies to assess the short- and long-term variability of the relationship between iodine concentration and measured attenuation for a single CT system, and to assess this relationship across a range of CT systems.
Materials and methods
The study arose from a quality-control procedure performed as part of a multi-centre study that aimed to use quantitative contrast-enhanced CT for tumour response evaluation. Working within the constraints of the clinical demands on the CT systems involved, the study protocol was developed in an adaptive manner both in response to the results of assessments of short- and long-term variability on a single CT system and as results were obtained from multiple centres.
Phantom design
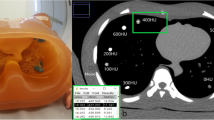
Figure 1 illustrates the phantom, which was designed by the authors and constructed from Perspex by Data Spectrum Corporation (Hillsborough, USA). The phantom body comprised a 30-cm cylinder within which five refillable tubes of 25-mm diameter were arranged in circular fashion. The sixth position was occupied by a Teflon plug to provide a quality-control standard of constant attenuation. It has been shown previously that the relationship between attenuation measured in HU and iodine concentration is dependent upon the amount of air within a particular body region [15]. Thus, the phantom body was designed to contain either air or water, in order to replicate QECT studies within the thorax (e.g., characterisation of lung nodules) or abdomen (e.g., measurement of hepatic enhancement), respectively. Several identical phantoms were produced and distributed to the various CT sites included in the study.
End plan view (a) and overall view (b) of the calibration phantom. Contrast material at various dilutions is introduced into cylinders of 25-mm diameter and 50-mm length located at positions 1 to 5 as follows: (1) 1:50, (2) 1:35, (3)1:20, (4) 1:200 and (5) 1:100. Three small venting plugs (V) allow release of air when filling the phantom with water. The phantom was placed on the CT table with the Teflon plug (T) down-most
Phantom protocol
The phantom studies were additional to the routine system calibrations performed in accordance with the manufacturer’s instructions to ensure stable attenuation values for air and water. Conventional contrast material of concentrations ranging from 300 to 370 mg iodine/ml was diluted in normal saline at ratios of 1:20, 1:35, 1:50, 1:100 and 1:200. The iodine concentration was calculated from the base concentration of contrast material and the volumes of contrast material and saline used, measured to the nearest 0.5 ml. The dilutions were chosen to give approximate iodine concentrations of between 1.5 and 15 mg/ml reflecting physiological concentrations found in tissues and vessels, respectively.
The tubes in the phantom were filled with the diluted contrast material solutions in a prescribed order, and the main phantom body was either left containing air or filled with water. The phantom was placed on the scanner table with the tubes of contrast material aligned along the Z-axis of the CT system. The position of the phantom and the height of the imaging table were adjusted so that the central long axis of the phantom was located at the centre-point of the CT gantry. The phantom orientation was constant with the Teflon plug lowermost. A single image acquisition comprising a 20-mm slab midway along the contrast material tubes was performed and post processed to either 5- or 6-mm-thick slices, depending upon the choices available on each CT system. The tube voltage was variable, but the tube current-time product was fixed at 150 mAs, consistent with image acquisition protocols in which QECT is used for perfusion imaging [16]. The acquisition field of view (FOV) was 500 mm. The reconstructed FOV was chosen by each site, but remained constant for repeated assessments at one site. Due to the variety of systems included in the study, it was not possible to standardise the reconstruction kernels, which were selected at the discretion of each participating centre to replicate clinical body CT. The reconstruction kernel was kept constant for repeated assessments at a single site.
On reconstructed images of the phantom, regions of interest (ROI) were placed over each tube containing contrast material. The ROI were constructed at each centre using the CT console or associated commercial work-station. A single operator was adopted for repeated studies at a single centre. Operators were instructed to make the ROI as large as possible whilst avoiding partial volume effects and air bubbles introduced when preparing the phantom. (Variability in the amount of air introduced across centres was reflected by the range of ROI sizes: 199–389 mm2, with a mean of 277 mm2.) Attenuation measurements from each tube were plotted against the corresponding iodine concentration. The gradient of a linear least-squares fit of the five points gave the iodine calibration factor.
Variation with tube voltage
Variation in the iodine calibration factor with tube voltage was assessed in a single day on one CT system (Lightspeed, GE Medical Systems, Milwaukee, WI) imaging the phantom, filled with air and filled with water, at 80 kVp, 100 kVp, 120 kVp and 140 kVp.
Short- and long- term stability
Variation in the iodine calibration factor over a 48-week period was assessed on one CT system (Lightspeed, GE Medical Systems, Milwaukee, WI). The X-ray tube was not changed during this period. Initial imaging at week 0 comprised measurements of the phantom, filled with air and filled with water, using tube voltages of 80, 100, 120 and 140 kVp. Imaging was repeated at week 2 using 120 kVp. Subsequent to analysis of the week 2 data, it was decided to reassess the system after a further 43 weeks, using 100 kVp. Following data analysis of this 45-week study, it was decided to confirm that no change in the concentration of contrast medium had occurred in the intervening period, either through evaporation or adsorption onto the surface of the phantom cylinders. Therefore, the phantom was re-filled with new dilutions of contrast media and imaged again using 100 kVp the following week (week 46) and 120 kVp at week 48. This re-dilution also allowed for an assessment of the magnitude of error potentially arising from preparation of the phantom. The FOV and reconstruction kernel were kept constant for the repeated measurements. Careful positioning of the phantom and adjustment of table height ensured that the position of the phantom was the same on each occasion with its central long axis located at the centre-point of the CT gantry.
CT systems
Variability in the iodine calibration factor between systems was determined by imaging the phantom on a range of CT systems from GE Medical Systems (Milwaukee, WI) and Siemens (Erlangen, Germany), including single-slice CT (one site), multi-slice CT (five sites) and combined Positron Emission Tomography/CT (PET/CT) systems (five sites). At one site, the phantom was imaged on two CT systems, with measurements made using air- and water-filled phantoms on both systems. On the remaining stand-alone CT systems, the phantom was imaged with water whilst on all PET/CT systems the phantom was imaged with air. The tube voltage was 120 kVp in all cases except on one combined PET/CT system, in which 120 kVp was not a selectable option. At this site, 130 kVp was selected.
Statistical analysis
Statistical analysis was performed using Excel software (Microsoft Corporation, Redmond, WA). The quality of each linear fit expressed as the correlation coefficient (r-value) and the 95% confidence limits for each iodine calibration factor were determined using standard regression analysis. Differences between linear fits were evaluated using the F-test with a probability value of 0.05 or less considered statistically significant. The variability of iodine calibration factors across CT systems was assessed by comparing each calibration curve to the median curve with overall variability expressed as the coefficient of variance (COV). The Siemens Biograph was excluded from statistical analysis because the phantom studies were performed at 130 kVp.
Results
Single-system variability
The results of the variability assessment of a single CT system are outlined in Table 1. The graphs plotting attenuation against iodine concentration gave a correlation coefficient for the linear fits of greater than 0.995 in all cases. Iodine calibration factors were significantly higher for lower tube voltages and studies in air compared to water (Fig. 2a). These differences in calibration factors with tube voltage were used as a reference against which to compare the magnitude of changes in iodine calibration with time and across systems. The assessment of short-term change between week 0 and week 2 demonstrated only a minor increase in calibration factor (1.0-2.2%), just reaching statistical significance for the water-filled phantom only. The short-term change between weeks 45 and 46, during which time new dilutions of contrast material were prepared, comprised greater increases in calibration factor of 3.5 to 5.8%. Although mean differences were statistically significant, there was considerable overlap between the 95% confidence limits of these calibration curves. Overall, short-term changes were considerably smaller than those produced by changing tube voltage by 20 kVp. Long-term changes were much greater at both tube voltages, and in air and water, with highly statistically significant increases in calibration factor of between 17 and 24% (P<0.0002) over 46–48 weeks (Fig. 2b). Long-term changes were similar in magnitude to the effect of reducing tube voltage by 20 kVp.
Graphs plotting attenuation against iodine concentration for water-filled phantoms. The correlation coefficient (r-value) is greater than 0.995 in each case. a: for multiple tube voltages in a single CT system, b: for a single CT system at 100 kVp showing statistically significant differences between the initial calibration curve and those measured at 45 weeks (P<0.001) and 46 weeks (P<0.0001) (including preparation of new solutions at 46 weeks) and c: for multiple CT systems showing the range of differences calibration factors amongst the seven CT systems evaluated. Statistically significant differences were found between the median and the highest (P<0.05) and lowest (P<0.0005) calibration curve
Variability between CT systems
The iodine calibration factors for the various CT systems assessed are given in Table 2. The graphs plotting attenuation against iodine concentration gave a correlation coefficient for the linear fits of greater than 0.995 for all systems. There was considerable variation in the iodine calibration factors amongst the different CT systems. The regression lines were significantly different from the median calibration for all but one system in air and all but two systems in water (Table 2) (P<0.01 to P<0.00005). Calibration factors ranged between 24.68 and 30.02 HU/mg iodine/ml (COV: 8.9 %) in air and between 19.74 and 23.26 HU/mg iodine/ml (COV: 5.1%) in water (Table 2 and Fig. 2c). The magnitude of these ranges approached the difference in calibration factor produced by a 20-kVp reduction in tube voltage for a single system. The single-slice CT system (HiSpeed, GE Medical Systems, Milwaukee, WI) gave the lowest values, whereas PET/CT systems gave higher values than stand-alone CT systems. The calibration factor of 30.79 HU/mg iodine/ml obtained with a tube voltage of 130 kVp on account of an inability to select 120 kVp on that system has been included for comparison. Had 120kVp been selectable, an even higher iodine calibration factor would be anticipated.
Discussion
The need for specific calibration protocols for CT densitometry of bone, and more recently lung, is well recognised [17]. We believe our study to be the first to consider the necessity of such calibrations for quantitative measures of contrast enhancement on CT. For CT studies without contrast material, the interaction between X-rays and soft tissues is mainly due to the Compton effect. However, after contrast enhancement, the photoelectric effect becomes important due to the 33-keV K-edge of the iodine included in the contrast material. Thus, a CT system’s response to soft-tissue density may be different to its response to iodinated contrast material. Indeed, a previous analysis has illustrated how CT measurements of attenuation from iodine are much more sensitive to changes in tube voltage than measurements from fat, soft tissue or bone [15]. (Even for bone, the likelihood of photoelectric interactions will be less than that for iodine despite the presence of the higher density elements of calcium and phosphorus, because the K-edge energies for these elements are relative low, i.e., <5 keV). Routine quality assurance for CT systems typically comprises calibration such that water and air return attenuation values of 0 HU and −1000 HU, respectively. Such calibration tests will not effectively evaluate the response of a CT system to changes in iodine concentration and hence contrast enhancement.
The variability in iodine calibration factors found in this study indicates that, despite routine calibration against air and water, a CT system’s response to iodine can change over time and different responses exist across CT systems. Such differences across CT systems specific to iodine concentration could arise due to variations in X-ray beam filtration resulting in X-ray spectra with different mean energies. An X-ray spectrum with a lower mean energy and/or a mean energy close to the inner (K) shell electronic-binding energy of iodine, i.e., 33.2 keV, would return a greater change in measured attenuation for a given concentration of iodine. The mean energy may also change over time due to wear in the anode. Indeed, in a previous study of long-term changes in air calibration for lung densitometry, a sudden shift in air calibration values was considered to be most likely due to a change in X-ray tube [17]. Routine quality assurance will correct for changes in mean energy as the anode wears but, being based on air and water, this re-calibration will be more appropriate for Compton interactions rather than the photoelectric interactions that are more common with contrast studies.
The increase in sensitivity to iodine at lower tube voltages (Fig. 2a) is well recognised [15, 18] and provides the rationale for selecting a lower tube voltage for QECT studies, as has been advocated for cerebral perfusion CT and CT cerebral angiography on the grounds of observed improvements in contrast enhancement outweighing any increase in image noise [19, 20]. This relationship can also provide a reference against which to compare the magnitude of changes in iodine calibration with time and across systems. The long-term changes on the single-system are approximately equivalent to a lowering of tube voltage by 20 kVp. A similar long-term drift in air calibration has been reported for CT densitometry of the lung [17], but the change in iodine calibration is of considerably greater magnitude, probably reflecting the greater prevalence of photoelectric interactions for iodine. The range of differences in calibration across systems is of similar magnitude, and the coefficients of variance are comparable to those previously reported for a multi-centre calibration against blood attenuation [17].
It is also useful to compare the magnitude of variability in iodine calibration factors to the impact that such variability in patient size could have upon QECT studies. Beam hardening will occur as X-ray photons pass through patients resulting in a higher mean photon energy, and hence a lower sensitivity to iodine, in larger patients. The phantom studies of Siegel et al. [18] demonstrated a 15% increase in sensitivity to iodine for a phantom of 8-cm diameter (equivalent to a neonate) relative to a 24-cm phantom (equivalent to an adult) as compared with our long-term increase in sensitivity of 17-24% and overall inter-system variability of 17.8–24.8%. Similarly, the studies of Huda et al. [15] suggest that an increase in patient weight of approximately 70 kg would be required to effect an increase in mean photon energy equivalent to a 20-kVp change in tube voltage. Thus, comparison of our results to previous phantom studies assessing the impact of patient size would suggest that both the degree of long-term variability on a single CT system and the variability between systems are likely to be of greater significance than beaming hardening effects resulting from differences in patient size.
Variations in patient size may also result in the selection of different table heights for individual patients undergoing CT. In addition, within a single patient, measurements of contrast enhancement may be made from structures at different positions relative to the centre-point of the CT gantry, e.g., the abdominal aorta and left lobe of the liver. These differences could potentially add to the variability of measurements of contrast enhancement in clinical practice. However, the degree of variability is likely to be small in view of the findings of Hopper et al. in which measured attenuation values were not significantly affected by a 20-cm y-direction change in the isocentre of a phantom containing multiple tissue equivalents [21]. Such effects were not evaluated by our study in which the position of the phantom and the height of the table were adjusted to align the central axis of the phantom with the centre-point of the CT gantry on each occasion.
One potential cause for differences in iodine calibration factors observed between CT systems is differences in the reconstruction kernel used at each site. Due to the inclusion of CT systems from different manufacturers, it was not possible to standardise the reconstruction kernel used. Nevertheless, the phantom studies of Groell et al. found that the reconstruction algorithm did not significantly affect absolute CT numbers obtained from tissue equivalents with attenuation values of 0HU and above [22]. Thus, the choice reconstruction kernel is likely to have little impact on the relative measurements of attenuation used to quantify contrast enhancement.
One limitation of our study is the possibility that the concentration of contrast medium in the phantom could vary across centres due to inaccuracies in dilution of contrast material or change over time within a single phantom examined repeatedly. The very high correlation coefficients for the linear fit of the plots of attenuation against iodine concentration suggest that the iodine solutions were prepared accurately across all sites. Inaccuracies in dilution of contrast material would most likely produce random errors and would thus be reflected by a poorer correlation coefficient. The likelihood of such inaccuracies producing a systematic error in the calibration factor was reduced by the use of five different dilutions. Furthermore, the change in calibration factor observed following re-dilution at a single site was small (3.5 to 5.8%) in comparison to the range of differences in calibration factor between systems (17.8 to 26.0%). Thus, it is more likely that the increase in calibration factor following preparation of new dilutions resulted from an increase in iodine concentration with time, possibly from evaporation of water. A phantom in which iodine is incorporated into solid material could overcome this problem.
A further limitation of the study has been the practical restrictions on the ability to perform more regular phantom studies along with the need to adapt the schedule as results became available. A greater frequency of repeated phantom studies on a greater number of systems would be required before firm guidelines for calibration can be established. It would also have been helpful to compare the repeated measurements of the iodine calibration factor on the single CT system with that systems’ stability for measurements of the attenuation of air and water. However, this was not possible because any variability in the attenuation values for water and air was corrected by the routine quality control procedures for which the magnitude of re-adjustment was not recorded. Furthermore, reliable measurements of air and water attenuation were not possible from the images obtained using the iodine calibration phantom due to beam-hardening effects resulting from the presence of contrast medium in the tubes. Our results indicate a need for manufacturers to develop and disseminate their own additional quality assurance protocols to allow users to evaluate a CT system’s response to iodine, including specifications concerning design of the phantom, alignment of the phantom in the gantry, exposure and field of view settings, bow-tie filter and frequency of evaluation. In the absence of manufacturers’ recommendations, it would be prudent to calibrate the CT system for iodine response on the same day as each quantitative contrast-enhanced study, particularly as statistically significant differences in calibration can develop within 2 weeks.
The potential for iodine calibration to differ between CT systems and to change over time needs to be considered as a potential source of error in research studies that use measurements of contrast enhancement, for example, when comparing the tissue enhancement achieved by particular contrast enhancement protocols or specific contrast media. Such studies should either include calibration of CT systems for iodine response or adopt randomisation that takes into account the X-ray tube age and CT systems used. Otherwise, it is possible that variations in iodine calibration could contribute to, or account for, apparent improvements in enhancement produced by a particular contrast enhancement protocol or contrast medium.
The degree of variability in iodine calibration factors with time and across systems also has implications for clinical practice where simple attenuation value thresholds may be used for diagnosis on contrast-enhanced CT, for instance, in the evaluation of indeterminate pulmonary nodules [1]. Our results indicate that such diagnostic thresholds cannot be assumed to remain constant over time and those derived on one CT system cannot be transferred to another system without knowledge of iodine calibration factors for each system at a particular time. For example, Swenson et al. proposed an enhancement threshold of 15 HU for diagnosis of malignancy within a pulmonary nodule [1]. Yet, based on the iodine calibration factors observed in air in our study, 15 HU of enhancement on one CT system could be equivalent to 17.6 HU on the same system 45 weeks later, or to 18.7 HU on another system. Similarly for hepatic enhancement, Sheafor et al. adopted a threshold of 105 HU to identify those patients with breast cancer subsequently developing overt liver metastases [7]. Based on our phantom measurements in water, enhancement by 105 HU on one CT system could be equivalent to 125.5 HU on the same system 45 weeks later, or to up to 123.7 HU on other systems. Thus, adopting a universal threshold enhancement value for diagnosis without system calibration creates the potential for misclassification of a patient’s diagnosis.
Rather than measure a change in attenuation value in a given structure after administration of contrast material, some quantitative CT techniques adopt a single densitometric measurement following contrast enhancement. In such cases, the attenuation value obtained will result from a combination of baseline attenuation values and changes in attenuation due to accumulation of contrast material. The fact that baseline attenuation values may also vary with the CT system has been shown by Stadler et al., who found that adrenal lesions with a mean CT number of 45.1 HU could vary in attenuation by up to 6.5 HU when examined on other CT systems [23]. Such inconsistencies in baseline values and also the variability in iodine calibration factors affect single CT attenuation values obtained after contrast enhancement. However, quantitative techniques that compare contrast enhancement in one structure to another (e.g., ratios between the target lesion and normal tissue or blood vessels), including perfusion CT techniques, will be less affected because the iodine calibration factor will impact measurements from both the target and reference regions, and thus tend to cancel out. Nevertheless, this benefit may be off-set to some extent by the increased complexity of such techniques and therefore the potential for other sources of error.
Measurement of contrast enhancement as a diagnostic tool is attractive on account of its simplicity. However, the results of this study indicate that calibration of individual CT systems is required to allow for comparison of quantitative measurements of contrast enhancement over time and across different institutions. Using the calibration factor to express contrast enhancement as iodine concentration (expressed in mg iodine/ml) or the Standardised Enhancement Value [14] would facilitate the universal application of diagnostic enhancement thresholds, especially if the necessary calculations were performed by software installed on the CT console.
References
Swensen SJ, Viggiano RW, Midthun DE, Muller NL, Sherrick A, Yamashita K, Naidich DP, Patz EF, Hartman TE, Muhm JR, Weaver AL (2000) Lung nodule enhancement at CT: multicenter study. Radiology 214:73–80
Pastorino U, Bellomi M, Landoni C, De Fiori E, Arnaldi P, Picchio M, Pelosi G, Boyle P, Fazio F (2003) Early lung-cancer detection with spiral CT and positron emission tomography in heavy smokers: 2-year results. Lancet 362(9384):593–597, Aug 23
Kiessling F, Boese J, Corvinus C, Ederle JR, Zuna I et al (2004) Perfusion CT in patients with advanced bronchial carcinomas: a novel chance for characterisation and treatment monitoring? Eur Radiol 14:1226–1233
Miles KA, Griffiths MR, Keith CJ (2005) Blood flow-metabolic relationships are dependent on tumour size in non-small cell lung cancer: a study using quantitative contrast enhanced computer tomography and positron emission tomography. Eur J Nucl Med Mol Imaging 33:22–28
Boll DT, Lewin JS, Young P, Siwik ES, Gilkeson RC (2005) Perfusion abnormalities in congenital and neoplastic pulmonary disease: comparison of MR perfusion and multislice CT imaging. Eur Radiol 15:1978–1986
Platt JF, Francis IR, Ellis JH, Reige KA (1997) Liver metastases: Early detection based on abnormal contrast material enhancement at dual-phase helical CT. Radiology 205:49–53
Sheafor DH, Killius JS, Paulson EK, DeLong DM, Foti AM, Nelson RC (2000) Hepatic parenchymal enhancement during triple-phase helical CT: Can it be used to predict which patients with breast cancer will develop hepatic metastases? Radiology 214:875–880
Szolar DH, Kammerhuber F (1997) Quantitative CT evaluation of adrenal gland masses: a step forward in the differentiation between adenomas and nonadenomas? Radiology 202(2):517–521, Feb
Boland GW, Hahn PF, Pena C, Mueller PR (1997) Adrenal masses: characterization with delayed contrast-enhanced CT. Radiology 202(3):693–696, Mar
Fukuya T, Honda H, Hayashi T, Kaneko K, Tateshi Y, Ro T, Maehara Y, Tanaka M, Tsuneyoshi M, Masuda K (1995) Lymph-node metastases: efficacy of detection with helical CT in patients with gastric cancer. Radiology 197:705–711
Swensen SJ, Brown LR, Colby TV, Weaver AL, Midthun DE (1996) Lung nodule enhancement at CT: prospective findings. Radiology 201:447–455
Tateishi U, Nishihara H, Watanabe S, Morikawa T, Abe K, Miyasaka K (2001) Tumor angiogenesis and dynamic CT in lung adenocarcinoma: radiologic-pathologic correlation. J Comput Assist Tomogr 25:23–27
Jinzaki M, Tanimoto A, Mukai M, Ikeda E, Kobayashi S, Yuasa Y, Narimatsu Y, Murai M (2000) Double-phase helical CT of small renal parenchymal neoplasms: correlation with pathologic findings and tumor angiogenesis. J Comput Assist Tomogr 24:835–842
Miles KA, Griffiths MR, Fuentes MA (2001) Standardized perfusion value: universal CT contrast enhancement scale that correlates with FDG PET in lung nodules. Radiology 220:548–553
Huda W, Scalzetti EM, Levin G (2000) Technique factors and image quality as functions of patient weight at abdominal CT. Radiology 217:430–435
Miles KA (2003) Perfusion CT for the assessment of tumour vascularity: which protocol? Brit J Radiol 76 Spec No. 1:S36–S42
Parr DG, Stoel BC, Stolk J, Nightingale PG, Stockley RA (2004) Influence of calibration on densitometric studies of emphysema progression using computed tomography. Am J Respir Crit Care Med 170:883–890
Siegel MJ, Schmidt B, Bradley D, Suess C, Hildebolt C (2004)Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology 233:515–522
Wintermark M, Maeder P, Verdun FR, Thiran JP, Valley JF, Schnyder P, Meuli R (2000) Using 80 kVp versus 120 kVp in perfusion CT measurement of regional cerebral blood flow. Am J Neuroradiol 21:1881–1884
Bahner ML, Bengel A, Brix G, Zuna I, Kauczor HU, Delorme S (2005) Improved vascular opacification in cerebral computed tomography angiography with 80 kVp. Invest Radiol 40:229–234
Hopper KD, Gouldy CA, Kasales CJ, TenHave TR, Fisher AL (1997) The effect of helical CT on X-ray attenuation. J Comput Assist Tomogr 21:152–155
Groell R, Rienmueller R, Schaffler GJ, Portugaller HR, Graif E, Willfurth P (2000) CT number variations due to different image acquisition and reconstruction parameters: a thorax phantom study. Comput Med Imaging Graph 24:53–58
Stadler A, Schima W, Prager G, Homolka P, Heinz G, Saini S, Eisenhuber E, Niederle B (2004) CT density measurements for characterization of adrenal tumors ex vivo: variability among three CT scanners. Am J Roentgenol 182:671–675
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miles, K.A., Young, H., Chica, S.L. et al. Quantitative contrast-enhanced computed tomography: is there a need for system calibration?. Eur Radiol 17, 919–926 (2007). https://doi.org/10.1007/s00330-006-0424-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0424-x